alternative medicine
The Nutrition Society is the interim professional body for nutrition. It seems that, unlike so many ‘regulatory bodies’, it may actually take its responsibilities seriously. The following announcement has appeared on their web site.
|
The UK Voluntary Register of Nutritionists acts to protect the public and the reputation the nutrition profession On March 4th 2009, a Fitness to Practice Panel was convened to consider an allegation against a registrant, Dr Ann Walker, that her fitness to practise was impaired. The panel considered whether the registrant, in advocating the use of a web based personal nutritional profiling service had complied with the Code of Ethics’ clause 3: This expects all registered nutritionists to “maintain the highest standards of professionalism and scientific integrity”. In particular, the panel considered whether the registrant showed “knowledge, skills and performance of high quality, up-to-date, and relevant to their field of practice”, in keeping with the Statement of Professional Conduct (para 9). The Panel accepted the allegation of impaired fitness to practice. Mindful of its duty to protect the public, it recommended that Dr Walker be removed from the register. Dr Walker has a right of appeal. |
Well. well, this must be none other than the Dr Ann Walker who caused UCL,and me, such trouble a few years ago. And just because I described her use of the word “blood cleanser” as gobbledygook. She has appeared a few times on this blog.
- Nutribollocks: antioxidants useless, some are dangerous
- Red clover, herbal spin and vested interests
- The fallout from DC’s de-excommunication
- So what is a “blood cleanser”? Quinion speaks.
- Herbal medicines fail test
- Nutriprofile: useful aid or sales scam?
- She even gets a brief mention at Boots reaches new level of dishonesty with CoQ10 promotion

Presumably the “web-based personal nutritional profiling service” that is referred to is Nutriprofile, on which, with the help of a dietition, we had a bit of fun a while ago. However ideal your diet it still recommended at the end of the questionnaire that you should buy some expensive supplements. Read about it at Nutriprofile: useful aid or sales scam?
I have no idea who lodged the complaint (but it wasn’t me).
It is interesting to compare the high standards of the Nutrition Society with the quite different standards of BANT (the British Association for Applied Nutrition and Nutritional Therapy). They bill themselves as the “Professional Body for Nutritional Therapists”. Nutritional therapists are those fantasists who believe you can cure any ill by buying some supplement pills. Their standards can be judged by, for example, BANT ethics code: BANT nutritional therapists are allowed to earn commission from selling pills and tests.
It seems Dr Ann Walker may have joined the wrong society.
Follow-up

On 24 July 2006, I sent a request to the University of Central Lancashire (UCLAN), under the Freedom of Information Act (2000) I asked to see the teaching materials that were used on their BSc Homeopathy course. The request was refused, citing the exemption under section 43(2) of the Act (Commercial Interests).
Two internal reviews were then held. These reviews upheld and the original refusal on the grounds of commercial interests, Section 43(3), and additionally claimed exemption under Section 21 “that is reasonably accessible to applicants by other means (upon the payment of a fee)….i.e. by enrolling on the course….”
In 21 October 2006 I appealed to the Office of the Information commisioner. (The”public authority” means UCLAN, and “the complainant” is me.)
|
“The complainant specifically asked the Commissioner to consider the application of section 43(2) to the course materials he had requested. The main thrust of his argument in this regard was that the public authority could not be considered a ‘commercial organisation’ for the purposes of the Act, and that the public authority had confused ‘commercial interests’ with ‘financial interests’. He however added that if the Commissioner decided section 43(2) was correctly engaged, then it was in the public interest to order disclosure.” |
In May 2008, my appeal got to the top of the pile, and on 30th March 2009 a judgement was delivered. In all respects but one trivial one, the appeal was upheld. In future universities will not be able to refuse requests for teaching materials.
The Decision Notice is on the web site of the Office of the Information Commissioner, [or download pdf file].
This whole thing has taken so long that the course at which it was aimed has already closed its doors last August (and blamed that, in part, on the problems caused by the Freedom of Information Act). UCLAN also announced a review of all its alternative medicine activities (and asked me to give evidence to it). That review is due to report its findings any time now.
