David Colquhoun
This is a web version of a review of Peter Gotzsche’s book. It appeared in the April 2014 Healthwatch Newsletter. Read the whole newsletter. It has lots of good stuff. Their newsletters are here. Healthwatch has been exposing quackery since 1989. Their very first newsletter is still relevant.
|
Most new drugs and vaccines are developed by the pharmaceutical industry. The industry has produced huge benefits for mankind. But since the Thatcherite era it has come to be dominated by marketing people who appear to lack any conscience. That’s what gave rise to the Alltrials movement. It was founded in January 2013 with the aim of ensuring that all past and present clinical trials are registered before they start and that and their results are published The industry has been dragged, kicking and screaming, towards a new era of transparency, with two of the worst offenders, GSK and Roche, now promising to release all data. Let’s hope this is the beginning of real open science. |

|
This version is not quite identical with the published version in which several changes were enforced by Healthwatch’s legal adviser. They weren’t very big changes, but here is the original.
Deadly Medicines and Organised Crime
By Peter Gøtzsche, reviewed by David Colquhoun
Published by Radcliffe Publishing Ltd on 1 August 2013. RRP £24.99 (320 pages, paperback)
ISBN-10: 1846198844 ISBN-13: 978-1846198847
As someone who has spent a lifetime teaching pharmacology, this book is a bitter pill to swallow. It makes Goldacre’s Bad Pharma seem quite mild.
In fairness, the bits of pharmacology that I’ve taught concern mostly drugs that do work quite well. Things like neuromuscular blocking agents, local anaesthetics, general anaesthetics, anticoagulants, cardiac glycosides and thyroid drugs all do pretty much what is says on the label.
Peter Gøtzsche is nothing if not evidence man. He directs the Nordic Cochrane group, and he talks straight. His book is about drugs that don’t work as advertised. There is no doubt whatsoever that the pharmaceutical industry has behaved very badly indeed in the last couple of decades. You don’t have to take my word for it, nor Peter Gotzche’s, nor Ben Goldacre’s. They have told us about it themselves. Not voluntarily of course, but in internal emails that have been revealed during court proceedings, and from whistleblowers.
Peter Rost was vice president marketing for the huge pharmaceutical company, Pfizer, until he was fired after the company failed to listen to his complaints about illegal marketing of human growth hormone as an anti-ageing drug. After this he said:
“It is scary how many similarities there are between this industry and the mob. The mob makes obscene amounts of money, as does this industry. The side effects of organized crime are killings and deaths, and the side effects are the same in this industry. The mob bribes politicians and others, and so does the drug industry … “
The pharmaceutical industry is the biggest defrauder of the US federal government under the False Claims Act. Roche led a cartel that, according to the US Justice Department’s antitrust division, was the most pervasive and harmful criminal antitrust conspiracy ever uncovered. Multibillion dollar fines have been levied on all of the big companies (almost all in the USA, other countries have been supine), though the company’s profits are so huge they are regarded as marketing expenses.
It’s estimated that adverse effects of drugs kill more people than anything but cancer and heart disease, roughly half as many as cigarettes. This horrifying statistic is announced at the beginning of the book, though you have to wait until Chapter 21 to find the data. I’d have liked to see a more critical discussion of the problems of causality in deciding why someone died, which are just as big as those in deciding why somebody recovered. Nevertheless, nobody seems to deny that the numbers who are killed by their treatments are alarmingly high.
Gøtzsche’s book deals with a wide range of drugs that don’t do what it says on the label, but which have made fortunes because of corruption of the scientific process. These include non-steroidal anti-inflammatory drugs (NSAIDs), an area described as “a horror story filled with extravagant claims, bending of the rules, regulatory inaction, . . .”. Other areas where there has been major misbehaviour include diabetes (Avandia), and the great Tamiflu scandal. and the great Tamiflu scandal. It took five years of pressure before Roche released the hidden data about Tamiflu trials. It barely works. Goldacre commented “government’s Tamiflu stockpile wouldn’t have done us much good in the event of a flu epidemic”
But the worst single area is psychiatry.
Two of the chapters in the book deal with psychiatry. Nobody has the slightest idea how the brain works (don’t believe the neuroscience hype) or what causes depression or psychosis. Treatments are no more than guesses and none of them seems to work very well.
The problems with the SSRI antidepressant, paroxetine (Seroxat in UK, Paxil in USA) were brought to public attention, not by a regulator, but by a BBC Panorama television programme. The programme revealed that a PR company, which worked for GSK, had written
"Originally we had planned to do extensive media relations surrounding this study until we actually viewed the results. Essentially the study did not really show it was effective in treating adolescent depression, which is not something we want to publicise."
This referred to the now-notorious study 329. It was intended to show that paroxetine should be recommended for adolescent depression. The paper that eventually appeared in 2001 grossly misrepresented the results. The conclusions stated “Paroxetine is generally well tolerated and effective for major depression in adolescents”, despite the fact that GSK already knew this wasn’t true. The first author of this paper was Martin Keller, chair of psychiatry at Brown University, RI, with 21 others.
But the paper wasn’t written by them, but by ghost authors working for GSK. Keller admitted that he hadn’t checked the results properly.
That’s not all. Gøtzsche comments thus.
“Keller is some character. He double- billed his travel expenses, which were reimbursed both by his university and the drug sponsor. Further, the Massachusetts Department of Mental Health had paid Brown’s psychiatry department, which Keller chaired, hundreds of thousands of dollars to fund research that wasn’t being conducted. Keller himself received hundreds of thousands of dollars from drug companies every year that he didn’t disclose.”
His department received $50 million in research funding. Brown University has never admitted that there was a problem. It still boasts about this infamous paper
The extent of corruption at Brown University rivals the mob.
The infamous case of Richard Eastell at Sheffield university is no better. He admitted in print to lying about who’d seen the data. The university did nothing but fire the whistleblower.
Another trial, study 377, also showed that paroxetine didn’t work. GSK suppressed it.
“There are no plans to publish data from Study 377” (Seroxat/Paxil Adolescent Depression. Position piece on the phase III clinical studies. GlaxoSmithKline document. 1998 Oct.)
Where were the regulatory agencies during all this? The MHRA did ban use of paroxetine in adolescents in 2003, but their full investigation didn’t report until 2008. It came to much the same conclusions as the TV programme six years earlier about the deceit. But despite that, no prosecution was brought. GSK got away with a deferential rap on the knuckles.
Fiona Godlee (editor of the BMJ, which had turned down the paper) commented
“We shouldn’t have to rely on investigative journalists to ask the difficult questions”
Now we can add bloggers to that list of people who ask difficult questions. The scam operated by the University of Wales, in ‘validating’ external degrees was revealed by my blog and by BBC TV Wales. The Quality Assurance Agency came in only at the last moment. Regulators regularly fail to regulate.
|
Despite all this, the current MHRA learning module on SSRIs contains little hint that SSRIs simply don’t work for mild or moderate depression. Neither does the current NICE guidance. Some psychiatrists still think they do work, despite there being so many negative trials. |
 |
The psychiatrists’ narrative goes like this. You don’t expect to see improvements for many weeks (despite the fact that serotonin uptake is stopped immediately). You may get worse before you get better. And if the first sort of pill doesn’t work, try another one. That’s pretty much identical with what a homeopath will tell you. The odds are that its meaning is, wait a while and you’ll get better eventually, regardless of treatment.
It’s common to be told that they must work because when you stop taking them, you get worse. But, perhaps more likely, when you stop taking them you get withdrawal symptoms, because the treatment itself caused a chemical imbalance. Gøtzsche makes a strong case that most psychiatric drugs do more harm than good, if taken for any length of time. Marcia Angell makes a similar case in The Illusions of Psychiatry.
Gøtzsche will inevitably be accused of exaggerating. Chapter 14 ends thus.
“Merck stated only 6 months before it withdrew Vioxx that ‘MSD is fully committed to the highest standards of scientific integrity, ethics, and protection of patient’s wellbeing in our research. We have a tradition of partnership with leaders in the academic research community. Great. Let’s have some more of such ethical partnerships. They often kill our patients while everyone else prospers.
Perhaps Hells Angels should consider something similar in their PR: We are fully committed to the highest standards of integrity, ethics and protection of citizens’ well- being when we push narcotic drugs. We have a tradition of partnership with leaders in the police force”.
But the evidence is there. The book has over 900 references. Much of the wrongdoing has been laid bare by legal actions. I grieve for the state of my subject.
The wrongdoing by pharma is a disgrace.
The corruption of universities and academics is even worse, because they are meant to be our defence against commercial corruption.
All one can do is to take consolation from the fact that academics, like Gøtzsche and Goldacre, and a host of bloggers, are the people who are revealing what’s wrong. As a writer for the business magazine, Fortune, said
“For better or worse, the drug industry is going to have to get used to Dr. Peter Rost – and others like him.”
At a recent meeting I said that it was tragic that medicine, the caring profession, was also the most corrupt (though I’m happy to admit that other jobs might be as bad if offered as much money).
At present there is little transparency. There is no way that I can tell whether my doctor is taking money from pharma, data are still hidden from public scrutiny by regulatory agencies (which are stuffed with people who take pharma money) as well as by companies. Governments regard business as more important than patients. In the UK, the Government continued promotion of the fake bomb detector for many years after they’d been told it was fake. Their attitude to fake medicines is not much different. Business is business, right?
One side effect of the horrific corruption is that it’s used as a stick by the alternative medicine industry. That’s silly of them, because their business is more or less 100% mendacious marketing of ineffective treatments. At least half of pharma products really do work.
Fines are useless. Nothing will change until a few CEOs, a few professors and a few vice-chancellors spend time in jail for corruption.
Read this book. Get angry. Do something.
Follow-up
This post is now a bit out of date: there is a summary of my more recent efforts (papers, videos and pop stuff) can be found on Prof Sivilotti’s OneMol pages.
What follows is a simplified version of part of a paper that appeared as a preprint on arXiv in July. It appeared as a peer-reviewed paper on 19th November 2014, in the new Royal Society Open Science journal. If you find anything wrong, or obscure, please email me. Be vicious.
There is also a simplified version, given as a talk on Youtube..
It’s a follow-up to my very first paper, which was written in 1959 – 60, while I was a fourth year undergraduate(the history is at a recent blog). I hope this one is better.
‘”. . . before anything was known of Lydgate’s skill, the judgements on it had naturally been divided, depending on a sense of likelihood, situated perhaps in the pit of the stomach, or in the pineal gland, and differing in its verdicts, but not less valuable as a guide in the total deficit of evidence” ‘George Eliot (Middlemarch, Chap. 45)
“The standard approach in teaching, of stressing the formal definition of a p-value while warning against its misinterpretation, has simply been an abysmal failure” Sellke et al. (2001) `The American Statistician’ (55), 62–71
The last post was about screening. It showed that most screening tests are useless, in the sense that a large proportion of people who test positive do not have the condition. This proportion can be called the false discovery rate. You think you’ve discovered the condition, but you were wrong.
Very similar ideas can be applied to tests of significance. If you read almost any scientific paper you’ll find statements like “this result was statistically significant (P = 0.047)”. Tests of significance were designed to prevent you from making a fool of yourself by claiming to have discovered something, when in fact all you are seeing is the effect of random chance. In this case we define the false discovery rate as the probability that, when a test comes out as ‘statistically significant’, there is actually no real effect.
You can also make a fool of yourself by failing to detect a real effect, but this is less harmful to your reputation.
It’s very common for people to claim that an effect is real, not just chance, whenever the test produces a P value of less than 0.05, and when asked, it’s common for people to think that this procedure gives them a chance of 1 in 20 of making a fool of themselves. Leaving aside that this seems rather too often to make a fool of yourself, this interpretation is simply wrong.
The purpose of this post is to justify the following proposition.
|
If you observe a P value close to 0.05, your false discovery rate will not be 5%. It will be at least 30% and it could easily be 80% for small studies.
|
This makes slightly less startling the assertion in John Ioannidis’ (2005) article, Why Most Published Research Findings Are False. That paper caused quite a stir. It’s a serious allegation. In fairness, the title was a bit misleading. Ioannidis wasn’t talking about all science. But it has become apparent that an alarming number of published works in some fields can’t be reproduced by others. The worst offenders seem to be clinical trials, experimental psychology and neuroscience, some parts of cancer research and some attempts to associate genes with disease (genome-wide association studies). Of course the self-correcting nature of science means that the false discoveries get revealed as such in the end, but it would obviously be a lot better if false results weren’t published in the first place.
How can tests of significance be so misleading?
Tests of statistical significance have been around for well over 100 years now. One of the most widely used is Student’s t test. It was published in 1908. ‘Student’ was the pseudonym for William Sealy Gosset, who worked at the Guinness brewery in Dublin. He visited Karl Pearson’s statistics department at UCL because he wanted statistical methods that were valid for testing small samples. The example that he used in his paper was based on data from Arthur Cushny, the first holder of the chair of pharmacology at UCL (subsequently named the A.J. Clark chair, after its second holder)
The outcome of a significance test is a probability, referred to as a P value. First, let’s be clear what the P value means. It will be simpler to do that in the context of a particular example. Suppose we wish to know whether treatment A is better (or worse) than treatment B (A might be a new drug, and B a placebo). We’d take a group of people and allocate each person to take either A or B and the choice would be random. Each person would have an equal chance of getting A or B. We’d observe the responses and then take the average (mean) response for those who had received A and the average for those who had received B. If the treatment (A) was no better than placebo (B), the difference between means should be zero on average. But the variability of the responses means that the observed difference will never be exactly zero. So how big does it have to be before you discount the possibility that random chance is all you were seeing. You do the test and get a P value. Given the ubiquity of P values in scientific papers, it’s surprisingly rare for people to be able to give an accurate definition. Here it is.
|
The P value is the probability that you would find a difference as big as that observed, or a still bigger value, if in fact A and B were identical.
|
If this probability is low enough, the conclusion would be that it’s unlikely that the observed difference (or a still bigger one) would have occurred if A and B were identical, so we conclude that they are not identical, i.e. that there is a genuine difference between treatment and placebo.
This is the classical way to avoid making a fool of yourself by claiming to have made a discovery when you haven’t. It was developed and popularised by the greatest statistician of the 20th century, Ronald Fisher, during the 1920s and 1930s. It does exactly what it says on the tin. It sounds entirely plausible.
What could possibly go wrong?
Another way to look at significance tests
One way to look at the problem is to notice that the classical approach considers only what would happen if there were no real effect or, as a statistician would put it, what would happen if the null hypothesis were true. But there isn’t much point in knowing that an event is unlikely when the null hypothesis is true unless you know how likely it is when there is a real effect.
We can look at the problem a bit more realistically by means of a tree diagram, very like that used to analyse screening tests, in the previous post.
In order to do this, we need to specify a couple more things.
First we need to specify the power of the significance test. This is the probability that we’ll detect a difference when there really is one. By ‘detect a difference’ we mean that the test comes out with P < 0.05 (or whatever level we set). So it’s analogous with the sensitivity of a screening test. In order to calculate sample sizes, it’s common to set the power to 0.8 (obviously 0.99 would be better, but that would often require impracticably large samples).
The second thing that we need to specify is a bit trickier, the proportion of tests that we do in which there is a real difference. This is analogous to the prevalence of the disease in the population being tested in the screening example. There is nothing mysterious about it. It’s an ordinary probability that can be thought of as a long-term frequency. But it is a probability that’s much harder to get a value for than the prevalence of a disease.
If we were testing a series of 30C homeopathic pills, all of the pills, regardless of what it says on the label, would be identical with the placebo controls so the prevalence of genuine effects, call it P(real), would be zero. So every positive test would be a false positive: the false discovery rate would be 100%. But in real science we want to predict the false discovery rate in less extreme cases.
Suppose, for example, that we test a large number of candidate drugs. Life being what it is, most of them will be inactive, but some will have a genuine effect. In this example we’d be lucky if 10% had a real effect, i.e. were really more effective than the inactive controls. So in this case we’d set the prevalence to P(real) = 0.1.
We can now construct a tree diagram exactly as we did for screening tests.
Suppose that we do 1000 tests. In 90% of them (900 tests) there is no real effect: the null hypothesis is true. If we use P = 0.05 as a criterion for significance then, according to the classical theory, 5% of them (45 tests) will give false positives, as shown in the lower limb of the tree diagram. If the power of the test was 0.8 then we’ll detect 80% of the real differences so there will be 80 correct positive tests.
The total number of positive tests is 45 + 80 = 125, and the proportion of these that are false positives is 45/125 = 36 percent. Our false discovery rate is far bigger than the 5% that many people still believe they are attaining.
In contrast, 98% of negative tests are right (though this is less surprising because 90% of experiments really have no effect).
The equation
You can skip this section without losing much.
As in the case of screening tests, this result can be calculated from an equation. The same equation works if we substitute power for sensitivity, P(real) for prevalence, and siglev for (1 – specificity) where siglev is the cut off value for “significance”, 0.05 in our examples.
The false discovery rate (the probability that, if a “signifcant” result is found, there is actually no real effect) is given by
\[FDR = \frac{siglev\left(1-P(real)\right)}{power.P(real) + siglev\left(1-P(real)\right) }\; \]
In the example above, power = 0.8, siglev = 0.05 and P(real) = 0.1, so the false discovery rate is
\[\frac{0.05 (1-0.1)}{0.8 \times 0.1 + 0.05 (1-0.1) }\; = 0.36 \]
So 36% of “significant” results are wrong, as found in the tree diagram.
Some subtleties
The argument just presented should be quite enough to convince you that significance testing, as commonly practised, will lead to disastrous numbers of false positives. But the basis of how to make inferences is still a matter that’s the subject of intense controversy among statisticians, so what is an experimenter to do?
It is difficult to give a consensus of informed opinion because, although there is much informed opinion, there is rather little consensus. A personal view follows. Colquhoun (1970), Lectures on Biostatistics, pp 94-95.
This is almost as true now as it was when I wrote it in the late 1960s, but there are some areas of broad agreement.
There are two subtleties that cause the approach outlined above to be a bit contentious. The first lies in the problem of deciding the prevalence, P(real). You may have noticed that if the frequency of real effects were 50% rather than 10%, the approach shown in the diagram would give a false discovery rate of only 6%, little different from the 5% that’s embedded in the consciousness of most experimentalists.
But this doesn’t get us off the hook, for two reasons. For a start, there is no reason at all to think that there will be a real effect there in half of the tests that we do. Of course if P(real) were even bigger than 0.5, the false discovery rate would fall to zero, because when P(real) = 1, all effects are real and therefore all positive tests are correct.
There is also a more subtle point. If we are trying to interpret the result of a single test that comes out with a P value of, say, P = 0.047, then we should not be looking at all significant results (those with P < 0.05), but only at those tests that come out with P = 0.047. This can be done quite easily by simulating a long series of t tests, and then restricting attention to those that come out with P values between, say, 0.045 and 0.05. When this is done we find that the false discovery rate is at least 26%. That’s for the best possible case where the sample size is good (power of the test is 0.8) and the prevalence of real effects is 0.5. When, as in the tree diagram, the prevalence of real effects is 0.1, the false discovery rate is 76%. That’s enough to justify Ioannidis’ statement that most published results are wrong.
One problem with all of the approaches mentioned above was the need to guess at the prevalence of real effects (that’s what a Bayesian would call the prior probability). James Berger and colleagues (Sellke et al., 2001) have proposed a way round this problem by looking at all possible prior distributions and so coming up with a minimum false discovery rate that holds universally. The conclusions are much the same as before. If you claim to have found an effects whenever you observe a P value just less than 0.05, you will come to the wrong conclusion in at least 29% of the tests that you do. If, on the other hand, you use P = 0.001, you’ll be wrong in only 1.8% of cases. Valen Johnson (2013) has reached similar conclusions by a related argument.
A three-sigma rule
As an alternative to insisting on P < 0.001 before claiming you’ve discovered something, you could use a 3-sigma rule. In other words, insist that an effect is at least three standard deviations away from the control value (as opposed to the two standard deviations that correspond to P = 0.05).
The three sigma rule means using P= 0.0027 as your cut off. This, according to Berger’s rule, implies a false discovery rate of (at least) 4.5%, not far from the value that many people mistakenly think is achieved by using P = 0.05 as a criterion.
Particle physicists go a lot further than this. They use a 5-sigma rule before announcing a new discovery. That corresponds to a P value of less than one in a million (0.57 x 10−6). According to Berger’s rule this corresponds to a false discovery rate of (at least) around 20 per million. Of course their experiments can’t be randomised usually, so it’s as well to be on the safe side.
Underpowered experiments
All of the problems discussed so far concern the near-ideal case. They assume that your sample size is big enough (power about 0.8 say) and that all of the assumptions made in the test are true, that there is no bias or cheating and that no negative results are suppressed. The real-life problems can only be worse. One way in which it is often worse is that sample sizes are too small, so the statistical power of the tests is low.
The problem of underpowered experiments has been known since 1962, but it has been ignored. Recently it has come back into prominence, thanks in large part to John Ioannidis and the crisis of reproducibility in some areas of science. Button et al. (2013) said
“We optimistically estimate the median statistical power of studies in the neuroscience field to be between about 8% and about 31%”
This is disastrously low. Running simulated t tests shows that with a power of 0.2, not only do you have only a 20% chance of detecting a real effect, but that when you do manage to get a “significant” result there is a 76% chance that it’s a false discovery.
And furthermore, when you do find a “significant” result, the size of the effect will be over-estimated by a factor of nearly 2. This “inflation effect” happens because only those experiments that happen, by chance, to have a larger-than-average effect size will be deemed to be “significant”.
What should you do to prevent making a fool of yourself?
The simulated t test results, and some other subtleties, will be described in a paper, and/or in a future post. But I hope that enough has been said here to convince you that there are real problems in the sort of statistical tests that are universal in the literature.
The blame for the crisis in reproducibility has several sources.
One of them is the self-imposed publish-or-perish culture, which values quantity over quality, and which has done enormous harm to science.
The mis-assessment of individuals by silly bibliometric methods has contributed to this harm. Of all the proposed methods, altmetrics is demonstrably the most idiotic. Yet some vice-chancellors have failed to understand that.
Another is scientists’ own vanity, which leads to the PR department issuing disgracefully hyped up press releases.
In some cases, the abstract of a paper states that a discovery has been made when the data say the opposite. This sort of spin is common in the quack world. Yet referees and editors get taken in by the ruse (e.g see this study of acupuncture).
The reluctance of many journals (and many authors) to publish negative results biases the whole literature in favour of positive results. This is so disastrous in clinical work that a pressure group has been started; altrials.net “All Trials Registered | All Results Reported”.
Yet another problem is that it has become very hard to get grants without putting your name on publications to which you have made little contribution. This leads to exploitation of young scientists by older ones (who fail to set a good example). Peter Lawrence has set out the problems.
And, most pertinent to this post, a widespread failure to understand properly what a significance test means must contribute to the problem. Young scientists are under such intense pressure to publish, they have no time to learn about statistics.
Here are some things that can be done.
- Notice that all statistical tests of significance assume that the treatments have been allocated at random. This means that application of significance tests to observational data, e.g. epidemiological surveys of diet and health, is not valid. You can’t expect to get the right answer. The easiest way to understand this assumption is to think about randomisation tests (which should have replaced t tests decades ago, but which are still rare). There is a simple introduction in Lectures on Biostatistics (chapters 8 and 9). There are other assumptions too, about the distribution of observations, independence of measurements), but randomisation is the most important.
- Never, ever, use the word “significant” in a paper. It is arbitrary, and, as we have seen, deeply misleading. Still less should you use “almost significant”, “tendency to significant” or any of the hundreds of similar circumlocutions listed by Matthew Hankins on his Still not Significant blog.
- If you do a significance test, just state the P value and give the effect size and confidence intervals (but be aware that this is just another way of expressing the P value approach: it tells you nothing whatsoever about the false discovery rate).
- Observation of a P value close to 0.05 means nothing more than ‘worth another look’. In practice, one’s attitude will depend on weighing the losses that ensue if you miss a real effect against the loss to your reputation if you claim falsely to have made a discovery.
- If you want to avoid making a fool of yourself most of the time, don’t regard anything bigger than P < 0.001 as a demonstration that you’ve discovered something. Or, slightly less stringently, use a three-sigma rule.
Despite the gigantic contributions that Ronald Fisher made to statistics, his work has been widely misinterpreted. We must, however reluctantly, concede that there is some truth in the comment made by an astute journalist:
“The plain fact is that 70 years ago Ronald Fisher gave scientists a mathematical machine for turning baloney into breakthroughs, and °flukes into funding. It is time to pull the plug“. Robert Matthews Sunday Telegraph, 13 September 1998.
There is now a video on YouTube that attempts to explain explain simply the essential ideas. The video has now been updated. The new version has better volume and it used term ‘false positive risk’, rather than the earlier term ‘false discovery rate’, to avoid confusion with the use of the latter term in the context of multiple comparisons.
The false positive risk: a proposal concerning what to do about p-values (version 2)
Follow-up
31 March 2014 I liked Stephen Senn’s first comment on twitter (the twitter stream is storified here). He said ” I may have to write a paper ‘You may believe you are NOT a Bayesian but you’re wrong'”. I maintain that the analysis here is merely an exercise in conditional probabilities. It bears a formal similarity to a Bayesian argument, but is free of more contentious parts of the Bayesian approach. This is amplified in a comment, below.
4 April 2014
I just noticed that my first boss, Heinz Otto Schild.in his 1942 paper about the statistical analysis of 2+2 dose biological assays (written while he was interned at the beginning of the war) chose to use 99% confidence limits, rather than the now universal 95% limits. The later are more flattering to your results, but Schild was more concerned with precision than self-promotion.
This post is about why screening healthy people is generally a bad idea. It is the first in a series of posts on the hazards of statistics.
There is nothing new about it: Graeme Archer recently wrote a similar piece in his Telegraph blog. But the problems are consistently ignored by people who suggest screening tests, and by journals that promote their work. It seems that it can’t be said often enough.
The reason is that most screening tests give a large number of false positives. If your test comes out positive, your chance of actually having the disease is almost always quite small. False positive tests cause alarm, and they may do real harm, when they lead to unnecessary surgery or other treatments.
Tests for Alzheimer’s disease have been in the news a lot recently. They make a good example, if only because it’s hard to see what good comes of being told early on that you might get Alzheimer’s later when there are no good treatments that can help with that news. But worse still, the news you are given is usually wrong anyway.
Consider a recent paper that described a test for "mild cognitive impairment" (MCI), a condition that may, but often isn’t, a precursor of Alzheimer’s disease. The 15-minute test was published in the Journal of Neuropsychiatry and Clinical Neurosciences by Scharre et al (2014). The test sounded pretty good. It had a specificity of 95% and a sensitivity of 80%.
Specificity (95%) means that 95% of people who are healthy will get the correct diagnosis: the test will be negative.
Sensitivity (80%) means that 80% of people who have MCI will get the correct diagnosis: the test will be positive.
To understand the implication of these numbers we need to know also the prevalence of MCI in the population that’s being tested. That was estimated as 1% of people have MCI. Or, for over-60s only, 5% of people have MCI. Now the calculation is easy. Suppose 10.000 people are tested. 1% (100 people) will have MCI, of which 80% (80 people) will be diagnosed correctly. And 9,900 do not have MCI, of which 95% will test negative (correctly). The numbers can be laid out in a tree diagram.
The total number of positive tests is 80 + 495 = 575, of which 495 are false positives. The fraction of tests that are false positives is 495/575= 86%.
Thus there is a 14% chance that if you test positive, you actually have MCI. 86% of people will be alarmed unnecessarily.
Even for people over 60. among whom 5% of the population have MC!, the test is gives the wrong result (54%) more often than it gives the right result (46%).
The test is clearly worse than useless. That was not made clear by the authors, or by the journal. It was not even made clear by NHS Choices.
It should have been.
It’s easy to put the tree diagram in the form of an equation. Denote sensitivity as sens, specificity as spec and prevalence as prev.
The probability that a positive test means that you actually have the condition is given by
\[\frac{sens.prev}{sens.prev + \left(1-spec\right)\left(1-prev\right) }\; \]
In the example above, sens = 0.8, spec = 0.95 and prev = 0.01, so the fraction of positive tests that give the right result is
\[\frac{0.8 \times 0.01}{0.8 \times 0.01 + \left(1 – 0.95 \right)\left(1 – 0.01\right) }\; = 0.139 \]
So 13.9% of positive tests are right, and 86% are wrong, as found in the tree diagram.
The lipid test for Alzheimers’
Another Alzheimers’ test has been in the headlines very recently. It performs even worse than the 15-minute test, but nobody seems to have noticed. It was published in Nature Medicine, by Mapstone et al. (2014). According to the paper, the sensitivity is 90% and the specificity is 90%, so, by constructing a tree, or by using the equation, the probability that you are ill, given that you test positive is a mere 8% (for a prevalence of 1%). And even for over-60s (prevalence 5%), the value is only 32%, so two-thirds of positive tests are still wrong. Again this was not pointed out by the authors. Nor was it mentioned by Nature Medicine in its commentary on the paper. And once again, NHS Choices missed the point.
Why does there seem to be a conspiracy of silence about the deficiencies of screening tests? It has been explained very clearly by people like Margaret McCartney who understand the problems very well. Is it that people are incapable of doing the calculations? Surely not. Is it that it’s better for funding to pretend you’ve invented a good test, when you haven’t? Do journals know that anything to do with Alzheimers’ will get into the headlines, and don’t want to pour cold water on a good story?
Whatever the explanation, it’s bad science that can harm people.
Follow-up
March 12 2014. This post was quickly picked up by the ampp3d blog, run by the Daily Mirror. Conrad Quilty-Harper showed some nice animations under the heading How a “90% accurate” Alzheimer’s test can be wrong 92% of the time.
March 12 2014.
As so often, the journal promoted the paper in a way that wasn’t totally accurate. Hype is more important than accuracy, I guess.