Tha particular course that prompted the request is no longer the point. What matters is that all the usual exemptions claimed by universities have been ruled invalid. Here are a few details
What the decision notice says (the short version)
The full text of the Act is here.
The following three exemptions were judged NOT to apply the requests for university teaching materials. I’ll quote some bits from the Decision Notice.
Section 21 provides that –
“Information which is reasonably accessible to the applicant otherwise than under section 1 is exempt information.”
|
34. The public authority’s argument suggests that the requested information is reasonably accessible to the complainant if he enrols as a student on the course, and is therefore not accessible to him by any other means outside the Act unless he decides to make a total payment of £9,345 as a combined payment of three years tuition fees. 40. The Commissioner therefore finds that the public authority incorrectly applied the exemption contained at section 21 of the Act. |
Section 42(2) provides that –
“Information is exempt information if its disclosure under this Act would, or would be likely to, prejudice the commercial interests of any person (including the public authority holding it).”
|
71. The Commissioner therefore finds that the section 43(2) was incorrectly engaged by virtue of the fact that the public authority’s ability to recruit students is not a commercial interest within the contemplation of section 43(2). 76. In addition to his finding on commercial interests the Commissioner finds that section 43(2) would in any case not be engaged as the likelihood of prejudice to the public authority’s ability to recruit students as a result of disclosure under the Act is no more than the likelihood of prejudice resulting from the availability of the course materials to students already enrolled on the course. |
Section 36(2)C provides that –
“Information to which this section applies is exempt information if, in the reasonable opinion of a qualified person, disclosure of the information under this Act-
(c) would otherwise prejudice, or would be likely otherwise to prejudice, the effective conduct of public affairs
| 98. For the reasons set out above, the Commissioner finds that section 36(2)(c) is not engaged as he does not accept the opinion of the qualified person is an objectively reasonable one. He does not find that disclosure would be likely to prejudice the effective conduct of public affairs. |
Section 41(1) provides that –
“Information is exempt information if-
(a) it was obtained by the public authority from any other person (including another public authority), and
(b) the disclosure of the information to the public (otherwise than under this Act) by the public authority holding it would constitute a breach of confidence actionable by that or any other person.”
| 56. The Commissioner therefore finds the public authority correctly applied the exemption contained at section 41 to the case studies listed in Annex A. In the Commissioner’s view, even though the patients would not be identifiable if the case studies were disclosed, this disclosure would still be actionable by the patients. |
The Decision
|
99. The Commissioner finds that section 41 is engaged 100. He however finds that the exemptions at sections 21, 43(2), and 36(2)(c) are not engaged. 101. The Commissioner therefore finds the public authority in breach of; • Sections 1(1)(b) and 10(1), because it failed to disclose the remainder of the course materials (i.e. excluding the case studies) to the complainant within 20 working days. • Section 17(1), because it did not specify in its refusal notice that it was also relying on sections 41 and 36(2)(c). |
Steps required
|
103. The Commissioner requires the public authority to take the following steps to ensure compliance with the Act: • Disclose all the course materials for the BSc (Hons) in Homeopathy apart from the case studies listed in Annex A of this Notice. 104. The public authority must take the steps required by this notice within 35 calendar days of the date of this notice. |
Follow-up
In March 2007 I wrote a piece in Nature on Science degrees without the science. At that time there were five “BSc” degrees in homeopathy. A couple of weeks ago I checked the UCAS site for start in 2009, and found there was only one full “BSc (hons)” left and that was at Westminster University.
Today I checked again and NOW THERE ARE NONE.
A phone call to the University of Westminster tonight confirmed that they have suspended entry to their BSc (Hons) homeopathy degree.
They say that they have done so because of “poor recruitment”. It was a purely financial decision. Nothing to do with embarrasment. Gratifying though it is that recruits for the course are vanishing, that statement is actually pretty appalling It says that the University of Westminster doesn’t care whether it’s nonsense, but only about whether it makes money.
Nevertheless the first part of this post is not entirely outdated before it even appeared, because homeopathy will still be taught as part of Complementary Therapies. And Naturopathy and “Nutritional Therapy” are still there..
According to their ‘School of Integrated Health‘, “The University of Westminster has a vision of health care for the 21st Century”. Yes, but it is what most people would call a vision of health care in the 18th century.
The revelation that the University of Westminster teaches that Amethysts emit high Yin energy caused something of a scandal.
Since then I have acquired from several sources quite a lot more of their teaching material, despite the fact that the university has refused to comply with the Freedom of Information Act.
In view of the rather silly internal review conducted by Westminster’s Vice-Chancellor, Professor Geoffrey Petts, this seems like a good moment to make a bit more of it public,
I think that revelation of the material is justified because it is in the
public interest to know how the University if Westminster is spending taxpayers’ money. Another motive is to defend the reputation of the post-1992 universities. I have every sympathy with the ex-polytechnics in their efforts to convert themselves into universities. In many ways they have succeeded. That effort
is impeded by teaching mystical versions of medicine.
If the University of Westminster is being brought into disrepute, blame its vice-chancellor, not me.
Homeopathic spiders
Here are a few slides from a lecture on how good spider venom is for you. It is from Course 3CTH502 Homeopathic Materia Medica II. No need to worry though, because they are talking about homeopathic spider venom, so there is nothing but sugar in the pills. The involvement of spiders is pure imagination. No more than mystical gobbledygook.


You are in hurry, or play with your fingers? You need spider venom pills (that contain no spider venom).




You break furniture? Time goes too fast for you? Try the tarantula-free tarantula pills.


You are preoccupied with sex? You play with ropes? What you need is Mygale (which contains no Mygale)


Much more seriously, the same sugar pills are recommended for serious conditions, chorea, ‘dim sight’, gonorrhoea, syphilis and burning hot urine.

This isn’t just preposterous made-up stuff. It is dangerous.
There is a whole lot more fantasy stuff in the handouts for Homeopathy Materia Medica II (3CTH502). Here are a couple of examples.
Aurum metallicum (metallic gold) [Download the whole handout]
Affinities MIND, VASCULAR SYSTEM, Nerves, Heart, Bones, Glands, Liver, Kidneys, RIGHT SIDE, Left side.
Causations Emotions. Ailments from disappointed love and grief, offence or unusual responsibility, abuse of mercury or allopathic drugs.
Aurum belongs to the syphilitic miasm but has elements of sycosis (Aur-Mur).
Potassium salts are the subject of some fine fantasy, in “The Kali’s” [sic]. (there is much more serious stuff to worry about here than a few misplaced apostrophes.). [Download the whole handout]
“The radioactive element of potassium emits negative electrons from the atom nucleus and is thought to be significant in the sphere of cell processes especially in relation to functions relating to automatism and rhythmicity.”
“Kali people are very conscientious with strong principles. They have their rules and they stick to them, ‘a man of his word’.”
“Potassium acts in a parasympathetic way, tending towards depression”
“They [“Kali people=] are not melancholic like the Natrum’s but rather optimistic.”
Radioactive potassium is involved in automaticity? Total nonsense.
Where is the science?
Yes, it is true that the students get a bit of real science. There isn’t the slightest trace that I can find of any attempt to resolve the obvious fact that what they are taught in the science bits contradict directly what they are told in the other bits. Sounds like a recipe for stress to me.
They even get a bit of incredibly elementary statistics. But they can’t even get that right. This slide is from PPP – Res Quant data analysis.

“Involves parameters and/or distributions”. This has no useful meaning whatsoever, that I can detect.
“Tests hypotheses when population distributions are skewed”. Well yes, though nothing there about forms of non-Gaussian properties other than skew, nothing about normalising transformations, and nothing about the Central Limit theorem.
“Ranks data rather than the actual data itself”. This is plain wrong. Randomisation tests on the original data are generally the best (uniformly most powerful) sort of non-parametric test. It seems to have escaped the attention of the tutor that ranking is a short-cut approximation that allowed tables to be constructed, before we had computers.