June 12 2014.
The empirical evidence shows that “general health checks” (a euphemism for mass screening of the healthy) simply don’t help. See review by Gøtzsche, Jørgensen & Krogsbøll (2014) in BMJ. They conclude
“Doctors should not offer general health checks to their patients,and governments should abstain from introducing health check programmes, as the Danish minister of health did when she learnt about the results of the Cochrane review and the Inter99 trial. Current programmes, like the one in the United Kingdom,should be abandoned.”
8 July 2014
Yet another over-hyped screening test for Alzheimer’s in the media. And once again. the hype originated in the press release, from Kings College London this time. The press release says
"They identified a combination of 10 proteins capable of predicting whether individuals with MCI would develop Alzheimer’s disease within a year, with an accuracy of 87 percent"
The term “accuracy” is not defined in the press release. And it isn’t defined in the original paper either. I’ve written to senior author, Simon Lovestone to try to find out what it means. The original paper says
"Sixteen proteins correlated with disease severity and cognitive decline. Strongest associations were in the MCI group with a panel of 10 proteins predicting progression to AD (accuracy 87%, sensitivity 85% and specificity 88%)."
A simple calculation, as shown above, tells us that with sensitivity 85% and specificity 88%. the fraction of people who have a positive test who are diagnosed correctly is 44%. So 56% of positive results are false alarms. These numbers assume that the prevalence of the condition in the population being tested is 10%, a higher value than assumed in other studies. If the prevalence were only 5% the results would be still worse: 73% of positive tests would be wrong. Either way, that’s not good enough to be useful as a diagnostic method.
In one of the other recent cases of Alzheimer’s tests, six months ago, NHS Choices fell into the same trap. They changed it a bit after I pointed out the problem in the comments. They seem to have learned their lesson because their post on this study was titled “Blood test for Alzheimer’s ‘no better than coin toss’ “. That’s based on the 56% of false alarms mention above.
The reports on BBC News and other media totally missed the point. But, as so often, their misleading reports were based on a misleading press release. That means that the university, and ultimately the authors, are to blame.
I do hope that the hype has no connection with the fact that Conflicts if Interest section of the paper says
"SL has patents filed jointly with Proteome Sciences plc related to these findings"
What it doesn’t mention is that, according to Google patents, Kings College London is also a patent holder, and so has a vested interest in promoting the product.
Is it really too much to expect that hard-pressed journalists might do a simple calculation, or phone someone who can do it for them? Until that happens, misleading reports will persist.
9 July 2014
It was disappointing to see that the usually excellent Sarah Boseley in the Guardian didn’t spot the problem either. And still more worrying that she quotes Dr James Pickett, head of research at the Alzheimer’s Society, as saying
These 10 proteins can predict conversion to dementia with less than 90% accuracy, meaning one in 10 people would get an incorrect result.
That number is quite wrong. It isn’t 1 in 10, it’s rather more than 1 in 2.
A resolution
After corresponding with the author, I now see what is going on more clearly.
The word "accuracy" was not defined in the paper, but was used in the press release and widely cited in the media. What it means is the ratio of the total number of true results (true positives + true negatives) to the total number of all results. This doesn’t seem to me to be useful number to give at all, because it conflates false negatives and false positives into a single number. If a condition is rare, the number of true negatives will be large (as shown above), but this does not make it a good test. What matters most to patients is not accuracy, defined in this way, but the false discovery rate.
The author makes it clear that the results are not intended to be a screening test for Alzheimer’s. It’s obvious from what’s been said that it would be a lousy test. Rather, the paper was intended to identify patients who would eventually (well, within only 18 months) get dementia. The denominator (always the key to statistical problems) in this case is the highly atypical patients that who come to memory clinics in trials centres (the potential trials population). The prevalence in this very restricted population may indeed be higher that the 10 percent that I used above.
Reading between the lines of the press release, you might have been able to infer some of thus (though not the meaning of “accuracy”). The fact that the media almost universally wrote up the story as a “breakthrough” in Alzeimer’s detection, is a consequence of the press release and of not reading the original paper.
I wonder whether it is proper for press releases to be issued at all for papers like this, which address a narrow technical question (selection of patients for trials). That us not a topic of great public interest. It’s asking for misinterpretation and that’s what it got.
I don’t suppose that it escaped the attention of the PR people at Kings that anything that refers to dementia is front page news, whether it’s of public interest or not. When we had an article in Nature in 2008, I remember long discussions about a press release with the arts graduate who wrote it (not at our request). In the end we decides that the topic was not of sufficient public interest to merit a press release and insisted that none was issued. Perhaps that’s what should have happened in this case too.
This discussion has certainly illustrated the value of post-publication peer review. See, especially, the perceptive comments, below, from Humphrey Rang and from Dr Aston and from Dr Kline.
14 July 2014. Sense about Science asked me to write a guest blog to explain more fully the meaning of "accuracy", as used in the paper and press release. It’s appeared on their site and will be reposted on this blog soon.
Last year, I was sent my answer paper for one of my final exams, taken in 1959. This has triggered a bout of shamelessly autobiographical nostalgia.
|
The answer sheets that I wrote had been kept by one of my teachers at Leeds, Dr George Mogey. After he died in 2003, aged 86, his widow, Audrey, found them and sent them to me. And after a hunt through the junk piled high in my office, I found the exam papers from that year too. George Mogey was an excellent teacher and a kind man. He gave most of the lectures to medical students, which we, as pharmacy/pharmacology students attended. His lectures were inspirational. |
|
Today, 56 years on, I can still recall vividly his lecture on anti-malarial drugs. At the end he paused dramatically and said “Since I started speaking, 100 people have died from malaria” (I don’t recall the exact number). He was the perfect antidote to people who say you learn nothing from lectures. Straight after the war (when he had seen the problem of malaria at first hand) he went to work at the Wellcome Research Labs in Beckenham, Kent. The first head of the Wellcome Lab was Henry Dale. It had a distinguished record of basic research as well as playing a crucial role in vaccine production and in development of the safe use of digitalis. In the 1930s it had an important role in the development of proper methods for biological standardisation. This was crucial for ensuring that, for example, each batch of tincture ot digitalis had the same potency (it has been described previously on this blog in Plants as Medicines. |
|
When George Mogey joined the Wellcome lab, its head was J.W. Trevan (1887 – 1956) (read his Biographical Memoir, written by J.H. Gaddum). Trevan’s most memorable contributions were in improving the statistics of biological assays. The ideas of individual effective dose and median effective dose were developed by him. His 1927 paper The Error of Determination of Toxicity is a classic of pharmacology. His advocacy of the well-defined quantity, median effective dose as a replacement for the ill-defined minimum effective dose was influential in the development of proper statistical analysis of biological assays in the 1930s. |
Trevan is something of hero to me. And he was said to be very forgetful. Gaddum, in his biographical memoir, recounts this story
“One day when he had lost something and suspected that it had been tidied away by his secretary, he went round muttering ‘It’s all due to this confounded tidiness. It always leads to trouble. I won’t have it in my lab.’ “
|
Trevan coined the abbreviation LD50 for the median lethal dose of a drug. George Mogey later acquired the car number plate LD50, in honour of Trevan, and his widow, Audrey, still has it (picture on right). |
Mogey wrote several papers with Trevan. In 1948 he presented one at a meeting of the Physiological Society. The programme included also A.V. Hill. E.J Denton, Bernhard [sic] Katz, J.Z. Young and Richard Keynes (Keynes was George Henry Lewes Student at Cambridge: Lewes was the Victorian polymath with whom the novelist George Eliot lived, openly unmarried, and a founder of the Physiological Society. He probably inspired the medical content of Eliot’s best known novel, Middlemarch).
|
Mogey may not have written many papers, but he was the sort of inspiring teacher that universities need. He had a letter in Nature on Constituents of Amanita Muscaria, the fly agaric toadstool, which appeared in 1965. That might explain why we went on a toadstool-hunting field trip. |
The tradition of interest in statistics and biological assay must have rubbed off on me, because the answers I gave in the exam were very much in that tradition. Here is a snippet (click to download the whole answer sheet).
A later answer was about probit analysis, an idea introduced by statistician Chester Bliss (1899–1979) in 1934, as an direct extension of Trevan’s work. (I met Bliss in 1970 or 1971 when I was in Yale -we had dinner, went to a theatre -then back to his apartment where he insisted on showing me his collection of erotic magazines!)
This paper was a pharmacology paper in my first final exam at the end of my third year. The external examiner was Walter Perry, head of pharmacology in Edinburgh (he went on to found the Open University). He had previously been head of Biological Standards at the National Institute for Medical Research, a job in which he had to know some statistics. In the oral exam he asked me a killer question “What is the difference between confidence limits and fiducial limits?”. I had no real idea (and, as I discovered later, neither did he). After that, I went on to do the 4th year where we specialised in pharmacology, and I spent quite a lot of time trying to answer that question. The result was my first ever paper, published in the University of Leeds Medical Journal. I hinted, obliquely, that the idea of fiducial inference was probably Ronald Fisher‘s only real mistake. I think that is the general view now, but Fisher was such a towering figure in statistics that nobody said that straight out (he was still alive when this was written -he died in 1962).
It is well-worth looking at a paper that Fisher gave to the Royal Statistical Society in 1935, The Logic of Inductive Inference. Then, as now, it was the custom for a paper to be followed by a vote of thanks, and a seconder. These, and the subsequent discussion, are all printed, and they could be quite vicious in a polite way. Giving the vote of thanks, Professor A.L. Bowley said
“It is not the custom, when the Council invites a member to propose a vote of thanks on a paper, to instruct him to bless it. If to some extent I play the inverse role of Balaam, it is not without precedent;”
And the seconder, Dr Isserlis, said
“There is no doubt in my mind at all about that, but Professor Fisher, like other fond parents, may perhaps see in his offspring qualities which to his mind no other children possess; others, however, may consider that the offspring are not unique.”
Post-publication peer review was already alive and well in 1935.
I was helped enormously in writing this paper by Dr B.L.Welch (1911 – 1989), whose first year course in statistics for biologists was a compulsory part of the course. Welch was famous particularly for having extended Student’s t distribution to the case where the variances in two samples being compared are unequal (Welch, 1947). He gave his whole lecture with his back to the class while writing what he said on a set of blackboards that occupied the whole side of the room. No doubt he would have failed any course about how to give a lecture. I found him riveting. He went slowly, and you could always check your notes because it was all there on the blackboards.
Walter Perry seemed to like my attempt to answer his question, despite the fact that it failed. After the 4th year final (a single 3 hour essay on drugs that affect protein synthesis) he offered me a PhD place in Edinburgh. He was one of my supervisors, though I never saw him except when he dropped into the lab for a cigarette between committee meetings. While in Edinburgh I met the famous statistician. David Finney, whose definitive book on the Statistics of Biological Assay was an enormous help when I later wrote Lectures on Biostatistics and a great help in getting my first job at UCL in 1964. Heinz Otto Schild. then the famous head of department, had written a paper in 1942 about the statistical analysis of 2+2 dose biological assays, while interned at the beginning of the war. He wanted someone to teach it to students, so he gave me a job. That wouldn’t happen now, because that sort of statistics would be considered too difficult Incidentally, I notice that Schild uses 99% confidence limits in his paper, not the usual 95% limits which make your results look better
It was clear even then, that the basis of statistical inference was an exceedingly contentious matter among statisticians. It still is, but the matter has renewed importance in view of the crisis of reproducibility in science. The question still fascinates me, and I’m planning to update my first paper soon. This time I hope it will be a bit better.
Postscript: some old pictures
While in nostalgic mood, here are a few old pictures. First, the only picture I have from undergraduate days. It was taken on a visit to May and Baker (of sulphonamide fame) in February 1957 (so I must have been in my first year). There were 15 or so in the class for the first three years (now, you can get 15 in a tutorial group). I’m in the middle of the back row (with hair!). The only names that I recall are those of the other two who went into the 4th year with me, Ed Abbs (rightmost on back row) and Stella Gregory (2nd from right, front row). Ed died young and Stella went to Australia. Just in front of me are James Dare (with bow tie) and Mr Nelson (who taught old fashioned pharmacognosy).
|
James Dare taught pharmaceutics, but he also had a considerable interest in statistics and we did lots of calculations with electromechanical calculators -the best of them was a Monroe (here’s a picture of one with the case removed to show the amazingly intricate mechanism). |
>
Monroe 8N-213 from http://www.science.uva.nl/museum/calclist.php |
The history of UCL’s pharmacology goes back to 1905. For most of that time, it’s been a pretty good department. It got top scores in all the research assessments until it was abolished by Malcolm Grant in 2007. That act of vandalism is documented in my diary section.