The students are told about randomised controlled trials. But amazingly in the lecture PPP-RCTs, the little matter of blinding is barely mantioned. And the teacher’s ideas about randomisation are a bit odd too.

Sorry, but if you fiddle the randomisation, no amount of “careful scrutiny” will rescue you from bias.
An Introduction to Naturopathic Philosophy
Naturopathy is just about as barmy as homeopathy. You can see something about it at the University of Wales. How about this slide from Westminster’s An Introduction to Naturopathic Philosophy.

So if you get tuberculosis, it isn’t caused by Mycobacterium tuberculosis? And the symptoms are “constructive”? So you don;t need to do anything. It’s all for the best really.
This isn’t just nonsense. It’s dangerous nonsense.
Traditional Chinese Medicine
Ever wondered what the mysterious “Qi” is? Worry no more. All is explained on this slide.

It means breath, air, vapour, gas, energy, vitalism. Or perhaps prana? Is that quite clear now?

What can we make of this one? Anyone can see that the description is barely written in English and that vital information is missing (such as the age of the woman). And it’s nonsense to suggest that “invasion of cold” (during keyhole surgery!) would cause prolonged constriction of blood vessels (never mind that it would “consume yang qi”). Not being a clinician, I showed it to an oncologist friend. He said that it was impossible to tell from the description whether the problem was serious or not, but that any abdominal pain should be investigated properly. There isn’t anything here about referral for proper investigation. Just a lot of stuff about ginger and cinnamon. Anyone who was taught in this way could be a real danger to the public. It isn’t harmless nonsense It’s potentially harmful nonsense.
And finally, it’s DETOX
Surely everyone knows by now that ‘detox’ is no more than a marketing word? Well not at the University of Westminster. They have a long handout that tells you all the usual myths and a few new ones.
It is written by Jennifer Harper-Deacon, who describes herself modestly, thus.
Jennifer Harper-Deacon is a qualified and registered Naturopath and acupuncturist who holds a PhD in Natural Health and MSc in Complementary Therapies. She is a gifted healer and Reiki Master who runs her own clinic in Surrey where she believes in treating the ‘whole’ person by using a combination of Chinese medicine and naturopathic techniques that she has qualified in, including nutritional medicine, Chinese and Western herbalism, homoeopathy, applied kinesiology, reflexology, therapeutic massage, aromatherapy and flower remedies.
It seems that there is no limit on the number of (mutually incompatible) forms of nuttiness that she believes. Here are a few quotations from her handout for Westminster students.
“Detoxification is the single most powerful tool used by natural health professionals to prevent and reverse disease”
What? To “prevent and reverse” malaria? tuberculosis? Parkinson’s disease? AIDS? cancer?
“When you go on to a raw food only diet, especially fruit, the stored toxins are brought up from the deep organs such as the liver and kidneys, to the superficial systems of elimination.”;
Very odd. I always though that kidneys were a system of elimination.
“The over-use and mis-use of antibiotics has weakened the body’s ability to attack and destroy new strains of resistant bacteria, virulent viruses, which have led to our immune system becoming compromised.”
Certainly over-use and mis-use are problems. But I always thought it was the bacteria that became resistant.
“The beauty about detoxification therapy is that it addresses the very causative issues of health problems”
That is another dangerous and silly myth. Tuberculosis is not caused by mythical and un-named “toxins”. It is caused by Mycobacterium tuberculosis.
“Naturopathy follows the logic of cause and effect therefore believes that we simply need pure food and water, sunshine, air, adequate rest and sleep coupled with the right amount of exercise for health.”
Try telling that to someone with AIDS.
“Colon cleansing is one of the most important parts of any detoxification programme.”
The strange obsession with enemas in the alternative world is always baffling.
“Frankincense: holds the capacity to physically strengthen our defence system and can rebuild energy levels when our immune system is weak. Revered as a herb of protection, frankincense can also strengthen our spiritual defences when our Wei qi is low, making us more susceptible to negative energies. This calming oil has the ability to deepen the breath, helping us to let go of stale air and emotions, making it ideal oil to use inhale prior to meditating.”
This is so much hot air. There is a bit of evidence that frankincense might have some anti-inflammatory action and that’s it.
But this has to be my favourite.
“Remember when shopping to favour fruits and vegetables which are in season and locally grown (and ideally organic) as they are more vibrationally compatible with the body.”
Locally grown vegetables are “more vibrationally compatible with the body”? Pure mystical gobbledygook. Words fail me.
OK there’s a whole lot more, but that will do for now.
It’s good that Westminster is shutting down its Homeopathy BSc, but it seems they have a bit further to go.
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
It is almost six months now since I posted Quackery creeps into good universities too -but through Human Resources. One example given there was the University of Leicester. This is an excellent university. It does first class research and it was the alma mater of the incomparable David Attenborough who has done more than anyone to show us the true beauty and wonder of the natural world.
Nevertheless, their well-meaning occupational health department had a section about “complementary therapies” that contained a lot of statements that were demonstrably untrue. They even recommended the utterly outrageous SCENAR device. So I pointed this out to them, and I had a quick and sympathetic response from their HR director.
But three months later, nothing had changed. Every now and then, I’d send a polite reminder, but it seemed the occupational health staff were very wedded to their quackery. The last reminder went on 6th February, but this time I copied it to Leicester’s vice-chancellor. This time it worked. There is still a link to Complementary Therapies on the Wellbeing site, but if you click on it, this is what you see.
Complementary therapiesSome employees may have an interest in complementary therapies such as acupuncture, yoga, Indian head massage, Reiki, sports & remedial massage, reflexology and hypnotherapy. If you have an interest in any of these, Staff Counselling can happily provide details of practitioners in the local area. Some of these practitioners offer discounts from their normal rates for University of Leicester staff. However, the University of Leicester cannot vouch for, or recommend any of these therapies to staff as being effective. We would urge members of staff who believe that such therapies might be effective to contact their GP prior to undertaking any of them. Further, the University of Leicester shall not be liable for any damage of any kind arising out of or related to the services of any complementary therapists or treatments listed here. If you would like further information, please contact Chris Wilson at: staffcounsel&welfare@le.ac.uk or telephone 1702. |
That’s not bad. Pity it doesn’t say alternative, rather than complementary though. Euphemisms aren’t really helpful.
In fact I have a bit of a problem with “wellbeing” too. It is a harmless word that has been highjacked so that its use now makes one think of mud baths provided by expensive hotels for their rich and gullible customers.
Leicester’s HR director wrote
“Unfortunately an instruction I had given previously had not been fully complied with. I spoke to the manager of the Staff Counselling team on Friday and gave clear instructions as to the content of this site. I had been assured that the offending information had been removed, but found that it had not.
I have now checked the site for myself and can say, with confidence, that all claims for the efficacy of complimentary [sic] therapies have been removed including SCENAR.”
The similarity between quack treatments and religion is intriguing. It seems that the devotion of the occupational health people to their baloney was so great that they wouldn’t take it down even when told to do so. The more irrational the belief, the greater the fervour with which it is defended,
What’s the lesson from this minor saga? It seems that most VCs and many HR people are too sensible to believe in alternative baloney, but that they are a bit too ready to tolerate it, perhaps on grounds of political correctness. Tolerance is a virtue, but lies about health are not in the least virtuous. If you point out that people are saying things for which there isn’t the slightest evidence, they will often respond. Just be prepared to send a few reminders.
It may also be useful to point out that some of the claims made are almost certainly illegal. Even people who care little about evidence of efficacy are impressed by the idea that they might be prosecuted by Trading Standards officers.
Who needs mystical medicine when you have real wonders like these.
(Click the google video logo for a bigger version)
Or try the pitcher plant video, or the Bird of paradise, or the Bower Bird, or the giant Amazon lilies.