For most of its history, there was one professor who was head of the department. That tradition ended in 1983,when Humphrey Rang left for Novartis. The established chair was then empty for two years, until Donald Jenkinson, then head of department, insisted with characteristic modesty, that I rather than he should take the chair. Some time during the subsequent reign of David Brown, it was decided to name the chairs, and mine became the A.J. Clark chair. It was decided that the headship of the department would rotate, between Donald, David Brown and me. But when it came to my turn, I decided I was much too interested in single ion channels to spend time pushing paper, and David Brown nobly extended his term. The A.J. Clark chair was vacant after I ‘retired’ in 2004, but in 2014, Lucia Sivilotti was appointed to the chair, a worthy successor in its quantitative tradition.
The first group picture of UCL’s Pharmacology department was from 1972. Heinz Schild is in the middle of the front row, with Desmond Laurence on his left. Between them they dominated the textbook market: Schild edited A.J. Clark’s Pharmacology (now known as Rang and Dale). Laurence wrote a very successful text, Clinical Pharmacology. Click on the picture for a bigger version, with names, as recalled by Donald Jenkinson: (DHJ). I doubt whether many people now remember Ada Corbett (the tea lady) or Frank Ballhatchet from the mechanical workshop. He could do superb work, though the price was to spent 10 minutes chatting about his Land Rover, or listening to reminiscences of his time working on Thames barges. I still have a beautiful 8-way tap that he made. with a jerk-free indexing mechanism.
The second Departmental picture was taken in June 1980. Humphrey Rang was head of department then. My colleagues David Ogden and Steven Siegelbaum are there. In those days we had a tea lady too, Joyce Mancini. (Click pictures to enlarge)
Follow-up
This post is the original version of a post by Michael Vagg. It was posted at the Conversation but taken down within hours, on legal advice. Sadly, the Conversation has a track record for pusillanimous behaviour of this sort. It took minutes before the cached version reappeared on freezepage.com. I’m reposting it from there in the interests of free speech. La Trobe "university" should be ashamed that it’s prostituted itself for the sake of $15 m.
La Trobe’s deputy vice-chancellor, Keith Nugent, gives a make-believe response to the resignation of Ken Harvey in a video. It is, in my opinion, truly pathetic.
Update, The next day, the article was reposted at the Conversation. The changes they’d made can be seen in a compare document. The biggest change was removal of "has just decided to join the ranks of the spivs and hucksters of the vitamin industry". This seems to me to be perfectly fair comment. It should not have been censored by the Conversation.
By Michael Vagg
The recent memorandum of understanding signed between supplement company Swisse and La Trobe University to establish a Complementary Medicine Evidence Centre (CMEC) looks to me like the latest effort by a corporation to cloak their business interests in a veil of science. Unlike the UTS Sydney Australian Research Centre in Complementary and Integrative Medicine (ARCCIM), which at least has significant NHMRC funding, the La Trobe version will undertake “independent research” into complementary and alternative medicine (CAM) products that are made by the major (and so far only) donor to the Centre. Southern Cross University also has a very close relationship with the Blackmores brand of CAM products, due to the personal interest of Marcus Blackmore, the company Chairman. Blackmores claims to spend a lazy couple of million a year on their branded research centre. The Blackmores Research Centre studies Blackmores products. Presumably this situation (so similar to the proposed La Trobe model) is a coincidence since the research centre is providing completely “independent” research.
The conflict of interest in such research centres is so laughably obvious that A/Prof Ken Harvey, a leading campaigner against shonky health products, a life member of Choice andThe Conversation contributor, has resigned his appointment at La Trobe in protest. Ken clearly points out in his letter of resignation that by accepting the money from Swisse, he believes La Trobe has unacceptably compromised its integrity. His letter cites multiple instances of non-compliance with TGA regulations by Swisse, as well as their disrespect for the regulatory process that governs corporate truth-telling in their industry.This story from last year gives a bit of background to the quixotic battle Harvey has fought against the massive coffers and unscrupulous business practices of Big Supplement. He has been more effective than the TGA itself at hindering the rampant gaming of the TGA Register of Therapeutic Goods by supplement and vitamin manufacturers.
Clearly as a man of principle, he could not be expected to continue his association with a university that has a close relationship to a company with such a history of regulatory infringements. The untenability of Ken’s position is underlined by the fact that La Trobe itself republished on their website one of his TC articles about Swisse’s regulatory tapdancing only the previous year!
Ken has been sued, traduced and generally railed against by a multi-billion dollar industry for the hideous crime of insisting that they tell the truth about their products and not mislead consumers. We need another hundred like him. That his own university has decided to take the money on offer from Swisse must be a bitter blow to him. It would be interesting to know whether any other universities were approached by Swisse in a similar way and had the courage to decline the offer.
The infiltration of academia by privately funded CAM institutes is old news in the United States. The Science Based Medicine blog has christened the phenomenon “quackademic medicine” and written about it at some length. It seems the Australian CAM industry has no need to hide behind astroturfing organisations like the American group the Bravewell Collaborative to get its agenda attended to. Companies like Blackmores and Swisse can seemingly just offer to fund research institutes and cash-strapped tertiary institutions can’t resist. Friends of Science in Medicine and others have had a bit to say about the irresponsibility of educational institutions lending credibility to pseudoscience and how this practice damages universities’ standing as exemplars of scholarship and intellectual leaders within their communities.
I can say without qualification that none of the much-maligned Big Pharma companies have their own fully-funded research centres at any university. Let alone a branded one where the studies are restricted to a single company’s products. It would be utterly unacceptable for the integrity of any university for such an outrageously conflicted institution to be given any support. What would it be like if GSK or Pfizer founded a research institute at a university and forced the researchers to only study their own products?
Imagine the outrage. Imagine what a laughing stock such a research centre would be. That’s medical research in clown shoes. That’s academic credibility in a cheap suit trying to sell you steak knives.
Vitamin and supplement companies will always be profitable because their sales pitch is based on psychological flaws that everyone has. Just ask the gaming, alcohol and tobacco companies. All of them are massively profitable. Sometimes their cash can even do good, but there’s always an angle by which they profit.
Look at these guys up close, and the warts appear. All of them seek to improve their image by splashing money on hanging around with the glamorous, the successful, the smart and the credible. They hope that the magic dust of celebrity and academia will disguise the stench of the swamp they crawled out from. La Trobe Uni has just decided to join the ranks of the spivs and hucksters of the vitamin industry, and they will now have to live with having a research centre with the academic and professional credibility of the Ponds Institute. Sadly for La Trobe, they won’t have Ken Harvey to keep things reality-based.
Follow-up
8 February 2014. Deputy vice-chancellor, Keith Nugent, tried to defend the university’s decision to take money from the "spivs and hucksters of the vitamin industry" in The Age. I sent the following letter to The Age. Let’s hope they publish it.
|
Keith Nugent, deputy vice-chancellor of La Trobe University, has offered a defence of the university’s decision to take a large amount of money from vitamin and herb company, Swisse. He justifies this by saying that we need to know whether or not the products work. Nugent seems to be unaware that we already know. There have been many good double-blind randomized trials and they have just about all shown that dosing yourself with vitamins and minerals does most people no good at all. Some have shown that high doses actually harm you. Perhaps the university should have checked what’s already known before taking the money. Perhaps Nugent is also unaware that trials with industry sponsorship tend to come out favourable to the companies’ product. For that reason, the results are treated with scepticism by the scientific community. If the research is worth doing, then it will be funded from the normal sources. There should be no need to take money from a company with a very strong financial interest in the outcome. D. Colquhoun FRS Professor of Pharmcology |
This discussion seemed to be of sufficient general interest that we submitted is as a feature to eLife, because this journal is one of the best steps into the future of scientific publishing. Sadly the features editor thought that " too much of the article is taken up with detailed criticisms of research papers from NEJM and Science that appeared in the altmetrics top 100 for 2013; while many of these criticisms seems valid, the Features section of eLife is not the venue where they should be published". That’s pretty typical of what most journals would say. It is that sort of attitude that stifles criticism, and that is part of the problem. We should be encouraging post-publication peer review, not suppressing it. Luckily, thanks to the web, we are now much less constrained by journal editors than we used to be.
Here it is.
Scientists don’t count: why you should ignore altmetrics and other bibliometric nightmares
David Colquhoun1 and Andrew Plested2
1 University College London, Gower Street, London WC1E 6BT
2 Leibniz-Institut für Molekulare Pharmakologie (FMP) & Cluster of Excellence NeuroCure, Charité Universitätsmedizin,Timoféeff-Ressowsky-Haus, Robert-Rössle-Str. 10, 13125 Berlin Germany.
Jeffrey Beall is librarian at Auraria Library, University of Colorado Denver. Although not a scientist himself, he, more than anyone, has done science a great service by listing the predatory journals that have sprung up in the wake of pressure for open access. In August 2012 he published “Article-Level Metrics: An Ill-Conceived and Meretricious Idea. At first reading that criticism seemed a bit strong. On mature consideration, it understates the potential that bibliometrics, altmetrics especially, have to undermine both science and scientists.
Altmetrics is the latest buzzword in the vocabulary of bibliometricians. It attempts to measure the “impact” of a piece of research by counting the number of times that it’s mentioned in tweets, Facebook pages, blogs, YouTube and news media. That sounds childish, and it is. Twitter is an excellent tool for journalism. It’s good for debunking bad science, and for spreading links, but too brief for serious discussions. It’s rarely useful for real science.
Surveys suggest that the great majority of scientists do not use twitter (7 — 13%). Scientific works get tweeted about mostly because they have titles that contain buzzwords, not because they represent great science.
What and who is Altmetrics for?
The aims of altmetrics are ambiguous to the point of dishonesty; they depend on whether the salesperson is talking to a scientist or to a potential buyer of their wares.
At a meeting in London , an employee of altmetric.com said “we measure online attention surrounding journal articles” “we are not measuring quality …” “this whole altmetrics data service was born as a service for publishers”, “it doesn’t matter if you got 1000 tweets . . .all you need is one blog post that indicates that someone got some value from that paper”.
These ideas sound fairly harmless, but in stark contrast, Jason Priem (an author of the altmetrics manifesto) said one advantage of altmetrics is that it’s fast “Speed: months or weeks, not years: faster evaluations for tenure/hiring”. Although conceivably useful for disseminating preliminary results, such speed isn’t important for serious science (the kind that ought to be considered for tenure) which operates on the timescale of years. Priem also says “researchers must ask if altmetrics really reflect impact” . Even he doesn’t know, yet altmetrics services are being sold to universities, before any evaluation of their usefulness has been done, and universities are buying them. The idea that altmetrics scores could be used for hiring is nothing short of terrifying.
The problem with bibliometrics
The mistake made by all bibliometricians is that they fail to consider the content of papers, because they have no desire to understand research. Bibliometrics are for people who aren’t prepared to take the time (or lack the mental capacity) to evaluate research by reading about it, or in the case of software or databases, by using them. The use of surrogate outcomes in clinical trials is rightly condemned. Bibliometrics are all about surrogate outcomes.
If instead we consider the work described in particular papers that most people agree to be important (or that everyone agrees to be bad), it’s immediately obvious that no publication metrics can measure quality. There are some examples in How to get good science (Colquhoun, 2007). It is shown there that at least one Nobel prize winner failed dismally to fulfil arbitrary biblometric productivity criteria of the sort imposed in some universities (another example is in Is Queen Mary University of London trying to commit scientific suicide?).
Schekman (2013) has said that science
“is disfigured by inappropriate incentives. The prevailing structures of personal reputation and career advancement mean the biggest rewards often follow the flashiest work, not the best.”
Bibliometrics reinforce those inappropriate incentives. A few examples will show that altmetrics are one of the silliest metrics so far proposed.
The altmetrics top 100 for 2103
The superficiality of altmetrics is demonstrated beautifully by the list of the 100 papers with the highest altmetric scores in 2013 For a start, 58 of the 100 were behind paywalls, and so unlikely to have been read except (perhaps) by academics.
The second most popular paper (with the enormous altmetric score of 2230) was published in the New England Journal of Medicine. The title was Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. It was promoted (inaccurately) by the journal with the following tweet:

Many of the 2092 tweets related to this article simply gave the title, but inevitably the theme appealed to diet faddists, with plenty of tweets like the following:


The interpretations of the paper promoted by these tweets were mostly desperately inaccurate. Diet studies are anyway notoriously unreliable. As John Ioannidis has said
"Almost every single nutrient imaginable has peer reviewed publications associating it with almost any outcome."
This sad situation comes about partly because most of the data comes from non-randomised cohort studies that tell you nothing about causality, and also because the effects of diet on health seem to be quite small.
The study in question was a randomized controlled trial, so it should be free of the problems of cohort studies. But very few tweeters showed any sign of having read the paper. When you read it you find that the story isn’t so simple. Many of the problems are pointed out in the online comments that follow the paper. Post-publication peer review really can work, but you have to read the paper. The conclusions are pretty conclusively demolished in the comments, such as:
“I’m surrounded by olive groves here in Australia and love the hand-pressed EVOO [extra virgin olive oil], which I can buy at a local produce market BUT this study shows that I won’t live a minute longer, and it won’t prevent a heart attack.”
We found no tweets that mentioned the finding from the paper that the diets had no detectable effect on myocardial infarction, death from cardiovascular causes, or death from any cause. The only difference was in the number of people who had strokes, and that showed a very unimpressive P = 0.04.
Neither did we see any tweets that mentioned the truly impressive list of conflicts of interest of the authors, which ran to an astonishing 419 words.
“Dr. Estruch reports serving on the board of and receiving lecture fees from the Research Foundation on Wine and Nutrition (FIVIN); serving on the boards of the Beer and Health Foundation and the European Foundation for Alcohol Research (ERAB); receiving lecture fees from Cerveceros de España and Sanofi-Aventis; and receiving grant support through his institution from Novartis. Dr. Ros reports serving on the board of and receiving travel support, as well as grant support through his institution, from the California Walnut Commission; serving on the board of the Flora Foundation (Unilever). . . “
And so on, for another 328 words.
The interesting question is how such a paper came to be published in the hugely prestigious New England Journal of Medicine. That it happened is yet another reason to distrust impact factors. It seems to be another sign that glamour journals are more concerned with trendiness than quality.
One sign of that is the fact that the journal’s own tweet misrepresented the work. The irresponsible spin in this initial tweet from the journal started the ball rolling, and after this point, the content of the paper itself became irrelevant. The altmetrics score is utterly disconnected from the science reported in the paper: it more closely reflects wishful thinking and confirmation bias.
The fourth paper in the altmetrics top 100 is an equally instructive example.
|
This work was also published in a glamour journal, Science. The paper claimed that a function of sleep was to “clear metabolic waste from the brain”. It was initially promoted (inaccurately) on Twitter by the publisher of Science. After that, the paper was retweeted many times, presumably because everybody sleeps, and perhaps because the title hinted at the trendy, but fraudulent, idea of “detox”. Many tweets were variants of “The garbage truck that clears metabolic waste from the brain works best when you’re asleep”. |
But this paper was hidden behind Science’s paywall. It’s bordering on irresponsible for journals to promote on social media papers that can’t be read freely. It’s unlikely that anyone outside academia had read it, and therefore few of the tweeters had any idea of the actual content, or the way the research was done. Nevertheless it got “1,479 tweets from 1,355 accounts with an upper bound of 1,110,974 combined followers”. It had the huge Altmetrics score of 1848, the highest altmetric score in October 2013.
Within a couple of days, the story fell out of the news cycle. It was not a bad paper, but neither was it a huge breakthrough. It didn’t show that naturally-produced metabolites were cleared more quickly, just that injected substances were cleared faster when the mice were asleep or anaesthetised. This finding might or might not have physiological consequences for mice.
Worse, the paper also claimed that “Administration of adrenergic antagonists induced an increase in CSF tracer influx, resulting in rates of CSF tracer influx that were more comparable with influx observed during sleep or anesthesia than in the awake state”. Simply put, giving the sleeping mice a drug could reduce the clearance to wakeful levels. But nobody seemed to notice the absurd concentrations of antagonists that were used in these experiments: “adrenergic receptor antagonists (prazosin, atipamezole, and propranolol, each 2 mM) were then slowly infused via the cisterna magna cannula for 15 min”. Use of such high concentrations is asking for non-specific effects. The binding constant (concentration to occupy half the receptors) for prazosin is less than 1 nM, so infusing 2 mM is working at a million times greater than the concentration that should be effective. That’s asking for non-specific effects. Most drugs at this sort of concentration have local anaesthetic effects, so perhaps it isn’t surprising that the effects resembled those of ketamine.
The altmetrics editor hadn’t noticed the problems and none of them featured in the online buzz. That’s partly because to find it out you had to read the paper (the antagonist concentrations were hidden in the legend of Figure 4), and partly because you needed to know the binding constant for prazosin to see this warning sign.
The lesson, as usual, is that if you want to know about the quality of a paper, you have to read it. Commenting on a paper without knowing anything of its content is liable to make you look like an jackass.
A tale of two papers
Another approach that looks at individual papers is to compare some of one’s own papers. Sadly, UCL shows altmetric scores on each of your own papers. Mostly they are question marks, because nothing published before 2011 is scored. But two recent papers make an interesting contrast. One is from DC’s side interest in quackery, one was real science. The former has an altmetric score of 169, the latter has an altmetric score of 2.
|
The first paper was “Acupuncture is a theatrical placebo”, which was published as an invited editorial in Anesthesia and Analgesia [download pdf]. The paper was scientifically trivial. It took perhaps a week to write. Nevertheless, it got promoted it on twitter, because anything to do with alternative medicine is interesting to the public. It got quite a lot of retweets. And the resulting altmetric score of 169 put it in the top 1% of all articles altmetric have tracked, and the second highest ever for Anesthesia and Analgesia. As well as the journal’s own website, the article was also posted on the DCScience.net blog (May 30, 2013) where it soon became the most viewed page ever (24,468 views as of 23 November 2013), something that altmetrics does not seem to take into account. |