Follow-up
This letter appeared in the Times on Friday 30 January, 2009. It was prompted by the news from the University of Salford, but its main purpose was to try to point out to the Department of Health that you can’t hope to regulate alternative treatments in any sensible way while continuing to push under the carpet the crucial question of which ones work and which don’t.
| Sir
We would like to congratulate the vice-chancellor of the University of Salford, Professor Michael Harloe for his principled decision to drop “all the University’s programmes associated with complementary medicine within the School of Community, Health Sciences & Social Care”. This includes their “Homeopathy in Practice” degree. It is also encouraging that the University of Central Lancashire recently closed its BSc in Homeopathy to new students, and announced a review of all its activities in alternative medicine. Although universities are now taking sensible actions, government policy in the area of regulation of alternative medicine is in urgent need of revision. In May 2008 the Steering Group chaired by Professor Pittilo recommended to the Department of Health that entry into acupuncture, herbal medicine and traditional Chinese medicine should “normally be through a bachelor degree with honours”. But, in the same month, new regulations on Unfair Trading came into effect. One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. One part of government seeks to endorse unproven and disproved treatments, at the same time as another part makes them illegal. The reason for this chaotic situation is simple. The Department of Health, and the Medicines and Healthcare products Regulatory Agency (MHRA), have consistently failed to grasp the nettle of deciding which treatments work and which don’t. That is the first thing you want to know about any treatment. Vice-chancellors seem now to be asking the question, and the government should do so too. The ideal mechanism already exists. The question should be referred to the National Institute for Health and Clinical Excellence (NICE). That was recommended by a House of Lords report in 2000, and it was recommended again by the Smallwood report (commissioned by the Prince of Wales) in 2005. Now it should be done. Sir Walter Bodmer FRCPath, FRS, FMedSci, FRCP (hon) FRCS(hon) Professor David Colquhoun, FRS Dame Bridget Ogilvie , AC, DBE, FRS, FAA, Professor Dame Nancy Rothwell, FRS, FMedSci, FRCP (hon) |
(Actually, the Times removed the qualifications of the signatories, but left the titles!)
An earlier, longer, version of the letter tried to preempt the obvious criticism by including, as the second paragraph, this passage.
“It makes no sense to offer Bachelor of Science degrees in subjects that have no scientific basis. Not only is homeopathy scientifically absurd, but also the best quality clinical trials show that it is not distinguishable from placebo. From the point of view of the patient, there is nothing wrong with placebo effects. Conventional drugs benefit from them too. There is everything wrong with surrounding the placebo effect with mystical mumbo-jumbo and awarding degrees in it.”
Universities drop degree courses in alternative medicine
In the same issue, there was a related article by the Times’ education editor, Alexandra Frean: Universities drop degree courses in alternative medicine..
“Universities are increasingly turning their backs on homoeopathy and complementary medicine amid opposition from the scientific community to “pseudo-science” degrees.
The University of Salford has stopped offering undergraduate degrees in the subjects, and the University of Westminster announced yesterday that it plans to strengthen the “science base” content of its courses after an internal review which examined their scientific credibility.
Both universities are following the lead of the University of Central Lancashire, which last year stopped recruiting new students to its undergraduate degree in homoeopathic medicine.
The decisions by Salford and Westminster open a new chapter in the fierce debate about the place of awarding of Bachelor of Science degrees in subjects that are not science.”
The article ends thus.
“Other universities are more robust in their defence of their courses
Ian Appleyard, principal lecturer in acupuncture at London South Bank University, said that acupuncture should be studied for the very reason that it was not well understood from the standpoint of Western scientific medicine. Acupuncture had been used by a significant proportion of the world’s population for thousands of years.
“Recent large-scale clinical trials such Haake and meta-analysis from reputable institutions such as The Cochrane Collaboration, have shown that there is evidence to support the therapeutic benefits of acupuncture treatment for back pain and migraine,” he said.”