|
Compare this with the fate of some real, but rather technical, science.
|
My [DC] best scientific papers are too old (i.e. before 2011) to have an altmetrics score, but my best score for any scientific paper is 2. This score was for Colquhoun & Lape (2012) “Allosteric coupling in ligand-gated ion channels”. It was a commentary with some original material. The altmetric score was based on two tweets and 15 readers on Mendeley. The two tweets consisted of one from me (“Real science; The meaning of allosteric conformation changes http://t.co/zZeNtLdU ”). The only other tweet as abusive one from a cyberstalker who was upset at having been refused a job years ago. Incredibly, this modest achievement got it rated “Good compared to other articles of the same age (71st percentile)”. |

|
Conclusions about bibliometrics
Bibliometricians spend much time correlating one surrogate outcome with another, from which they learn little. What they don’t do is take the time to examine individual papers. Doing that makes it obvious that most metrics, and especially altmetrics, are indeed an ill-conceived and meretricious idea. Universities should know better than to subscribe to them.
Although altmetrics may be the silliest bibliometric idea yet, much this criticism applies equally to all such metrics. Even the most plausible metric, counting citations, is easily shown to be nonsense by simply considering individual papers. All you have to do is choose some papers that are universally agreed to be good, and some that are bad, and see how metrics fail to distinguish between them. This is something that bibliometricians fail to do (perhaps because they don’t know enough science to tell which is which). Some examples are given by Colquhoun (2007) (more complete version at dcscience.net).
Eugene Garfield, who started the metrics mania with the journal impact factor (JIF), was clear that it was not suitable as a measure of the worth of individuals. He has been ignored and the JIF has come to dominate the lives of researchers, despite decades of evidence of the harm it does (e.g.Seglen (1997) and Colquhoun (2003) ) In the wake of JIF, young, bright people have been encouraged to develop yet more spurious metrics (of which ‘altmetrics’ is the latest). It doesn’t matter much whether these metrics are based on nonsense (like counting hashtags) or rely on counting links or comments on a journal website. They won’t (and can’t) indicate what is important about a piece of research- its quality.
People say – I can’t be a polymath. Well, then don’t try to be. You don’t have to have an opinion on things that you don’t understand. The number of people who really do have to have an overview, of the kind that altmetrics might purport to give, those who have to make funding decisions about work that they are not intimately familiar with, is quite small. Chances are, you are not one of them. We review plenty of papers and grants. But it’s not credible to accept assignments outside of your field, and then rely on metrics to assess the quality of the scientific work or the proposal.
It’s perfectly reasonable to give credit for all forms of research outputs, not only papers. That doesn’t need metrics. It’s nonsense to suggest that altmetrics are needed because research outputs are not already valued in grant and job applications. If you write a grant for almost any agency, you can put your CV. If you have a non-publication based output, you can always include it. Metrics are not needed. If you write software, get the numbers of downloads. Software normally garners citations anyway if it’s of any use to the greater community.
When AP recently wrote a criticism of Heather Piwowar’s altmetrics note in Nature, one correspondent wrote: "I haven’t read the piece [by HP] but I’m sure you are mischaracterising it". This attitude summarizes the too-long-didn’t-read (TLDR) culture that is increasingly becoming accepted amongst scientists, and which the comparisons above show is a central component of altmetrics.
Altmetrics are numbers generated by people who don’t understand research, for people who don’t understand research. People who read papers and understand research just don’t need them and should shun them.
But all bibliometrics give cause for concern, beyond their lack of utility. They do active harm to science. They encourage “gaming” (a euphemism for cheating). They encourage short-term eye-catching research of questionable quality and reproducibility. They encourage guest authorships: that is, they encourage people to claim credit for work which isn’t theirs. At worst, they encourage fraud.
No doubt metrics have played some part in the crisis of irreproducibility that has engulfed some fields, particularly experimental psychology, genomics and cancer research. Underpowered studies with a high false-positive rate may get you promoted, but tend to mislead both other scientists and the public (who in general pay for the work). The waste of public money that must result from following up badly done work that can’t be reproduced but that was published for the sake of “getting something out” has not been quantified, but must be considered to the detriment of bibliometrics, and sadly overcomes any advantages from rapid dissemination. Yet universities continue to pay publishers to provide these measures, which do nothing but harm. And the general public has noticed.
It’s now eight years since the New York Times brought to the attention of the public that some scientists engage in puffery, cheating and even fraud.
Overblown press releases written by journals, with connivance of university PR wonks and with the connivance of the authors, sometimes go viral on social media (and so score well on altmetrics). Yet another example, from Journal of the American Medical Association involved an overblown press release from the Journal about a trial that allegedly showed a benefit of high doses of Vitamin E for Alzheimer’s disease.
This sort of puffery harms patients and harms science itself.
We can’t go on like this.
What should be done?
Post publication peer review is now happening, in comments on published papers and through sites like PubPeer, where it is already clear that anonymous peer review can work really well. New journals like eLife have open comments after each paper, though authors do not seem to have yet got into the habit of using them constructively. They will.
It’s very obvious that too many papers are being published, and that anything, however bad, can be published in a journal that claims to be peer reviewed . To a large extent this is just another example of the harm done to science by metrics –the publish or perish culture.
Attempts to regulate science by setting “productivity targets” is doomed to do as much harm to science as it has in the National Health Service in the UK. This has been known to economists for a long time, under the name of Goodhart’s law.
Here are some ideas about how we could restore the confidence of both scientists and of the public in the integrity of published work.
- Nature, Science, and other vanity journals should become news magazines only. Their glamour value distorts science and encourages dishonesty.
- Print journals are overpriced and outdated. They are no longer needed. Publishing on the web is cheap, and it allows open access and post-publication peer review. Every paper should be followed by an open comments section, with anonymity allowed. The old publishers should go the same way as the handloom weavers. Their time has passed.
- Web publication allows proper explanation of methods, without the page, word and figure limits that distort papers in vanity journals. This would also make it very easy to publish negative work, thus reducing publication bias, a major problem (not least for clinical trials)
- Publish or perish has proved counterproductive. It seems just as likely that better science will result without any performance management at all. All that’s needed is peer review of grant applications.
- Providing more small grants rather than fewer big ones should help to reduce the pressure to publish which distorts the literature. The ‘celebrity scientist’, running a huge group funded by giant grants has not worked well. It’s led to poor mentoring, and, at worst, fraud. Of course huge groups sometimes produce good work, but too often at the price of exploitation of junior scientists
- There is a good case for limiting the number of original papers that an individual can publish per year, and/or total funding. Fewer but more complete and considered papers would benefit everyone, and counteract the flood of literature that has led to superficiality.
- Everyone should read, learn and inwardly digest Peter Lawrence’s The Mismeasurement of Science.
A focus on speed and brevity (cited as major advantages of altmetrics) will help no-one in the end. And a focus on creating and curating new metrics will simply skew science in yet another unsatisfactory way, and rob scientists of the time they need to do their real job: generate new knowledge.
It has been said
“Creation is sloppy; discovery is messy; exploration is dangerous. What’s a manager to do?
The answer in general is to encourage curiosity and accept failure. Lots of failure.”
And, one might add, forget metrics. All of them.
Follow-up
17 Jan 2014
This piece was noticed by the Economist. Their ‘Writing worth reading‘ section said
"Why you should ignore altmetrics (David Colquhoun) Altmetrics attempt to rank scientific papers by their popularity on social media. David Colquohoun [sic] argues that they are “for people who aren’t prepared to take the time (or lack the mental capacity) to evaluate research by reading about it.”"
20 January 2014.
Jason Priem, of ImpactStory, has responded to this article on his own blog. In Altmetrics: A Bibliographic Nightmare? he seems to back off a lot from his earlier claim (cited above) that altmetrics are useful for making decisions about hiring or tenure. Our response is on his blog.
20 January 2014.
Jason Priem, of ImpactStory, has responded to this article on his own blog, In Altmetrics: A bibliographic Nightmare? he seems to back off a lot from his earlier claim (cited above) that altmetrics are useful for making decisions about hiring or tenure. Our response is on his blog.
23 January 2014
The Scholarly Kitchen blog carried another paean to metrics, A vigorous discussion followed. The general line that I’ve followed in this discussion, and those mentioned below, is that bibliometricians won’t qualify as scientists until they test their methods, i.e. show that they predict something useful. In order to do that, they’ll have to consider individual papers (as we do above). At present, articles by bibliometricians consist largely of hubris, with little emphasis on the potential to cause corruption. They remind me of articles by homeopaths: their aim is to sell a product (sometimes for cash, but mainly to promote the authors’ usefulness).
It’s noticeable that all of the pro-metrics articles cited here have been written by bibliometricians. None have been written by scientists.
28 January 2014.
Dalmeet Singh Chawla,a bibliometrician from Imperial College London, wrote a blog on the topic. (Imperial, at least in its Medicine department, is notorious for abuse of metrics.)
29 January 2014 Arran Frood wrote a sensible article about the metrics row in Euroscientist.
2 February 2014 Paul Groth (a co-author of the Altmetrics Manifesto) posted more hubristic stuff about altmetrics on Slideshare. A vigorous discussion followed.
5 May 2014. Another vigorous discussion on ImpactStory blog, this time with Stacy Konkiel. She’s another non-scientist trying to tell scientists what to do. The evidence that she produced for the usefulness of altmetrics seemed pathetic to me.
7 May 2014 A much-shortened version of this post appeared in the British Medical Journal (BMJ blogs)
One of my scientific heroes is Bernard Katz. The closing words of his inaugural lecture, as professor of biophysics at UCL, hang on the wall of my office as a salutory reminder to refrain from talking about ‘how the brain works’. After speaking about his discoveries about synaptic transmission, he ended thus.
|
"My time is up and very glad I am, because I have been leading myself right up to a domain on which I should not dare to trespass, not even in an Inaugural Lecture. This domain contains the awkward problems of mind and matter about which so much has been talked and so little can be said, and having told you of my pedestrian disposition, I hope you will give me leave to stop at this point and not to hazard any further guesses." |
The question of what to eat for good health is truly a topic about "which so much has been talked and so little can be said"
That was emphasized yet again by an editorial in the British Medical Journal written by my favourite epidemiologist. John Ioannidis. He has been at the forefront of debunking hype. Its title is “Implausible results in human nutrition research” (BMJ, 2013;347:f6698.
Get pdf).
The gist is given by the memorable statement
"Almost every single nutrient imaginable has peer reviewed publications associating it with almost any outcome."
and the subtitle
“Definitive solutions won’t come from another million observational papers or small randomized trials“.
Being a bit obsessive about causality, this paper is music to my ears. The problem of causality was understood perfectly by Samuel Johnson, in 1756, and he was a lexicographer, not a scientist. Yet it’s widely ignored by epidemiologists.
The problem of causality is often mentioned in the introduction to papers that describe survey data, yet by the end of the paper, it’s usually forgotten, and public health advice is issued.
Ioannidis’ editorial vindicates my own views, as an amateur epidemiologist, on the results of the endless surveys of diet and health.
- Diet and health. What can you believe: or does bacon kill you (2009) in which I look at the World Cancer Research Fund’s evidence for causality (next to none in my opinion). Through this I got to know Gary Taubes, whose explanation of causality in the New York Times is the best popular account I’ve ever seen.
- How big is the risk from eating red meat now: an update (2012) This was based on the WCRF update – the risk was roughly halved though it didn’t say that in the press release.
- Another update. Red meat doesn’t kill you, but the spin is fascinating (2013). Update after the EPIC results in which the risk essentially vanished: good news which you could find only by digging into Table 3.
There is nothing new about the problem. It’s been written about many times. Young & Karr (Significance, 8, 116 – 120, 2011: get pdf) said "Any claim coming from an observational study is most likely to be wrong". Out of 52 claims made in 12 observational studies, not a single one was confirmed when tested by randomised controlled trials.
Another article cited by Ioannidis, "Myths, Presumptions, and Facts about Obesity" (Casazza et al , NEJM, 2013), debunks many myths, but the list of conflicts of interests declared by the authors is truly horrendous (and at least one of their conclusions has been challenged, albeit by people with funding from Kellogg’s). The frequent conflicts of interest in nutrition research make a bad situation even worse.
The quotation in bold type continues thus.
"On 25 October 2013, PubMed listed 291 papers with the keywords “coffee OR caffeine” and 741 with “soy,” many of which referred to associations. In this literature of epidemic proportions, how many results are correct? Many findings are entirely implausible. Relative risks that suggest we can halve the burden of cancer with just a couple of servings a day of a single nutrient still circulate widely in peer reviewed journals.
However, on the basis of dozens of randomized trials, single nutrients are unlikely to have relative risks less than 0.90 for major clinical outcomes when extreme tertiles of population intake are compared—most are greater than 0.95. For overall mortality, relative risks are typically greater than 0.995, if not entirely null. The respective absolute risk differences would be trivial. Observational studies and even randomized trials of single nutrients seem hopeless, with rare exceptions. Even minimal confounding or other biases create noise that exceeds any genuine effect. Big datasets just confer spurious precision status to noise."
And, later,
"According to the latest burden of disease study, 26% of deaths and 14% of disability adjusted life years in the United States are attributed to dietary risk factors, even without counting the impact of obesity. No other risk factor comes anywhere close to diet in these calculations (not even tobacco and physical inactivity). I suspect this is yet another implausible result. It builds on risk estimates from the same data of largely implausible nutritional studies discussed above. Moreover, socioeconomic factors are not considered at all, although they may be at the root of health problems. Poor diet may partly be a correlate or one of several paths through which social factors operate on health."
Another field that is notorious for producing false positives, wirh false attribution of causality, is the detection of biomarkers. A critical discussion can be found in the paper by Broadhurst & Kell (2006), "False discoveries in metabolomics and related experiments".
"Since the early days of transcriptome analysis (Golub et al., 1999), many workers have looked to detect different gene expression in cancerous versus normal tissues. Partly because of the expense of transcriptomics (and the inherent noise in such data (Schena, 2000; Tu et al., 2002; Cui and Churchill, 2003; Liang and Kelemen, 2006)), the numbers of samples and their replicates is often small while the number of candidate genes is typically in the thousands. Given the above, there is clearly a great danger that most of these will not in practice withstand scrutiny on deeper analysis (despite the ease with which one can create beautiful heat maps and any number of ‘just-so’ stories to explain the biological relevance of anything that is found in preliminary studies!). This turns out to be the case, and we review a recent analysis (Ein-Dor et al., 2006) of a variety of such studies."
The fields of metabolomics, proteomics and transcriptomics are plagued by statistical problems (as well as being saddled with ghastly pretentious names).
What’s to be done?
Barker Bausell, in his demolition of research on acupuncture, said:
[Page39] “But why should nonscientists care one iota about something as esoteric as causal inference? I believe that the answer to this question is because the making of causal inferences is part of our job description as Homo Sapiens.”
The problem, of course, is that humans are very good at attributing causality when it does not exist. That has led to confusion between correlation and cause on an industrial scale, not least in attempts to work out the effects of diet on health.
More than in any other field it is hard to do the RCTs that could, in principle, sort out the problem. It’s hard to allocate people at random to different diets, and even harder to make people stick to those diets for the many years that are needed.
We can probably say by now that no individual food carries a large risk, or affords very much protection. The fact that we are looking for quite small effects means that even when RCTs are possible huge samples will be needed to get clear answers. Most RCTs are too short, and too small (under-powered) and that leads to overestimation of the size of effects.
That’s a problem that plagues experimental pyschology too, and has led to a much-discussed crisis in reproducibility.
"Supplements" of one sort and another are ubiquitous in sports. Nobody knows whether they work, and the margin between winning and losing is so tiny that it’s very doubtful whether we ever will know. We can expect irresponsible claims to continue unabated.
The best thing that can be done in the short term is to stop doing large observational studies altogether. It’s now clear that inferences made from them are likely to be wrong. And, sad to say, we need to view with great skepticism anything that is funded by the food industry. And make a start on large RCTs whenever that is possible. Perhaps the hardest goal of all is to end the "publish or perish" culture which does so much to prevent the sort of long term experiments which would give the information we want.
Ioannidis’ article ends with the statement
"I am co-investigator in a randomized trial of a low carbohydrate versus low fat diet that is funded by the US National Institutes of Health and the non-profit Nutrition Science Initiative."
It seems he is putting his money where his mouth is.
Until we have the results, we shall continue to be bombarded with conflicting claims made by people who are doing their best with flawed methods, as well as by those trying to sell fad diets. Don’t believe them. The famous "5-a-day" advice that we are constantly bombarded with does no harm, but it has no sound basis.
As far as I can guess, the only sound advice about healthy eating for most people is
- don’t eat too much
- don’t eat all the same thing
You can’t make much money out of that advice.
No doubt that is why you don’t hear it very often.
Follow-up
Two relevant papers that show the unreliability of observational studies,
"Nearly 80,000 observational studies were published in the decade 1990–2000 (Naik 2012). In the following decade, the number of studies grew to more than 260,000". Madigan et al. (2014)
“. . . the majority of observational studies would declare statistical significance when no effect is present” Schuemie et al., (2012)
20 March 2014
On 20 March 2014, I gave a talk on this topic at the Cambridge Science Festival (more here). After the event my host, Yvonne Noblis, sent me some (doubtless cherry-picked) feedback she’d had about the talk.


The General Pharmaceutical Council (GPhC) has been the statutory body responsible for the regulation of pharmacy since 2010. It’s status is similar to that of the GMC and. heaven help us, the GCC. Before that the regulator was the same as the professional body, the Royal Pharmaceutical Society of Great Britain (RPS). The RPS proved to be as useless as most other regulators, as documented in detail in my 2008 post, At around the time it stopped being a regulator, the RPS started to condemn quackery more effectively, but by then it had lost the power to do much about it (I hope the latter wasn’t the cause of the former). The body that could do something, the GPhC has done essentially nothing. as described in this post.
I did a 2 year apprenticeship in Timothy White’s and Taylor’s Homeopathic (yes, really) Chemists in the 1950s.
My first degree was in pharmacy. I got my interest in pharmacology from reading Martindale’s Extra Pharmacopoeia in the shop. I soon decided that I didn’t really want to spend the rest of my life selling lipstick and Durex. The latter was quite a big seller because the Boots across the road didn’t sell contraceptives (they changed their minds in the 1960s).
In those days, we spent quite a lot of time making up (almost entirely ineffective) ‘tonics’ and ‘cough mixtures’. Now the job consists largely of counting pills. This has exacerbated the ‘chip on the shoulder’ attitude that was present even in the 1950s. For a long time now, pharmacists have wanted to become the a ‘third tier’ in the NHS, alongside GP practices and hospitals., after hospitals and doctors". . Here are a few comments on this proposition.
First let me say that I’ve met some very good and ethical pharmacists. I did a vacation job in a hospital pharmacy where the boss had an encyclopaedic knowledge of the effects and side effects of drugs, and of their dosage. His advice was often sought by doctors, and rightly so. He had no way of knowing at the time that his advice to replace barbiturates with thalidomide would lead to such a tragedy, because the evidence had been concealed by the manufacturer. Some of the problems alluded to here have already been highlighted by two excellent pharmacists, Anthony Cox and @SparkleWildfire, neither of whom work in pharmacists shops. They are absolutely spot on but they seem to be in a minority among pharmacists.
The problems seem to lie mostly in retail shops. Their shelves are laden with ineffective pills and potions. And the pharmacist has every incentive to sell them. His/her income depends on it directly if it’s a privately owned pharmacy. And his/her standing with head office depends on it in chain store pharmacies. This conflict of financial interest is the prime reason why pharmacists are not qualified to form a third tier of healthcare. The avoidance of conflicts of interest among doctors was one of the great accomplishments of the NHS. In the USA there are huge scandals when, as happens repeatedly, doctors order expensive and unnecessary treatments from which they profit. It’s no consolation that such problems are creeping back in the UK as a result of the government’s vigorous efforts to sell it off.
Here are few examples of things that have gone wrong, and who is to blame. Then I’ll consider what can be done.
Ineffective medicines
In any pharmacy you can see ineffective ‘tonics’ and ‘cough medicines’, unnecessary supplements with dishonest claims and even, heaven help us, the ultimate scam, homeopathic pills.
What’s worse, if you ask a pharmacist for advice, it’s quite likely that they’ll recommend you to buy them.
|
I was amazed to discover that a number of old-fashioned ‘tonics’ and ‘cough medicines’ still have full marketing authorisation. That’s the fault of the Medicines and Healthcare Regulatory Auhority (MHRA) who are supposed to assess efficacy and totally failed to do so, Read about that in “Some medicines that don’t work. Why doesn’t the MHRA tell us honestly?” . It’s hard to blame a pharmacist for the bad advice given by the MHRA, but a good one would tell patients to save their money. |

|
Big corporate pharmacies
Companies like Boots seem to have no interest whatsoever in ethical behaviour. All that matters is sales. They provide “(mis)educational” materials that promote nonsense They advertise ridiculous made-up claims in the newspapers, which get shot down regularly by the Advertising Standards Authority, but by that time the promotion is over so they don’t give a damn. See for example, CoQ10 scam and the ASA verdict on it. And "Lactium: more rubbish from Boots the Chemists. And a more serious problem". And "The Vitamin B scam. Don’t trust Boots"
Recently the consumer magazine Which? checked 122 High Street pharmacies. They got unsatisfactory advice from 43% of them, a disastrously bad performance for people who want to be the third tier of healthcare.
|
Even that’s probably better than my own experience. Recently, when I asked a Sainsbury’s pharmacist about a herbal treatment for prostate problems, he pointed to the MHRA’s kite mark and said it must work because the MHRA approved it -he was quite unaware that you get the THR kite mark without having to present any evidence at all about efficacy. |

|
Of course that is partly the fault of the MHRA for allowing misleading labels, but nevertheless, he should have known. See “Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me” for more on how the MHRA has betrayed its own standards.
When I’ve asked Boots’ pharmacists advice about persistent diarrhoea in an infant, saying I wanted a natural remedy, I’ve usually been guided to the homeopathic display. Only once was I told firmly that I should use rehydration not homeopathy (something every good parent knows) and when I asked that good pharmacist where she’d been educated, she said in Germany (mildly surprising given the amount of junk available in German pharmacies)
Regulators
Anthony Cox, a pharmacist who has been consistently on the side of right, says
"This is something that needs to be dealt with at a regulatory and professional body by the whole profession, and I am certain we have the majority of the UK pharmacy profession on side."
But the regulator has done nothing, and it isn’t even clear that there is a majority on his side.
At a 2009 meeting of Branch Representatives of the RPS a motion was proposed:
“…registration as a pharmacist and practice as a homeopath are not compatible, and that premises registered with the Society should not be used for the promotion of homeopathy”
Although that is obviously sensible to most people, the proposal was followed by a speaker from Leicester who thought it right to keep an open mind about Avogadro’s number and the motion was defeated. So much for the "scientists on the High Street" aspiration.
There have been two major scandals surrounding homeopathy recently. Both were revealed first by bloggers, and both came to wide notice through television programs. None were noticed by the regulators, and when they were brought to the attention of the regulator, nothing effective was done.
The malaria scandal
A lot has been wriitten about this here and on other blogs e.g. here and here. The idea that sugar pills can prevent or cure malaria is so mind-bogglingly dangerous that it was condemned by the Queen’s Homeopathic Physician, Peter Fisher. It was exposed on a BBC Newsnight programme in 2006. Watch the video.
The Gentle Art of Homeopathic Killing was an article that originally appeared on the excellent Quackometer blog produced by Andy Lewis. "The Society of Homeopaths were so outraged about one of their members flouting the code of ethics so blatantly that they took immediate action. That action was, as expected, not to do anything about the ethics breach but to threaten Andy and his hosting ISP with legal action for defamation. The article is reproduced here as a public service".
Some of the people involved in this bad advice were pharmacists, Very properly they were referred to the RPS in 2006 qnd 2009, the regulator at that time. They sat on the complaint so long that eventually the RPS was replaced by the GPhC as regulator. Nothing much has happened.
The GPhC did precisely nothing. Read their pathetic response.
Homeopathy for meningitis
An equally murderous fraud, "homeopathic vaccines" by Ainsworth’s has long been targeted by bloggers. In January 2013, Samantha Smith made an excellent BBC South West programme about it. Watch it and get angry.
Anthony Pinkus, pharmacist at Ainsworths, has been referred to the then regulator, the RPS, in 2006 and 2009. It’s said that he took "remedial action", though there is little obvious change judged by the video above. No doubt some of the most incriminating stuff has been removed from his web site to hide it from the ASA. It’s safer to mislead people by word of mouth. Since the last video more complaints have been made to the GPhC. So far, nothing but silence.
Why doesn’t the regulator regulate?
This pamphlet is reproduced from the July 2011 Quackometer post, “Ainsworths Pharmacy: Casual Disregard for the Law“

|
It’s almost as though those royal warrants, enlarged on right, acted as a talisman that puts this dangerous company outside the grasp of regulators. I hope that the GPhC Council , and Duncan Rudkin (its chief executive and registrar), are not so worried about their knighthoods that they won’t risk upsetting the royal family, just to save patients from malaria and meningitis. Their CEO, Robert Nicholls is only a CBE so far. |
|
Another reason for their inaction might be that the GPhC Council members, and Duncan Rudkin (its chief executive and registrar), lack critical faculties. Perhaps they have not been very well educated? Many of them aren’t even pharmacists, but that curious breed of professional administrators who inhabit the vast number of quangos, tick their boxes and do harm. Or perhaps they are just more interested in protecting the income of pharmacists than in protecting their customers?
Education
The solution to most problems is education. But there is no real knowledge of how many pharmacists in the UK are educated in the critical assessment of evidence. A recent paper from the USA did not give cause for optimism. It’s discussed by the excellent US pharmacist, Scott Gavura, at Science-based medicine. The results are truly horrifying.
“Few students disagreed with any CAM therapy. There was the greatest support for vitamins and minerals (94%, mean 4.29) which could include the science-based use these products. But there was strong support for demonstrably ineffective treatments like acupuncture, with 64% agreeing it was acceptable. Even homeopathy, which any pharmacy student with basic medicinal chemistry skills ought to know is absurd, was supported by over 40% of students.”
If the numbers are similar in the UK, the results of the Which? magazine survey are not so surprising. And if they are held by the GPhC Council. their inaction is to be expected. We just don’t know, and perhaps someone should find out.
I suspect that sympathy for quackery may sometimes creep in through that old-fashioned discipline known as pharmacognosy. It is about the botany of medicinal plants, and it’s still taught, despite the fact that very few drugs are now extracted from plants. At times, it gets dangerously close to herbalism. For example, at the School of Pharmacy (now part of UCL) a book is used Fundamentals of Pharmacognosy and Phytotherapy by Michael Heinrich, Joanne Barnes, Simon Gibbons and Elizabeth M. Williamson, ot the Centre for Pharmacognosy and Phytotherapy at the School of Pharmacy. The introductory chapter says.
“TRADITIONAL CHINESE MEDICINE (TCM) The study of TCM is a mixture of myth and fact, stretching back well over 5000 years. At the time, none of the knowledge was written down, apart from primitive inscriptions of prayers for the sick on pieces of tortoise carapace and animal bones, so a mixture of superstition, symbolism and fact was passed down by word of mouth for centuries. TCM still contains very many remedies, which were selected by their symbolic significance rather than proven effects; however, this does not necessarily mean that they are all ‘quack’ remedies!”
Well, not necessarily. But as in most such books, there are good descriptions of the botany, more or less good accounts of the chemical constituents followed by uncritical lists of things that the herb might (or might not) do. The fact that even the US National Institutes of Health quackery branch, NCCAM, doesn’t claim that a single herbal treatment is useful tells you all you need to know.
Joanna Barnes is Associate Professor in Herbal Medicines, School of Pharmacy, University of Auckland, New Zealand. She has written a book, Herbal Medicines (“A useful book for learning holistic medicine”) that is desperately uncritical about the alleged theraputic effectiveness of plants. ("Simon Gibbons is on the editorial board of The Chinese Journal of Natural Medicine. Elizabeth Williamson is editor of the Journal of Phytotherapy Research, a journal that has a strong flavour of herbalism (take the infamous snoring remedy). These people aren’t quacks but they are dangerously tolerant of quacks.
The warning is in the title. "Phytotherapy" is the current euphemism for herbalism. It’s one of those red light words that tells you that what follows is unlikely to be critical. Exeter’s fantasy herbalist, Simon Mills, now describes himself as a phytotherapist. What more warning could you need?
Perhaps this explains why so many pharmacists are unworried by selling things that don’t work. Pharmacy education seems not to include much about the critical assessment of evidence. It should do.
Chemist and Druggist magazine certainly doesn’t help. It continually reinforces the idea that there is a debate about homepathy. There isn’t. And in one of its CPD modules Katherine Gascoigne says
"Homeopathic remedies are available, but are best prescribed by a homeopath"
Ms Gascoigne must be living on another planet.
Conclusions
The main conclusion from all of this is that the General Pharmaceutical Council is almost criminally negligent. It continues to allow pharmacists, Anthony Pinkus among them, to endanger lives. It fails to apply its own declared principles. The members of its Council, and Duncan Rudkin (its chief executive and registrar), are not doing their job.
Individual pharmacists vary a lot, from the superb to those who believe in quackery. Some, perhaps many, are embarrassed by the fact that their employer compels them to sell rubbish. It’s too much to expect that they’ll endanger their mortgage payments by speaking out about it, but the best ones will take you aside and explain that they can’t recommend it.
The GPhC itself is regulated by the Professional Standards Authority, the subject of my last post. We can’t expect anything sensible from them.
In the USA there is a shocking number of pharmacists who seem to believe in quackery. In the UK. nobody knows, though judging by their failure to vote against the daftest of all scams, homeopathy, there is no cause for complacency here.
It seems that there will have to be big improvements in pharmacy education before you can have much confidence in the quality of the advice that you get in a pharmacy.
Follow-up
Yesterday a talk was given at the School of Pharmacy, organised by the “The Centre for Homeopathic Education” (an oxymoron if there ever was one). The flyer had all the usual nonsense. Its mention of “Remedies & Tonics for Cancer Recovery” might well have breached the Cancer Act (1939). When I asked whether the amount received in room rental was sufficient to offest the damage to the reputation of the School of Pharmacy resulting from hosting a nutty (and possible illegal) event, I had the greatest difficulty in extracting any sort of response from the school’s director, Duncan Craig. I’m told that he considers “the policy on space rental to be a UCL management issue, rather than a matter of discussion on scientific ethics with a colleague”. Oh dear.
The consistent failure of ‘regulators’ to do their job has been a constant theme on this blog. There is a synopsis of dozens of them at Regulation of alternative medicine: why it doesn’t work, and never can. And it isn’t only quackery where this happens. The ineptitude (and extravagance) of the Quality Assurance Agency (QAA) was revealed starkly when the University of Wales’ accreditation of external degrees was revealed (by me and by BBC TV Wales, not by the QAA) to be so bad that the University had to shut down.
Here is another example that you couldn’t make up.
 |
 |
Yes, the Professional Standards Authority (PSA) has agreed to accredit that bad-joke pseudo-regulator, the Complementary & Natural Healthcare Council (CNHC, more commonly known as Ofquack)
Ofquack was created at the instigation of HRH the Prince of Wales, at public expense, as a means of protecting the delusional beliefs of quacks from criticism. I worked for them for a while, and know from the inside that their regulation is a bad joke.
When complaints were made about untrue claims made by ‘reflexologists’, the complaints were upheld but they didn’t even reach the Conduct and Competence committee, on the grounds that the reflexologists really believed the falsehoods that they’d been taught. Therefore, by the Humpty Dumpty logic of the CNHC, their fitness to practise was not affected by their untrue claims. You can read the account of this bizarre incident by the person who submitted the complaints, Simon Perry.
In fact in the whole history of the CNHC, it has received a large number of complaints, but only one has ever been considered by their Conduct and Competence Committee. The rest have been dismissed before they were considered properly. That alone makes their claim to be a regulator seem ridiculous.
The CNHC did tell its registrants to stop making unjustified claims, but it has been utterly ineffective in enforcing that ruling. In May 2013, another 100 complaints were submitted and no doubt they will be brushed aside too: see Endemic problems with CNHC registrants..
As I said at the time
It will be fascinating to see how the CNHC tries to escape from the grave that it has dug for itself.
If the CNHC implements properly its own code of conduct, few people will sign up and the CNHC will die. If it fails to implement its own code of conduct it would be shown to be a dishonest sham.
In February of this year (2013), I visited the PSA with colleagues from the Nightingale Collaboration. We were received cordially enough, but they seemed to be bureaucrats with no real understanding of science. We tried to explain to them the fundamental dilemma of the regulation of quacks, namely that no amount of training will help when the training teaches things that aren’t true. They were made aware of all of the problems described above. But despite that, they ended up endorsing the CNHC.
How on earth did the PSA manage to approve an obviously ineffective ‘regulator’?
The job of the PSA is said to be “. . . protecting users of health and social care services and the public”. They (or at least their predecessor, the CHRE), certainly didn’t do that during the saga of the General Chiropractic Council.
The betrayal of reason is catalogued in a PSA document [get local copy]. Here is some nerdy detail.
It is too tedious to go through the whole document, so I’ll deal with only two of its many obvious flaws, the sections that deal with the evidence base, and with training.
The criteria for accreditation state
Standard 6: the organisation demonstrates that there is a defined knowledge base underpinning the health and social care occupations covered by its register or, alternatively, how it is actively developing one. The organisation makes the defined knowledge base or its development explicit to the public.
The Professional Standards Authority recognises that not all disciplines are underpinned by evidence of proven therapeutic value. Some disciplines are subject to controlled randomized trials, others are based on qualitative evidence. Some rely on anecdotes. Nevertheless, these disciplines are legal and the public choose to use them. The Authority requires organisations to make the knowledge base/its development clear to the public so that they may make informed decisions.
Since all 15 occupations that are “regulated” by the CNHC fall into the last category. they “rely on anecdotes”, you would imagine the fact that “The Authority requires organisations to make the knowledge base/its development clear to the public” would mean that the CNHC was required to make a clear statement that reiki, reflexology etc are based solely on anecdote. Of course the CNHC does no such thing. For example, the CNHC’s official definition of reflexology says
Reflexology is a complementary therapy based on the belief that there are reflex areas in the feet and hands which are believed to correspond to all organs and parts of the body
There is, of course, not the slightest reason to think such connections exist, but the CNHC gives no hint whatsoever of that inconvenient fact. The word “anecdote” is used by the PSA but occurs nowhere on the CNHC’s web site.
It is very clear that the CNHC fails standard 6.
But the PSA managed to summon up the following weasel words to get around this glaring failure:
“The professional associations (that verify eligibility for CNHC registration) were actively involved in defining the knowledge base for each of the 15 professions. The Panel further noted that Skills for Health has lead responsibility for writing and reviewing the National Occupational Standards (NOS) for the occupations CNHC registers and that all NOS have to meet the quality criteria set by the UK Commission for Employment and Skills (UKCES), who are responsible for the approval of all NOS across all industry sectors. The Panel considered evidence provided and noted that the applicant demonstrated that there is a defined knowledge base underpinning the occupations covered by its registers. The knowledge base was explicit to the public”.
The PSA, rather than engaging their own brains, simply defer to two other joke organisations, Skills for Health and National Occupational Standards. But it is quite obvious that for things like reiki, reflexology and craniosacral therapy, the “knowledge base” consists entirely of made-up nonsense. Any fool can see that (but not, it seems, the PSA).
Skills for Health lists made-up, HR style, “competencies” for everything under the sun. When I got them to admit that their efforts on distance-healing etc had been drafted by the Prince of Wales’ Foundation, the conversation with Skills for Health became surreal (recorded in January 2008)
DC. Well yes the Prince of Wales would like that. His views on medicine are well known, and they are nothing if not bizarre. Haha are you going to have competencies in talking to trees perhaps?
“You’d have to talk to LANTRA, the land-based organisation for that.”
DC. I’m sorry, I have to talk to whom?
“LANTRA which is the sector council for the land-based industries uh, sector, not with us sorry . . . areas such as horticulture etc.”
DC. We are talking about medicine aren’t we? Not horticulture.
“You just gave me an example of talking to trees, that’s outside our remit ”
You couldn’t make it up, but it’s true. And the Professional Standards Authority rely on what these jokers say.
The current Skills for Health entry for reflexology says
“Reflexology is the study and practice of treating reflex points and areas in the feet and hands that relate to corresponding parts of the body. Using precise hand and finger techniques a reflexologist can improve circulation, induce relaxation and enable homeostasis. These three outcomes can activate the body’s own healing systems to heal and prevent ill health.”
This is crass, made-up nonsense. Of course there are no connections between “areas in the feet and hands that relate to corresponding parts of the body” and no reason to think that reflexology is anything more than foot massage. That a very expensive body, paid for by you and me, can propagate such preposterous nonsense is worrying. That the PSA should rely on them is even more worrying.
National Occupational Standards is yet another organisation that is utterly dimwitted about medical matters, but if you look up reflexology you are simply referred to Skills for Health, as above.
UK Commission for Employment and Skills
(UKCES) is a new one on me. The PSA says that “the UK Commission for Employment and Skills (UKCES), who are responsible for the approval of all NOS across all industry sectors” It is only too obvious that the UKCES leadership team have failed utterly to do their job when it comes to made-up medicine. None of them know much about medicine. It’s true that their chairman did once work for SmithKline Beecham, but as a marketer of Lucozade, a job which anyone with much knowledge of science would not find comfortable..
You don’t need to know much medicine to spot junk. I see no excuse for their failure.
The training problem.
The PSA’s criteria for accreditation say
Standard 9: education and training
The organisation:
9a) Sets appropriate educational standards that enable its registrants to practise competently the occupation(s) covered by its register. In setting its standards the organisation takes account of the following factors:
- The nature and extent of risk to service users and the public
- The nature and extent of knowledge, skill and experience required to provide
service users and the public with good quality careand later
9b) Ensures that registrants who assess the health needs of service users and provide any form of care and treatment are equipped to:
- Recognise and interpret clinical signs of impairment
- Recognise where a presenting problem may mask underlying pathologies
- Have sufficient knowledge of human disease and social determinants of health to identify where service users may require referral to another health or social care professional.
Anyone who imagines for a moment that a reflexologist or a craniosacral therapist is competent to diagnose a subarachnoid haemorrhage or malaria must need their head examining. In any case, the CNHC has already admitted that their registrants are taught things that aren’t true, so more training presumably means more inculcation of myths.
So how does the PSA wriggle out of this? Their response started
“The Panel noted that practitioners must meet, as a minimum, the National Occupational Standards for safe and competent practice. This is verified by the professional associations, who have in turn provided written undertakings to CNHC affirming that there are processes in place to verify the training and skills outcomes of their members to the NOS”
Just two problems there. The NOS standards themselves are utterly delusional. And checking them is left to the quacks themselves. To be fair, the PSA weren’t quite happy with this, but after an exchange of letters, minor changes enabled the boxes to be ticked and the PSA said “The Panel was now satisfied from the evidence provided, that this Standard had been
met”.
What’s wrong with regulators?
This saga is typical of many other cases of regulators doing more harm than good. Regulators are sometimes quacks themselves, in which case one isn’t surprised at their failure to regulate.
But organisations like the Professional Standards Authority and Skills for Health are not (mostly) quacks themselves. So how do they end up giving credence to nonsense? I find that very hard to comprehend, but here are a few ideas.
(1) They have little scientific education and are not really capable of critical thought
(2) Perhaps even more important, they lack all curiosity. It isn’t very hard to dig under the carapace of quack organisations, but rather than finding out for themselves, the bureaucrats of the PSA are satisfied by reassuring letters that allow them to tick their boxes and get home.
(3) A third intriguing possibility is that people like the PSA yield to political pressure. The Department of Health is deeply unscientific and clearly has no idea what to do about alternative medicine. They have still done nothing at all about herbal medicine, traditional Chinese medicine or homeopathy, after many years of wavering. My guess is that they see the CNHC as an organisation that gives the appearance that they’ve done something about reiki etc. I wonder whether they applied pressure to the PSA to accredit CNHC, despite it clearly breaking their own rules. I have sent a request under the Freedom of Information Act in an attempt to discover if the Department of Health has misbehaved in the way it did when it attempted to override NHS Choices.
The responsibility for this cock-up has to rest squarely on the shoulders of the PSA’s director, Harry Cayton. He was director of the CHRE from which PSA evolved and is the person who so signally failed to do anything about the General Chiropractic Council fiasco,
What can be done?
This is just the latest of many examples of regulators who not only fail to help but actually do harm by giving their stamp of approval to mickey mouse organisations like the CNHC. Most of the worst quangos survived the “bonfire of the quangos”.. The bonfire should have started with the PSA, CNHC and Skills for Health. They cost a lot and do harm.
There is a much simpler answer. There is a good legal case that much of alternative medicine is illegal. All one has to do is to enforce the existing law. Nobody would object to quacks if they stopped making false claims (though whether they could stay in business if they stopped exaggerating is debatable). There is only one organisation that has done a good job when it comes to truthfulness. That is the Advertising Standards Authority. But the ASA can do nothing apart from telling people to change the wording of their advertisements, and even that is often ignored.
The responsibility for enforcing the Consumer Protection Law is Trading Standards. They have consistently failed to do their job (see Medico-Legal Journal, Rose et al., 2012. “Spurious Claims for Health-care Products“.
If they did their job of prosecuting people who defraud the public with false claims, the problem would be solved.
But they don’t, and it isn’t.
Follow-up
The indefatigable Quackometer has wriiten an excellent account of the PSA fiasco
Despite the First Amendment in the US and a new Defamation Act in the UK, fear of legal threats continue to suppress the expression of honest scientific opinion.
I was asked by Nature Medicine (which is published in the USA) to write a review of Paul Offit’s new book. He’s something of a hero, so of course I agreed. The editor asked me to make some changes to the first draft, which I did. Then the editor concerned sent me this letter.
|
Thank you for the revised version of the book review.
The chief editor of the journal took a look at your piece, and he thought that it would be a good idea to run it past our legal counsel owing to the strong opinions expressed in the piece in relation to specific individuals. I regret to say that the lawyers have advised us against publishing the review. |
After that I tried the UK Conversation. They had done a pretty good job with my post on the baleful influence of royals on medicine. They were more helpful then Nature Medicine, but for some reason that I can’t begin to understand, they insisted that I should not name Nature Medicine, but to refer only to "a leading journal". And they wanted me not to name Harvard in the last paragraph. I’m still baffled about why. But it seemed to me that editorial interference had gone too far, so rather than have an editor re-write my review, I withdrew it.
It is precisely this sort of timidity that allows purveyors of quackery such success with their bait and switch tactics. The fact that people seem so terrified to be frank must be part of the reason why Harvard, Yale and the rest have shrugged their shoulders and allowed nonsense medicine to penetrate so deeply into their medical schools. It’s also why blogs now are often better sources of information than established journals.
Here is the review. I see nothing defamatory in it.
Do You Believe in Magic? The Sense and Nonsense of Alternative Medicine
|
Paul A. Offit Reviewed by David Colquhoun Research Professor of Pharmacology, UCL. |