Uhuh, it seems that Ian Appleyard has been reading the misleading BBC report on the recent trials. In fact they show precisely the opposite of what he claims. The fact that advocates of alternative medicine can misinterpret the evidence so badly is, I guess, at the heart of the problem.
What’s happening at the University of Westminster?
Westminster has regularly been labelled as the University that has more quackery courses than any other.
It is also the only university for which we have much idea about what is taught. The university, like all others, has tried to keep secret what they teach. That itself shows that they aren’t very proud of it. But a surprising amount has leaked out from Westminster, nonetheless. The set of “vibrational medicine” slides, including “Amethysts emit high Yin energy”, have caused much hilarity. The Westminster “miasmatic” examination question gets some laughs too, after it was published in Nature. The set of homeopathic materia medica notes that have come into my possession are pretty good too (coming on line soon).
Recently it emerged that the University of Westminster had followed the example of the University of Central Lancashire (UCLAN), and set up a review of its activities in alternative medicine. But unlike UCLAN it was kept secret, and as far as one can tell, it asked for no input from critics.
Well the outcome of this review turned up in my mail recently. Click the picture to read the whole letter from the Vice-Chancellor.
There is no doubt that the outcome, so far, is rather disappointing. Here are some quotations from this letter, with my comments interleaved.
“The Audit was Chaired by Professor Alan Jago and carried out its review using a comprehensive evidence base”
Alan Jago is a pro- vice chancellor, and formerly from Westminster’s School of Architecture and the Built Environment, so no specialist knowledge there.
“The panel made a number of recommendations to me as a result of their Audit. Many of these recommendations concern the University’s processes for review and validation of courses and these will be passed to the Pro Vice Chancellor responsible for Quality to consider.”
Uhuh, sounds like box-ticking again When will universities learn that validation procedures are, on the whole, not worth the paper they are written on.
“The overarching aim of these actions then is to strengthen and make more explicit the ‘scientific’ nature of the Integrated Health undergraduate degrees.
In order to do this we will:
Strengthen learning outcomes particularly in discipline and clinical modules to reflect the science outcomes embedded in the courses.
Revise course specific regulations to explicitly identify that the core health sciences modules have to be passed to complete a degree of the BSc Scheme.
Strengthen the final year project offer to provide more scientific projects through working with Biosciences staff.
Strengthen the scientific/academic qualifications of staff through development
of existing staff and appointments where they become available.”
This seems to me to be whistling in the wind. Remember, we are talking about “bachelor of science” degrees in things like homeopathy and naturotherapy. These are things that are not science at all. In fact they are antiscience to their core.
If you were successful in raising the increasing the scientific level of the staff, many of the subjects they are meant to be teaching would vanish in a puff of smoke.
Certainly the responses of the Westminster staff to earlier enquiries (here, and here) showed little sign of scientific thinking.
And I wonder what Westminster’s admirable biomedical scientists think about taking on homeopathy students for projects?
“I am certain that this work will place Complementary therapies courses in an extremely strong position to meet the external challenges of the future.
I’m sorry to say, Professor Petts, that the scientific community is not likely to share your certainty.
Remember, Peter Fisher is on record as saying that there is not enough science in homeopathy to justifiy offering a BSc degree in it (watch the movie). He is the Queen’s Homeopathic Physician, and Clinical Director of the Royal London Homeopathic Hospital But Westminster still seems to know better.
It seems, so far, that Westminster has missed a chance to change for the better.
Follow-up
Times Higher Education published a pretty pathetic report on the Westminster audit. They did ask me for comments but then failed to publish most of them. I suppose a magazine like that is so dependent on advertising that they can’t afford to upset the authorities. Nevertheless, do they really have to be quite so bland?
I hear that the internal audit has made everyone at the University of Woominster Westminster more nervous and that staff and students have been advised not to share teaching material with people outside the university. Having seen some of them, I’m not surprised they are ashamed of them.
Acupuncture in the BMJ
A new review appeared in the BMJ today. It is by Madsen et al., from the Nordic Cochrane Centre, Copenhagen. Here are the conclusions.