|
Here’s an odd thing. There is a group of people who advocate the silly idea that you can cure all ills by stuffing yourself with expensive pills, made by large and unscrupulous Pharma companies. No, I’m not talking about pharmacologists or doctors or dietitians. They mostly say that stuffing yourself with pills is often useless and sometimes harmful, because that’s what the evidence says .
Rather, the pill pushers are the true believers in the alternative realities of the “supplement” industry. They seem blithely unaware that the manufacturers are mostly the same big pharma companies that they blame for trying to suppress “natural remedies”. Far from trying to suppress them, pharma companies love the supplement industry because little research is needed and there are few restrictions on the claims that can be made.
Paul Offit’s excellent book concentrates on alternative medicine in the USA, with little mention of the rest of the world. He describes how American pork barrel politics have given supplement hucksters an almost unrestricted right to make stuff up.
Following the thalidomide tragedy, which led to birth defects in babies in the 1950s and 60s, many countries passed laws that required evidence that a drug was both effective and safe before it could be sold. This was mandate by the Kefauver-Harris amendment (1961) in the USA and the Medicines Act (1968) in the UK. Laws like that upset the quacks, and in the UK the quacks got a free pass, a ‘licence of right‘, largely still in existence.
|
In order to sell a herbal concoction in the UK you need to present no evidence at all that it works, just evidence of safety, in return for which you get a reassuring certification mark and freedom to use misleading brand names and labels. |
 Tradional herbal mark |
In the USA the restrictions didn’t last long. Offit describes how a lobby group for vitamin sellers, the National Health Federation, had a board made up of quacks, some of whom, according to Offit (page 73) had convictions. They found an ally in Senator William Proxmire who introduced in 1975 an amendment that banned the Food and Drugs Administration (FDA) from regulating the safety of megavitamins. Tragically, this bill was even supported by the previously-respected scientist Linus Pauling. Offit tells us that “to Proxmire” became a verb meaning to obstruct science for political gain.
The author then relates how the situation got worse with the passage of the Dietary Supplement Health and Education Act (DSHEA) in 1994. It was passed with the help of ex-vitamin salesman Senator Orin Hatch and lots of money from the supplement industry.
This act iniquitously defined a “supplement” as “a product intended to supplement the diet that bears or contains one or more of the following ingredients: a vitamin, a mineral, an herb or other botanical, or an amino acid”. At a stroke, herbs were redefined as foods. There was no need to submit any evidence of either efficacy or even of safety, before marketing anything. All a manufacturer had to do to sell almost any herbal drug or megadose vitamin was to describe it as a “dietary supplement”. The lobbying to get this law through was based on appealing to the Tea Party tendency –get the government’s hands off our vitamins. And it was helped by ‘celebrities’ such as Sissy Spacek and Mel Gibson (it’s impossible to tell whether they really believed in the magic of vitamins, or whether they were paid, or had Tea Party sympathies).
Offit’s discussion of vaccination is a heartbreaking story of venom and misinformation. As co-inventor of the first rotavirus vaccine he’s responsible for saving many lives around the world. But he, perhaps more than anyone, suffered from the autism myth started by the falsified work of Andrew Wakefield.
The scientific community took the question seriously and soon many studies showed absolutely no link between vaccination and autism. But evidence did not seem to interest the alternative world. Rather than Offit being lauded as a saver of children’s lives, he describes how he was subjected to death threats and resorted to having armed guards at meetings.
Again, Offit tells us how celebrities were able to sway public opinion For example (chapter 6), the actress Jenny McCarthy and talk-show hostess Oprah Winfrey promoted, only too successfully, the vaccine-autism link despite abundant evidence that it didn’t exist, and promoted a number of theories that were not supported by any evidence, such as the idea that autism can be “cured” by mega-doses of vitamins and supplements.
Of course vaccines like the one for rotavirus can’t be developed without pharmaceutical companies because, as Offit says, only they "have the resources and expertise to make a vaccine. We can’t make it in our garage". When the Children’s Hospital of Philadelphia sold its royalty stake in the rotavirus vaccine for $182 million, Offit received an undisclosed share of the intellectual property, “in the millions ”.
That’s exactly what universities love. We are encouraged constantly to collaborate with industry, and, in the process, make money for the university. It’s also what Wakefield, and the Royal Free Hospital where he worked, hoped to do. But sadly, these events led to Offit being called names such as “Dr Proffit” and “Biostitute” (to rhyme with “prostitute”) by people like Jenny McCarthy and Robert F. Kennedy Jr. The conspiritorialist public lapped up this abuse, but appeared not to notice that many quacks have become far richer by peddling cures that do not work.
One lesson from this sad story is that we need to think more about the potential for money to lead to good science being disbelieved, and sometimes to corrupt science.
Everyone should buy this book, and weep for the gullibility and corruption that it describes.
I recommend it especially to the deans of US Medical schools, from Harvard downwards, who have embraced “integrative medicine” departments. In doing so they have betrayed both science and their patients.
Abraham Flexner, whose 1910 report first put US medicine on a sound scientific footing, must be turning in his grave.

|

|
Follow-up
30 August 2013
Quack lobby groups got a clause inserted into Obamacare that will make any attempt to evaluate whether a treatment actually works will leave insurance companies open to legal action for "discrimination".
"Discrimination? Yes! We must not allow the government to exclude health care providers just because those providers don’t cure anything."
The latest piece of well-organised corporate corruption by well-funded lobbyists is revealed by Steven Salzberg, in Forbes Magazine. The chaos in the US health system makes one even more grateful for the NHS and for the evaluation of effectiveness of treatments by NICE.
This article has appeared, in nearly identical form, on the UK Conversation . You can leave comments there or here.
A constitutional monarch is purely ceremonial and plays no part in politics. Well actually in the UK it isn’t quite as simple as that. The first problem is that we have no constitution. Things haven’t changed much since the 19th century when Walter Bagehot said "the Sovereign has, under a constitutional monarchy… three rights—the right to be consulted, the right to encourage, the right to warn."
These are not inconsiderable powers in a country which is meant to be run by elected representatives. But nobody knows how these powers are used: it is all done in secret. Well, almost all. Charles, Prince of Wales, has been unusually public in expressing his views. He told a conference at St James’s Palace “I was accused once of being the enemy of the Enlightenment” “I felt proud of that.” That’s a remarkable point of view for someone who, if he succeeds, will become the patron of that product of the age of enlightenment, the Royal Society.
I have no doubt that Prince Charles means well. He can’t be blamed for his lack of education. But his views on medicine date from a few centuries ago, and he has lost no opportunity to exploit his privileged position to proclaim them.
Euphemisms for quackery
He set up the Prince’s Foundation for Integrated Health (PFIH) to promote his views. ( “Integrated”, in this context, is, of course, just the latest euphemism for “alternative” or “quack”.) When the Foundation collapsed because of a financial scandal in 2010, it was replaced by the “College of Medicine”. The name changed, but not the people behind it. Initially this phoenix was to be named the “College of Integrated Health”, but by this time the prince’s views on medicine had become sufficiently discredited that the word “integrated” was quickly dropped. This might be thought less than frank, but it is just employment of the classic bait and switch technique, beloved by used car salesmen.
His views were well publicised in a PFIH publication, “Complementary Healthcare: a Guide for Patients”. That volume either omitted or misrepresented the evidence about the one question that matters most to patients – does the treatment work or not? It caused me to write a much shorter, but more accurate, version, the Patients’ Guide to Magic Medicine. The PFIH guide was arguably a danger to public health. When, very properly, it was criticised by Edzard Ernst, a letter was sent from from the prince’s private secretary to Ernst’s vice-chancellor, Steve Smith. Instead of defending Ernst’s public spirited action, Smith instituted disciplinary proceedings against Ernst that lasted for a year. The prince had intervened directly in the affairs of the university. Steve Smith was rewarded with a knighthood in 2011.
None of this criticism has dimmed the prince’s enthusiasm for barmy medical ideas. He is well known to write many letters to government ministers to try to persuade them to adopt his ideas in a whole range of areas. In July 2013, the Minister of Health, Jeremy Hunt, visited the prince at Clarence House. The visit was reported to be to persuade the minister to defend homeopathy, though it was more likely to have been to press the case to confer a government stamp of approval on herbalists and traditional Chinese Medicine practitioners by giving them statutory regulation. This is a matter that was recently raised again in parliament by Charles’ greatest ally, David Tredinnick MP (Con, Bosworth) who got into trouble for charging astrology software to expenses. We shall never know what pressure was applied. A ruling of the Information Commissioner judged, reasonably enough, that there was public interest in knowing what influences were being brought to bear on public policy. But the Attorney General overruled the judgement on the grounds that “Disclosure of the correspondence could damage The Prince of Wales’ ability to perform his duties when he becomes King.” That, of course, is exactly what we are worried about.
Influence on politics
The prince’s influence seems to be big in the Department of Health (DH). He was given £37,000 of taxpayers’ money to produce his guide, and an astonishing £900,000 to prepare the ground for the setting up of the hapless self-regulator, the Complementary and Natural Healthcare Council (CNHC, also known as Ofquack). When NHS Choices (itself set up by DH to assess evidence) tried to rewrite its web page about that most discredited of all forms of quackery, homeopathy, officials in DH referred the new advice to Michael Dixon, the medical director of the Prince’s Foundation and, were it not for the Freedom of Information act, the DH would have caused inaccurate information to be provided. The DH has a chief medical officer and two scientific advisors, but prefers to take the advice of the Prince of Wales.
The Prince of Wales’ business, Duchy Originals, has been condemned by the Daily Mail, (of all places) for selling unhealthy foods. And when his business branched into selling quack “detox” and herbal nonsense he found himself censured by both the MHRA and the Advertising Standards Authority (ASA) for making unjustifiable medical claims for these products.
Ainsworth’s homeopathic pharmacy is endorsed by both Prince Charles and the Queen: it has two Royal Warrants. They sell “homeopathic vaccines” for meningitis, measles, rubella and whooping cough. These “vaccines” contain nothing whatsoever so they are obviously a real danger to public health. Despite the fact that Ainsworth’s had already been censured by the ASA in 2011 for selling similar products, Ainsworth’s continued to recommend them with a “casual disregard for the law”. The regulator (the MHRA) failed to step in to stop them until it was eventually stirred into action by a young BBC reporter, Sam Smith, made a programme for BBC South West. Then, at last, the somnolent regulator was stirred into action. The MHRA “told Ainsworths to stop advertising a number of products” (but apparently not to stop making them or selling them). They still sell Polonium metal 30C and Swine Meningitis 36C, and a booklet that recommends homeopathic “vaccination”. Ainsworth’s sales are no doubt helped by the Royal Warrants. The consequence is that people may die of meningitis. In 2011, the MHRA Chief Executive Professor Kent Woods, was knighted.
It runs in the family
The Prince of Wales is not the only member of the royal family to be obsessed with bizarre forms of medicine. The first homeopath to the British royal family, Frederick Quin, was a son of the Duchess of Devonshire (1765-1824). Queen Mary (1865-1953), wife of King George V, headed the fundraising efforts to move and expand the London Homeopathic Hospital.
King George VI was so enthusiastic that in 1948 conferred the royal title on the London Homeopathic Hospital. The Queen Mother loved homeopathy too (there is no way to tell whether this contributed to her need for a colostomy in the 1960s).
The present Queen’s homeopathic physician is Peter Fisher, who is medical director of what, until recently was called the Royal London Homeopathic Hospital (RLHH). In 2010 that hospital was rebranded as the Royal London Hospital for Integrated Medicine (RLHIM) in another unsubtle bait and switch move.
|
The RLHIM is a great embarrassment to the otherwise excellent UCLH Trust. It has been repeatedly condemned by the Advertising Standards Authority for making false claims. As a consequence, it has been forced to withdraw all of its patient information. The patron of the RLHIM is the Queen, not the Prince of Wales. It is hard to imagine that this anachronistic institution would still exist if it were not for the influence, spoken or unspoken, of the Queen. Needless to say we will never be told. |
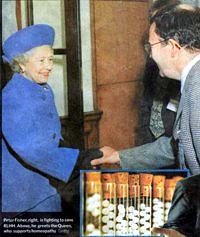 The Queen and Peter Fisher Observer 8 April 2007 |
The attorney general, while trying to justify the secrecy of Charles’ letters, said
“It is a matter of the highest importance within our constitutional framework that the Monarch is a politically neutral figure”.
Questions about health policy are undoubtedly political, and the highly partisan interventions of the prince in the political process make his behaviour unconstitutional. They endanger the monarchy itself. Whether that matters depends on how much you value tradition and how much you value the tourist business generated by the Gilbert & Sullivan flummery at which royals excel.
The least that one can ask of the royal family is that they should not endanger the health of the nation. If I wanted to know the winner of the 2.30 at Ascot, I’d ask a royal. For any question concerning science or medicine I’d ask someone with more education.
Here is some more interesting reading
Michael Baum’s “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong”
Gerald Weissman’s essay Homeopathy: Holmes, Hogwarts, and the Prince of Wales.
Channel 4 TV documentary HRH “meddling in politics”
Observer April 2007 "Royals’ favoured hospital at risk as homeopathy backlash gathers pace. The Queen loves it. But alternative medicine centre’s future looks uncertain as more NHS trusts axe funding"
Follow-up
A constant theme of this blog is that the NHS should not pay for useless treatments. By and large, NICE does a good job of preventing that. But NICE has not been allowed by the Department of Health to look at quackery.
I have the impression that privatisation of many NHS services will lead to an increase in the provision of myth-based therapies. That is part of the "bait and switch" tactic that quacks use in the hope of gaining respectability. A prime example is the "College of Medicine", financed by Capita and replete with quacks, as one would expect since it is the reincarnation of the Prince’s Foundation for Integrated Health.
One such treatment is acupuncture. Having very recently reviewed the evidence, we concluded that "Acupuncture is a theatrical placebo: the end of a myth". Any effects it may have are too small to be useful to patients. That’s the background for an interesting case study.
A colleague got a very painful frozen shoulder. His GP referred him to the Camden & Islington NHS Trust physiotherapy service. That service is now provided by a private company, Connect Physical Health.
That proved to be a big mistake. The first two appointments were not too bad, though they resulted in little improvement. But at the third appointment he was offered acupuncture. He hesitated, but agreed, in desperation to try it. It did no good. At the next appointment the condition was worse. After some very painful manipulation, the physiotherapist offered acupuncture again. This time he refused on the grounds that "I hadn’t noticed any effect the first time, because there is no evidence that it works and that I was concerned by her standards of hygiene". The physiotherapist then became "quite rude" and said that she would put down that the patient had refused treatment.
The lack of response was hardly surprising. NHS Evidence says
"There is no clinical evidence to show that other treatments, such as transcutaneous electrical nerve stimulation (TENS), Shiatsu massage or acupuncture are effective in treating frozen shoulder."
In fact it now seems beyond reasonable doubt that acupuncture is no more than a theatrical placebo.
According to Connect’s own web site “Our services are evidence-based”. That is evidently untrue in this case, so I asked them for the evidence that acupuncture was effective.
I’d noticed that in other places, Connect Physical Health also offers the obviously fraudulent craniosacral therapy (for example, here) and discredited chiropractic quackery. So I asked them about the evidence for their effectiveness too.
This is what they said.
|
Many thanks for your comments via our web site. In response, we thought you might like to access the sources for some of the evidence which underpins our MSK services: Integrating Evidence-Based Acupuncture into Physiotherapy for the Benefit of the Patient – you can obtain the information you require from www.aacp.org.uk The General Chiropractic Council www.gcc-uk.org/page.cfm We have also attached a copy of the NICE Guidelines. |
So, no Cochrane reviews, no NHS Evidence. Instead I was referred to the very quack organisations that promote the treatments in question, the Acupuncture Association of Chartered Physiotherapists, and the totally discredited General Chiropractic Council.
The NICE guidelines that they sent were nothing to do with frozen shoulder. They were the guidelines for low back pain which caused such a furore when they were first issued (and which, in any case, don’t recommend chiropractic explicitly).
When I pointed out these deficiencies I got this.
|
Your email below has been forwarded to me. I am sorry if you feel that that that information we pointed you towards to enable you to make your own investigations into the evidence base for the services provided by Connect Physical Health and your hospital did not meet with your expectations. ‘ ‘ ‘ Please understand that our NHS services in Camden were commissioned by the Primary Care Trust. The fully integrated MSK service model included provision for acupuncture and other manual therapy provided by our experienced Chartered Physiotherapists. If you have any problems with the evidence base for the use of acupuncture or manual therapy within the service, which has been commissioned on behalf of the GPs in Camden Borough, then I would politely recommend that you direct your observations to the clinical commissioning authorities and other professional bodies who do spend time evidencing best practice and representing the academic arguments. I am sure they will be pleased to pick up discussions with you about the relative merits of the interventions being procured by the NHS. Yours sincerely, Mark Mark Philpott BSc BSc MSc MMACP MCSP
Head of Operations, Community MSK Services Connect Physical Health 35 Apex Business Village Cramlington Northumberland NE23 7BF |
So, "don’t blame us, blame the PCT". A second letter asked why they were shirking the little matter of evidence.
|
In response to your last email, I would like to say that Connect does not wish to be drawn into a debate over two therapeutic options (acupuncture and craniosacral therapy) that are widely practiced [sic] within and outside the NHS by very respectable practitioners. You will be as aware, as Connect is, that there are lots of treatments that don’t have a huge evidence base that are practiced in mainstream medicine. Connect has seen many carefully selected patients helped by acupuncture and manual therapy (craniosacral therapy / chiropractic) over many years. Lack of evidence doesn’t mean they don’t work, just that benefit is not proven. Furthermore, nowhere on our website do we state that ALL treatments / services / modalities that Connect offer are ‘Evidence Based’. We do however offer many services that are evidence based, where the evidence exists. We aim to offer ‘choice’ to patients, from a range of services that are safe and delivered by suitably trained professionals and practitioners in line with Codes of Practice and Guidelines from the relevant governing bodies. Connect’s service provision in Camden is meticulously assessed and of a high standard and we are proud of the services provided. |
This response is so wrong, on so many levels, that I gave up on Mr Philpott at this point. At least he admitted implicitly that all of their treatments are not evidence-based. In that case their web site needs to change that claim.
If, by "governing bodies" he means jokes like the GCC or the CNHC then I suppose the behaviour of their employees is not surprising. Mr Philpott is evidently not aware that "craniosacral therapy" has been censured by the Advertising Standards Authority. Well he is now, but evidently doesn’t seem to give a damn.
Next I wrote to the PCT and it took several mails to find out who was responsible for the service. Three mails produced no response so I sent a Freedom of Information Act request. In the end I got some
"Connect PHC provide the Community musculoskeletal service for Camden. The specification for the service specifically asks for the provision of evidence based management and treatments see paragraph on Governance page 14 of attached.. Patients are treated with acupuncture as per the NICE Guidelines (May 2009) for the management of low back pain … . .. Chiropractors are not employed in the service and craniosacral therapy is not provided as part of the service either."
Another letter, pointing out that they were using acupuncture for things other than low back pain got no more information. They did send a copy of the contract with Connect. It makes no mention whatsoever of alternative treatments. It should have done, so part of the responsibility for the failure must lie with the PCT.
The contract does, however, say (page 18)
The service to be led by a lead clinician/manager who can effectively demonstrate ongoing and evidence-based development of clinical guidelines, policies and protocols for effective working practices within the service
In my opinion, Connect Physical Health are in breach of contract
Another example of Connect ignoring evidence
The Connect Physical Health web site has an article about osteoarthritis of the knee
Physiotherapy can be extremely beneficial to help to reduce the symptoms of OA. Treatments such as mobilizations, rehab exercises, acupuncture and taping can help to reduce pain, increase range of movement, increase muscle strength and aid return to functional activities and sports.
There is little enough evidence that physiotherapy does any of these things, but at least it is free of mystical mumbo-jumbo. Although at one time the claim for acupuncture was thought to have some truth, the 2010 Cochrane review concludes otherwise
Sham-controlled trials show statistically significant benefits; however, these benefits are small, do not meet our pre-defined thresholds for clinical relevance, and are probably due at least partially to placebo effects from incomplete blinding.
This conclusion is much the same as has been reached for acupuncture treatments of almost everything. Two major meta-analyses come to similar conclusions. Madsen Gøtzsche & Hróbjartsson (2009) and Vickers et al (2012) both conclude that if there is an effect at all (dubious) then it is too small to be noticeable to the patient. (Be warned that in the case of Vickers et al. you need to read the paper itself because of the spin placed on the results in the abstract.). These papers are discussed in detail in our recent paper.
Why is Connect Physical Health not aware of this?
Their head of operations told me (see above) that
"Connect does not wish to be drawn into a debate [about acupuncture and craniosacral therapy]".
That outlook was confirmed when I left a comment on their osteoarthritis post. This is what it looked like almost a month later.

Guess what? The comment has never appeared..
The attitude of Connect Physical Health to evidence is simply to ignore it if it gets in the way of making money, and to censor any criticism.
What have Camden NHS done about it?
The patient and I both complained to Camden NHS in August 2012. At first, they simply forwarded the complaints to Connect Physical Health with the unsatisfactory results shown above. It took until May 2013 to get any sort of reasonable response. That seems a very long time. In fact by the time the response arrived the PCT had been renamed a Clinical Commissioning Group (CCG) because of the vast top-down reorganisation inposed by Lansley’s Health and Social Care Act.
On 8 May 2013, this response was sent to the patient, Here is part of it.
|
I have received your email of complaint from the NHSNCL complaints department regarding your care. You raise some very clear concerns and I will attempt to address these in order. 1) The fact that you felt pressurised into having acupuncture is a concern as everybody should be given a choice. As part of the informed consent relating to acupuncture you should have been told about the treatment, it’s [sic] benefits and risks and then you sign to confirm you are happy to proceed. I understand that this was the case in your situation but I have reinforced that the consent is important and must be adhered to by the provider Connect Physical Health. There are clear standards of clinical practice that all Chartered Physiotherapists must follow which I will discuss further with the Connect Camden team Manager Nick Downing. I do disagree with you around acupuncture; there is no conclusive evidence for acupuncture in frozen shoulder but I have referenced a systematic review which concludes the studies were too small to draw any conclusions although shoulder function was significantly improved at 4 weeks (Green S et al. Acupuncture for shoulder pain. Cochrane Database Syst Rev 2005; 18: CD005319). There is a growing body of evidence supporting the use of acupuncture and until such time as there is specific evidence against it I don’t think we would be absolutely against the practice of this modality alongside other treatments. .Best wishes Strategy and Planning Directorate |
This response raises more questions than it answers.
For example, what is "informed consent" worth if the therapist is his/herself misinformed about the treatment? It is the eternal dilemma of alternative medicine that it is no use referring to well-trained practitioners, when their training has inculcated myths and untruths.
There is not a "growing body of evidence supporting the use of acupuncture". Precisely the opposite is true.
And the statement "until such time as there is specific evidence against it I don’t think we would be absolutely against the practice of this modality alongside" betrays a basic misunderstanding of the scientific process.
So I sent the writer of this letter a reprint of our paper, "Acupuncture is a theatrical placebo: the end of a myth" (the blog version alone has had over 12,000 page views). A few days later we had an amiable lunch together and we had a constructive discussion about the problems of deciding what should be commissioned and what shouldn’t.
It seems to me to be clear that CCGs should take better advice before boasting that they commission evidence-based treatments.
Postscript
Stories like this are worrying to the majority of physiotherapists who don’t go in for mystical mumbo-jumbo of acupuncture. One of the best is Neil O’Connell who blogs at BodyInMind. He tweeted
Physio fail, sigh RT@david_colquhoun: Yet more #acupuncture. Sold to the NHS by private contractor @ConnectPHC http://t.co/HylkwMCVTh
— Neil O'Connell (@NeilOConnell) June 10, 2013
It isn’t clear how many physiotherapists embrace nonsense, but the Acupuncture Association of Chartered Physiotherapists has around 6000 members, compared with 47,000 chartered physiotherapists (AACP), so it’s a smallish minority. The AACP claims that it is “Integrating Evidence-Based Acupuncture into Physiotherapy”. Like most politicians, the term “evidence-based” is thrown around with gay abandon. Clearly they don’t understand evidence.
Follow-up
12 June 2013
The Advertising Standards Authority has, one again, upheld complaints against the UCLH Trust, for making false claims in its advertising. This time, appropriately, it’s about acupuncture. Just about everything in their advertising leaflets was held to be unjustifiable. They’ve been in trouble before about false claims for homeopathy, hypnosis and craniosacral "therapy".
Of course all of these embarrassments come from one very small corner of the UCLH Trust, the Royal London Hospital for Integrated Medicine (previously known as the Royal London Homeopathic Hospital).
Why is it tolerated in an otherwise excellent NHS Trust? Well, the patron is the Queen herself (not Charles, aka the Quacktitioner Royal), She seems to exert more power behind the scenes than is desirable in In a constitutional monarchy
29 June 2013
I wrote to Dr Gill Gaskin about the latest ASA judgement against RLHIM. She is the person at the UCLH Trust who has responsibility for the quack hospital. She previously refused to do anything about the craniosacral nonsense that is promoted there. This time the ASA seems to have stung them into action at long last. I was told
|
In response to your question about proposed action: All written information for patients relating to the services offered by the Royal London Hospital for Integrated Medicine are being withdrawn for review in the light of the ASA’s rulings (and the patient leaflets have already been withdrawn). It will be reviewed and modified where necessary item by item, and only reintroduced after sign-off through the Queen Square divisional clinical governance processes and the Trust’s patient information leaflet team. With best wishes Gill Gaskin Dr Gill Gaskin |
It remains to be seen whether the re-written information is accurate or not.
The rules for advertising
The Advertising Standards Authority gives advice for advertisers about what’s permitted and what isn’t.
Acupuncture The CAP advice
Craniosacral therapy The CAP advice
Homeopathy The CAP advice and 2013 update
Chiropractic The CAP advice.
Here is a record of a couple of recent newspaper pieces. Who says the mainstream media don’t matter any longer? Blogs may be in the lead now when it comes to critical analysis. The best blogs have more expertise and more time to read the sources than journalists. But the mainstream media get the message to a different, and much larger, audience.
The Observer ran a whole page interview with me as part of their “Rational Heroes” series. I rather liked their subtitle [pdf of article]
“Professor of pharmacology David Colquhoun is the take-no-prisoners debunker of pseudoscience on his unmissable blog”
It was pretty accurate apart from the fact that the picture was labelled as “DC in his office”. Actually it was taken (at the insistence of the photographer) in Lucia Sivilotti’s lab.

Photo by Karen Robinson.
The astonishing result of this was that on Sunday the blog got a record 24,305 hits. Normally it gets 1,000-1,400 hits a day . between posts, fewer on Sunday, and the previous record was around 7000/day
A week later it was still twice normal. It remains to be seen whether the eventual plateau stays up.
I also gained around 1000 extra followers on twitter, though some dropped away quite soon, and 100 or so people signed for email updates. The dead tree media aren’t yet dead. I’m happy to say.
3 June 2013
Perhaps as a result of the foregoing piece, I got asked to write a column for The Observer, at barely 48 hours notice. This is the best I could manage in the time. The web version has links.
This attracted the usual "it worked for me" anecdotes in the comments, but I spent an afternoon answering them. It seems important to have a dialogue, not just to lecture the public. In fact when I read a regular scientific paper, I now find myself looking for the comment section. That may say something about the future of scientific publishing.
It is for others to judge how succesfully I engage with the public, but I was quite surprised to discover that UCL’s public engagement unit, @UCL_in_public, has blocked me on twitter. Hey ho. They have 1574 follower and I have 7597. I wish them the best of luck.
Follow-up
Anesthesia & Analgesia is the official journal of the International Anesthesia Research Society. In 2012 its editor, Steven Shafer, proposed a head-to-head contest between those who believe that acupuncture works and those who don’t. I was asked to write the latter. It has now appeared in June 2013 edition of the journal [download pdf]. The pro-acupuncture article written by Wang, Harris, Lin and Gan appeared in the same issue [download pdf].
Acupuncture is an interesting case, because it seems to have achieved greater credibility than other forms of alternative medicine, despite its basis being just as bizarre as all the others. As a consequence, a lot more research has been done on acupuncture than on any other form of alternative medicine, and some of it has been of quite high quality. The outcome of all this research is that acupuncture has no effects that are big enough to be of noticeable benefit to patients, and it is, in all probablity, just a theatrical placebo.
After more than 3000 trials, there is no need for yet more. Acupuncture is dead.


Acupuncture is a theatrical placebo
David Colquhoun (UCL) and Steven Novella (Yale)
Anesthesia & Analgesia, June 2013 116:1360-1363.
Pain is a big problem. If you read about pain management centres you might think it had been solved. It hasn’t. And when no effective treatment exists for a medical problem, it leads to a tendency to clutch at straws. Research has shown that acupuncture is little more than such a straw.
Although it is commonly claimed that acupuncture has been around for thousands of years, it hasn’t always been popular even in China. For almost 1000 years it was in decline and in 1822 Emperor Dao Guang issued an imperial edict stating that acupuncture and moxibustion should be banned forever from the Imperial Medical Academy.
Acupuncture continued as a minor fringe activity in the 1950s. After the Chinese Civil War, the Chinese Communist Party ridiculed traditional Chinese medicine, including acupuncture, as superstitious. Chairman Mao Zedong later revived traditional Chinese Medicine as part of the Great Proletarian Cultural Revolution of 1966 (Atwood, 2009). The revival was a convenient response to the dearth of medically-trained people in post-war China, and a useful way to increase Chinese nationalism. It is said that Chairman Mao himself preferred Western medicine. His personal physician quotes him as saying “Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine” Li {Zhisui Li. Private Life Of Chairman Mao: Random House, 1996}.
The political, or perhaps commercial, bias seems to still exist. It has been reported by Vickers et al. (1998) (authors who are sympathetic to alternative medicine) that
“all trials [of acupuncture] originating in China, Japan, Hong Kong, and Taiwan were positive”(4).
Acupuncture was essentially defunct in the West until President Nixon visited China in 1972. Its revival in the West was largely a result of a single anecdote promulgated by journalist James Reston in the New York Times, after he’d had acupuncture in Beijing for post-operative pain in 1971. Despite his eminence as political journalist, Reston had no scientific background and evidently didn’t appreciate the post hoc ergo propter hoc fallacy, or the idea of regression to the mean.
After Reston’s article, acupuncture quickly became popular in the West. Stories circulated that patients in China had open heart surgery using only acupuncture (Atwood, 2009). The Medical Research Council (UK) sent a delegation, which included Alan Hodgkin, to China in 1972 to investigate these claims , about which they were skeptical. In 2006 the claims were repeated in 2006 in a BBC TV program, but Simon Singh (author of Fermat’s Last Theorem) discovered that the patient had been given a combination of three very powerful sedatives (midazolam, droperidol, fentanyl) and large volumes of local anaesthetic injected into the chest. The acupuncture needles were purely cosmetic.
Curiously, given that its alleged principles are as bizarre as those on any other sort of pre-scientific medicine, acupuncture seemed to gain somewhat more plausibility than other forms of alternative medicine. The good thing about that is that more research has been done on acupuncture than on just about any other fringe practice.
The outcome of this research, we propose, is that the benefits of acupuncture, if any, are too small and too transient to be of any clinical significance. It seems that acupuncture is little or no more than a theatrical placebo. The evidence for this conclusion will now be discussed.
Three things that are not relevant to the argument
There is no point in discussing surrogate outcomes such as fMRI studies or endorphine release studies until such time as it has been shown that patients get a useful degree of relief. It is now clear that they don’t.
There is also little point in invoking individual studies. Inconsistency is a prominent characteristic of acupuncture research: the heterogeneity of results poses a problem for meta-analysis. Consequently it is very easy to pick trials that show any outcome whatsoever. Therefore we shall consider only meta-analyses.
The argument that acupuncture is somehow more holistic, or more patient-centred, than medicine seems us to be a red herring. All good doctors are empathetic and patient-centred. The idea that empathy is restricted to those who practice unscientific medicine seems both condescending to doctors, and it verges on an admission that empathy is all that alternative treatments have to offer.
There is now unanimity that the benefits, if any, of acupuncture for analgesia, are too small to be helpful to patients.
Large multicenter clinical trails conducted in Germany {Linde et al., 2005; Melchart et, 2005; Haake et al, 2007, Witt et al, 2005), and in the United States {Cherkin et al, 2009) consistently revealed that verum (or true) acupuncture and sham acupuncture treatments are no different in decreasing pain levels across multiple chronic pain disorders: migraine, tension headache, low back pain, and osteoarthritis of the knee.
If, indeed, sham acupuncture is no different from real acupuncture the apparent improvement that may be seen after acupuncture is merely a placebo effect. Furthermore it shows meridians don’t exist, so the “theory” memorized by qualified acupuncturists is just myth. All that remains to be discussed is whether or not the placebo effect is big enough to be useful, and whether it is ethical to prescribe placebos.
Some recent meta-analyses have found that there may be a small difference between sham and real acupuncture. Madsen Gøtzsche & Hróbjartsson {2009) looked at thirteen trials with 3025 patients, in which acupuncture was used to treat a variety of painful conditions. There was a small difference between ‘real’ and sham acupuncture (it didn’t matter which sort of sham was used), and a somewhat bigger difference between the acupuncture group and the no-acupuncture group. The crucial result was that even this bigger difference corresponded to only a 10 point improvement on a 100 point pain scale. A consensus report (Dworkin, 2009) that a change of this sort should be described as a “minimal” change or “little change”. It isn’t big enough for the patient to notice much effect.
The acupuncture and no-acupuncture groups were, of course, not blind to the patients and neither were they blind to the practitioner giving the treatment. It isn’t possible to say whether the observed difference is a real physiological action or whether it’s a placebo effect of a rather dramatic intervention. Interesting though it would be to know this, it matters not a jot, because the effect just isn’t big enough to produce any tangible benefit.
Publication bias is likely to be an even greater problem for alternative medicine than it is for real medicine, so it is particularly interesting that the result just described has been confirmed by authors who practise, or sympathise with, acupuncture. Vickers et al. (2012) did a meta-analysis for 29 RCTs, with 17,922 patients. The patients were being treated for a variety of chronic pain conditions. The results were very similar to those of Madsen et al.{2009). Real acupuncture was better than sham, but by a tiny amount that lacked any clinical significance. Again there was a somewhat larger difference in the non-blind comparison of acupuncture and no-acupuncture, but again it was so small that patients would barely notice it.
Comparison of these two meta-analyses shows how important it is to read the results, not just the summaries. Although the outcomes were similar for both, the spin on the results in the abstracts (and consequently the tone of media reports) was very different.
An even more extreme example of spin occurred in the CACTUS trial of acupuncture for ” ‘frequent attenders’ with medically unexplained symptoms” (Paterson et al., 2011). In this case, the results showed very little difference even between acupuncture and no-acupuncture groups, despite the lack of blinding and lack of proper controls. But by ignoring the problems of multiple comparisons the authors were able to pick out a few results that were statistically significant, though trivial in size. But despite this unusually negative outcome, the result was trumpeted as a success for acupuncture. Not only the authors, but also their university’s PR department and even the Journal editor issued highly misleading statements. This gave rise to a flood of letters to the British Journal of General Practice and much criticism on the internet.
From the intellectual point of view it would be interesting to know if the small difference between real and sham acupuncture found in some, but not all, recent studies is a genuine effect of acupuncture or whether it is a result of the fact that the practitioners are never blinded, or of publication bias. But that knowledge is irrelevant for patients. All that matters for them is whether or not they get a useful degree of relief.
There is now unanimity between acupuncturists and non-acupuncturists that any benefits that may exist are too small to provide any noticeable benefit to patients. That being the case it’s hard to see why acupuncture is still used. Certainly such an accumulation of negative results would result in the withdrawal of any conventional treatment.
Specific conditions
Acupuncture should, ideally, be tested separately for effectiveness for each individual condition for which it has been proposed (like so many other forms of alternative medicine, that’s a very large number). Good quality trials haven’t been done for all of them. It’s unlikely that acupuncture works for rheumatoid arthritis, stopping smoking, irritable bowel syndrome or for losing weight. And there is no good reason to think it works for addictions, asthma, chronic pain, depression, insomnia, neck pain, shoulder pain or frozen shoulder, osteoarthritis of the knee, sciatica, stroke or tinnitus and many other conditions (Ernst et al., 2011).
In 2009, the UK’s National Institute for Clinical Excellence (NICE) did recommend both acupuncture and chiropractic for back pain. This exercise in clutching at straws caused something of a furore. In the light of NICE’s judgement the Oxford Centre for Evidence-based medicine updated its analysis of acupuncture for back pain. Their verdict was
“Clinical bottom line. Acupuncture is no better than a toothpick for treating back pain.”
The paper by Artus et al. (2010) is of particular interest for the problem of back pain. Their Fig 2 shows that there is a modest improvement in pain scores after treatment, but much the same effect, with the same time course is found regardless of what treatment is given, and even with no treatment at all. They say
“we found evidence that these responses seem to follow a common trend of early rapid improvement in symptoms that slows down and reaches a plateau 6 months after the start of treatment, although the size of response varied widely. We found a similar pattern of improvement in symptoms following any treatment, regardless of whether it was index, active comparator, usual care or placebo treatment”.
It seems that most of what’s being seen is regression to the mean. And that is very likely to be the main reason why acupuncture sometimes appears to work when it doesn’t.
Although the article by Wang et al (2012) was written to defend the continued use of acupuncture, the only condition for which they claim that there is any reasonably strong evidence is for post-operative nausea and vomiting (PONV). It would certainly be odd if a treatment that had been advocated for such a wide variety of conditions turned out to work only for PONV. Nevertheless, let’s look at the evidence.
The main papers that are cited to support the efficacy of acupuncture in alleviation of PONV are all from the same author: Lee & Done (1999), and two Cochrane reviews, Lee & Done (2004), updated in Lee & Fan (2009). We need only deal with this latest updated meta-analysis.
Although the authors conclude “P6 acupoint stimulation prevented PONV”, closer examination shows that this conclusion is very far from certain. Even taken at face value, a relative risk of 0.7 can’t be described as “prevention”. The trials that were included were not all tests of acupuncture but included several other more or less bizarre treatments (“acupuncture, electro-acupuncture, transcutaneous nerve stimulation, laser stimulation, capsicum plaster, an acu-stimulation device, and acupressure”). The number needed to treat varied from a disastrous 34 to a poor 5 for patients with control rates of PONV of 10% and 70% respectively.
The meta-analysis showed, on average, similar effectiveness for acupumcture and anti-emetic drugs. The problem is that the effectiveness of drugs is in doubt because an update to the Cochrane review has been delayed (Carlisle, 2012) by the discovery of major fraud by a Japanese anesthetist, Yoshitaka Fujii (Sumikawa, 2012). It has been suggested that metclopramide barely works at all (Bandolier, 2012; Henzi, 1999).
Of the 40 trials (4858 participants) that were included; only four trials reported adequate allocation concealment. Ninety percent of trials were open to bias from this source. Twelve trials did not report all outcomes. The opportunities for bias are obvious. The authors themselves describe all estimates as being of “Moderate quality” which is defined this: “Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate”. That being the case, perhaps the conclusion should have been “more research needed”. In fact almost all trials of alternative medicines seem to end up with the conclusion that more research is needed.
Conclusions
It is clear from meta-analyses that results of acupuncture trials are variable and inconsistent, even for single conditions. After thousands of trials of acupuncture, and hundreds of systematic reviews (Ernst et al., 2011), arguments continue unabated. In 2011, Pain carried an editorial which summed up the present situation well.
“Is there really any need for more studies? Ernst et al. (2011) point out that the positive studies conclude that acupuncture relieves pain in some conditions but not in other very similar conditions. What would you think if a new pain pill was shown to relieve musculoskeletal pain in the arms but not in the legs? The most parsimonious explanation is that the positive studies are false positives. In his seminal article on why most published research findings are false, Ioannidis (2005) points out that when a popular but ineffective treatment is studied, false positive results are common for multiple reasons, including bias and low prior probability.”
Since it has proved impossible to find consistent evidence after more than 3000 trials, it is time to give up. It seems very unlikely that the money that it would cost to do another 3000 trials would be well-spent.
A small excess of positive results after thousands of trials is most consistent with an inactive intervention. The small excess is predicted by poor study design and publication bias. Further, Simmons et al (2011) demonstrated that exploitation of “undisclosed flexibility in data collection and analysis” can produce statistically positive results even from a completely nonexistent effect. With acupuncture in particular there is documented profound bias among proponents (Vickers et al., 1998). Existing studies are also contaminated by variables other than acupuncture – such as the frequent inclusion of “electroacupuncture” which is essentially transdermal electrical nerve stimulation masquerading as acupuncture.
The best controlled studies show a clear pattern – with acupuncture the outcome does not depend on needle location or even needle insertion. Since these variables are what define “acupuncture” the only sensible conclusion is that acupuncture does not work. Everything else is the expected noise of clinical trials, and this noise seems particularly high with acupuncture research. The most parsimonious conclusion is that with acupuncture there is no signal, only noise.
The interests of medicine would be best-served if we emulated the Chinese Emperor Dao Guang and issued an edict stating that acupuncture and moxibustion should no longer be used in clinical practice.
No doubt acupuncture will continue to exist on the High Streets where they can be tolerated as a voluntary self-imposed tax on the gullible (as long as they don’t make unjustified claims).
|
REFERENCES
|
|
| 1. Acupuncture Centre. . About Acupuncture. Available at: http://www.acupuncturecentre.org/aboutacupuncture.html. Accessed March 30, 2013 | |
| 2. Atwood K. “Acupuncture Anesthesia”: a Proclamation from Chairman Mao (Part IV). Available at: http://www.sciencebasedmedicine.org/index.php/acupuncture-anesthesia-a-proclamation-from-chairman-mao-part-iv/. Accessed September 2, 2012 | |
| 3. Li Z Private Life of Chairman Mao: The Memoirs of Mao’s Personal Physician. 1996 New York: Random House | |
| 4. Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials. 1998;19:159–66 Available at: http://bit.ly/WqVGWN. Accessed September 2, 2012 | |
| 5. Reston J. Now, About My Operation in Peking; Now, Let Me Tell You About My Appendectomy in Peking … The New York Times. 1971 Available at: http://select.nytimes.com/gst/abstract.html?res=FB0D11FA395C1A7493C4AB178CD85F458785F9. Accessed March 30, 2013 | |
| 6. Atwood K. “Acupuncture anesthesia”: a proclamation from chairman Mao (part I). Available at: http://www.sciencebasedmedicine.org/index.php/acupuncture-anesthesia-a-proclamation-of-chairman-mao-part-i/. Accessed September 2, 2012 | |
| 7. Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes MG, Weidenhammer W, Willich SN, Melchart D. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293:2118–25 | |
| 8. Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes M, Hummelsberger J, Irnich D, Weidenhammer W, Willich SN, Linde K. Acupuncture in patients with tension-type headache: randomised controlled trial. BMJ. 2005;331:376–82 | |
| 9. Haake M, Müller HH, Schade-Brittinger C, Basler HD, Schäfer H, Maier C, Endres HG, Trampisch HJ, Molsberger A. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–8 | |
| 10. Witt C, Brinkhaus B, Jena S, Linde K, Streng A, Wagenpfeil S, Hummelsberger J, Walther HU, Melchart D, Willich SN. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366:136–43 | |
| 11. Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, Delaney K, Hawkes R, Hamilton L, Pressman A, Khalsa PS, Deyo RA. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169:858–66 | |
| 12. Madsen MV, Gøtzsche PC, Hróbjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ. 2009;338:a3115 | |
| 13. Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S, Burke LB, Cowan P, Farrar JT, Hertz S, Raja SN, Rappaport BA, Rauschkolb C, Sampaio C. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–44 | |
| 14. Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, Sherman KJ, Witt CM, Linde K. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–53 | |
| 15. Paterson C, Taylor RS, Griffiths P, Britten N, Rugg S, Bridges J, McCallum B, Kite G. Acupuncture for ‘frequent attenders’ with medically unexplained symptoms: a randomised controlled trial (CACTUS study). Br J Gen Pract. 2011;61:e295–e305 | |
| 16. . Letters in response to Acupuncture for ‘frequent attenders’ with medically unexplained symptoms. Br J Gen Pract. 2011;61 Available at: http://www.ingentaconnect.com/content/rcgp/bjgp/2011/00000061/00000589. Accessed March 30, 2013 | |
| 17. Colquhoun D. Acupuncturists show that acupuncture doesn’t work, but conclude the opposite: journal fails. 2011 Available at: https://www.dcscience.net/?p=4439. Accessed September 2, 2012 | |
| 18. Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011;152:755–64 | |
| 19. Colquhoun D. NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself. 2009 Available at: https://www.dcscience.net/?p=1516. Accessed September 2, 2012 | |
| 20. Colquhoun D. The NICE fiasco, part 3. Too many vested interests, not enough honesty. 2009 Available at: https://www.dcscience.net/?p=1593. Accessed September 2, 2012 | |
| 21. Bandolier. . Acupuncture for back pain—2009 update. Available at: http://www.medicine.ox.ac.uk/bandolier/booth/painpag/Chronrev/Other/acuback.html. Accessed March 30, 2013 | |
| 22. Artus M, van der Windt DA, Jordan KP, Hay EM. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology (Oxford). 2010;49:2346–56 | |
| 23. Wang S-M, Harris RE., Lin Y-C, Gan TJ. Acupuncture in 21st century anesthesia: is there a needle in the haystack? Anesth Analg. 2013;116:1356–9 | |
| 24. Lee A, Done ML. The use of nonpharmacologic techniques to prevent postoperative nausea and vomiting: a meta-analysis. Anesth Analg. 1999;88:1362–9 | |
| 25. Lee A, Done ML. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2004:CD003281 | |
| 26. Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2009:CD003281 | |
| 27. Carlisle JB. A meta-analysis of prevention of postoperative nausea and vomiting: randomised controlled trials by Fujii etal. compared with other authors. Anaesthesia. 2012;67:1076–90 | |
| 28. Sumikawa K. The results of investigation into Dr.Yoshitaka Fujii’s papers. Report of the Japanese Society of Anesthesiologists Special Investigation Committee. http://www.anesth.or.jp/english/pdf/news20120629.pdf | |
| 29. Bandolier. . Metoclopramide is ineffective in preventing postoperative nausea and vomiting. Available at: http://www.medicine.ox.ac.uk/bandolier/band71/b71-8.html. Accessed March 30, 2013 | |
| 30. Henzi I, Walder B, Tramèr MR. Metoclopramide in the prevention of postoperative nausea and vomiting: a quantitative systematic review of randomized, placebo-controlled studies. Br J Anaesth. 1999;83:761–71 | |
| 31. Hall H. Acupuncture’s claims punctured: not proven effective for pain, not harmless. Pain. 2011;152:711–2 | |
| 32. Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2:e124 | |
| 33. Simmons JP, Leif DN, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol Sci. 2011;22:1359–66 |
Follow-up
30 May 2013 Anesthesia & Analgesia has put the whole paper on line. No paywall now!
9 June 2013. Since this page was posted on May 30, it has had over 20,000 page views. Not bad.
26 July 2013. The Observer had a large double-page spread about acupuncture. It was written by David Derbyshire, largely on the basis of this article.
26 December 2013
Over christmas the flow of stuff that misrepresents the “thousands of years” of Chinese medicine has continued unabated. Of course one expects people who are selling Chinese herbs and acupuncture to lie. All businesses do. One does not expect such misrepresentation from British Columbia, Cardiff University School of medicine, or from Yale University. I left a comment on the Yale piece. Whether it passes moderation remains to be seen. Just in case, here it is.
One statement is undoubtedly baseless ““If it’s still in use after a thousand years there must be something right,” It’s pretty obvious to the most casual observer that many beliefs that have been round for a thousand years have proved to be utterly wrong.
In any case, it’s simply not true that most “Traditional” Chinese medicine has been around for thousands of years. Acupuncture was actually banned by the Emperor Dao Guang in 1822. The sort of Chinese medicine that is sold (very profitably) to the west was essentially dead in China until it was revived by Mao as part of the great proletarian cultural revolution (largely to stir up Chinese nationalism at that time). Of course he didn’t use it himself.
This history has been documented in detail now, and it surprises me to see it misrepresented, yet again, from a Yale academic.
Of course there might turn out to be therapeutically useful chemicals in Chinese herbs (it has happened with artemesinin). But it is totally irresponsible to pretend that great things are coming in the absence of good RCTs in human patients.
Yale should be ashamed of PR like this. And so should Cardiff University. It not only makes the universities look silly. It corrupts the whole of the rest of these institutions. Who knows how much more of their PR is mere puffery.
18 January 2014. I checked the Yale posting and found that the comment, above, had indeed been deleted. There is little point in having comments if you are going to delete anything that’s mildly critical. It is simply dishonest.
A recent post, A right royal cock-up, got a lot more press attention than I’d expected. Perhaps I should have realised that the mainstream media are fascinated with anything that involves royalty. Here is my last word on that topic.
My reasons for writing about it had very little to do with royalty. I was elected to the Royal Society in 1985 and I’ve tolerated the odd voting forms, and the election of Royal Fellows, in silence for the last 27 years. What made me speak out this time was almost entirely to do with Andrew’s record of dubious behaviour. For me, it was a moral question, not a question of royalty per se.
The election of Prince Andrew (as a "Royal Fellow", not on scientific grounds) attracted 171 votes and 1128 non-responders. I was curious to know why so many people failed to vote. I was also curious about the statement made to the Sunday Times
"David’s [Colquhoun] views about our royal connections are very much in a minority"
Since I don’t recall being asked, I’m baffled about what data (if any) on which that statement was based. There was only one way to find out. To ask. The following email was sent at around 5 pm on Friday 17 May.
|
Subject: A very quick question about the election of Royal Fellows In the light of the recent publicity surrounding the “election” of Prince Andrew as a Royal Fellow, I thought that, because so few people voted, it would be interesting to know the views of all fellows on this tradition. This mail is being sent to the 1197 fellows whose email address is given in the Year Book. All you need to do is to hit reply and put YES or NO next to the following two questions. Only the total numbers are interesting. I promise not to reveal how anyone voted. 1) Do you think that the time has come to discontinue the tradition of electing Royal Fellows? 2) Do you think the election of Prince Andrew, in particular, has harmed the reputation of the Royal Society? NB These questions do not refer to the monarch as patron (but if you have an opinion about that. please say so). Best regards David Colquhoun |
The intention was to word it as neutrally as possible. Few people expressed an opinion about the monarch as patron. I see no harm in continuing that tradition myself.
What happened?
First, the Year Book is out of date. 106 emails bounced, several were "out of office", and a few recipients had died. So about 1080 emails should have arrived. I have no way of knowing how many were opened and read.
After one week, 324 replies had arrived, almost twice as many as the 171 votes cast in the original ballot. A couple of responses were surprisingly abusive. More were supportive. Most made no comment. 70% of those mailed didn’t respond. The 30% return rate is certainly a flaw, tnough not as big a flaw as the 13% return rate in the orginal poll,
Perhaps 30% isn’t so surprising. A weekly newsletter goes out to all UCL staff, and it has interesting information, though a bit too PR-like for my taste. But I’m told that 50% of emails sent out are never even opened, never mind read.
The results were as follows.
Of 302 who answered question 1, 131 (43%) said YES
Of 284 who answered question 2, 151 (53%) said YES
It was noticeable that those who work outside the UK were distinctly more likely to say NO. Perhaps they are unaware of the extensive press coverage about Andrew in the UK? 54 answers were received from people with .edu addresses, 32% yes for question 1, and 38% yes on question 2. If these are excluded on the grounds that they are unlikely to be aware of the problems, the results are
Of 248 who answered question 1, 114 (46%) said YES
Of 239 who answered question 2, 134 (56%) said YES
It might also be relevant almost half the fellows are 70 years old or older and 80% of fellows are 60 or older. That’s not surprising because very few people are elected at younger than 40, many are much older, and once in, you are in for life.
What can we conclude?
(1) 70% of those mailed have little interest in the politics of the RS, and there is no way to know whether they even opened my mail,
(2) Roughly half of those who expressed an opinion agreed with me
so
(3) it is not true that "David’s [Colquhoun] views about our royal connections are very much in a minority".
It seems to me that these numbers provide a good case for the RS Council to consider whether or not it is a good idea to continue to nominate Royal Fellows.
One more thing
The Sunday Times was also told
"The Duke of York is beloved by the tabloids but he has always had a robust defence in these issues . . . I think David is quite wrong to raise that"
It is most certainly not true that Andrew’s reputation is bad only in tabloid newspapers.
Try this leader in the Times (March 2011) “Undiplomatic Envoy. Prince Andrew’s friendship with a convicted US financier is an embarrassment. He should resign as a trade envoy“. [pdf]There are many more reports like that in the Times.
The most royalist of Conservative broadsheets, the Daily Telegraph, broke the story of abuse of aircraft and published Timeline: the Duke of York’s questionable friends. And the Telegraph’s chief reporter wrote "Sack the Duke of York as trade envoy, says former ambassador". And in 2012, the Telegraph wrote "Money laundering probe puts spotlight on the £15 million sale of the Duke of York’s home"
In March 2011, Channel 4 News wrote “Prince Andrew: ‘Cheerleader in chief for the arms industry‘
The Guardian has been critical since 2004. And of course it was the Guardian who published the cables that revealed Andrew’s curious attitude to bribery in arms deals.
These are not tabloids. The fact that every newspaper has written this sort of thing is what caused me to worry that his election would not go down well with the public. One of the most alarming aspects of the affair was the comments left by readers on the various newspaper articles. They did not give the impression that the public was as impressed by the Royal Society as its fellows tend to be. That is bad for everyone because the society does much good work, in funding science (in particular the excellent University Research Fellowships which give young scientists five years of independence).
Postscript
I do sometimes wonder about the value of prizes and honours. My attitude to them is very much like that of one of my great scientific heroes, Richard Feynman. Watch this.
Follow-up
26 May 2013 The Sunday Times was onto the story quickly again, with a short piece. The cartoon isn’t totally appropriate (for me) since I’ve said repeatedly that it is Andrew’s morals that worry me, far more than his royalty.
