- The analgesic effect of acupuncture is small and cannot be distinguished from bias resulting from incomplete blinding.
- The analgesic effect of placebo acupuncture is moderate but very variable as some large trials report substantial effects.
- The effect of acupuncture seems to be unrelated to the type of placebo acupuncture used as control.
The results confirm, yet again, that there is essentially no difference between “real” acupuncture and sham acupuncture. All that talk about meridians and Qi really is so much mumbo jumbo.

The average effect (the diamond at the bottom) is essentially zero.
It has often been supposed that acupuncture is a theatrical placebo, but because of the placebo effect it produces more pain relief than (non-blind) controls. This study confirms that there is likely to be such an effect, but it also finds that the size of the placebo effect is too small to be useful to patients. Here is the comparison between sham acupuncture and no acupuncture at all.

The results of different trials are very variable, but the average effect (diamond at the bottom) favours sham acupuncture over no acupuncture at all.
But how big is the effect? The numbers along the bottom of the graph are ‘standardised mean differences’. The average value of -0.42 (95% confidence limits -0.6 to -0.23) between ‘no acupuncture’ and ‘sham acupuncture’ corresponds to a difference of about 10 points on a 100 point scale. This difference is big enough to be real, in the sense that it isn’t just chance. But is it big enough to be useful to the patient? Probably not. Madsen et al conclude
“a consensus report characterised a 10mm reduction on a 100 mm visual analogue scale as representing a “minimal” change or “little change”. Thus, the apparent analgesic effect of acupuncture seems to be below a clinically relevant pain improvement.”
This makes nonsense of the Pittilo report. Notice that these results, yet again, make nonsense of the proposals in the gamma-minus Pittilo report, to pseudo-regulate acupuncture, and to have degrees in the subject.
Cochrane reviews of Acupuncture : and a bad report from BBC
Two new Cochrane reviews appeared last week, Acupuncture for tension-type headache, and Acupuncture for migraine prophylaxis.
You can’t blame subeditors for the appalling title of the BBC’s report on Acupuncture ‘works for headaches’. The content is pretty misleading too. (The link is to a version saved at 19.35 on 21 January 2009.). Furthermore, like far too many of the BBC reports, it is anonymous. One has no idea to blame This is important, if only because the BBC news site is so influential. Twelve hours after posting the misleading title has been copied all round the world.
In the Guardian, Ian Sample had a much better report, Even’fake’ acupuncture reduces the severity of headaches and migraines. Sadly the print edition had the title “Acupuncture aids migraines, researchers
find”, but that can be blamed on subeditors who have a problem with reading (in fact Sample had seen neither title).
The BBC report seemed to call for a complaint. This is what I sent.
| I wish to complain about the report on acupuncture at http://news.bbc.co.uk/1/hi/health/7838231.stm
The title itself was highly misleading “Acupuncture works for headaches” is precisely the opposite of what was shown, namely that it is no better than sham acupuncture controls. The article goes on to say
It is not said that there isn’t the slightest reason to think this is true (or even means anything) , and that the work which is being reported is strong evidence that it’s not true
That is wrong. University of Salford , for example has just closed its acupuncture course after a number of us have pointed out that it is teaching things that aren’t true
It is exactly the opposite of an endorsement. It is one more nail in the coffin of acupuncture as generally understood. This article, I contend, is partial and misleading. Unfortunately it is anonymous. |
Follow-up
Today’s BBC report on the BMJ paper is almost as partisan as the one that I just complained about. “Confusion on acupuncture benefit ” exaggerates greatly the amount of confusion. Worse still, it quotes only two well-known advocates of acupuncture, people who make their living from it. No independent scientific voice is to be heard.
One of those cited is Adrian White. He is described as “a researcher into acupuncture at the Peninsula Medical School”. There is no mention of the fact that he is also Editor in Chief of the journal Acupuncture in Medicine. The other person who is quoted is Mike O’Farrell, the chief executive of the British Acupuncture Council. What do you expect him to say?
I’ve just sent another complaint, about today’s BBC report. The more the merrier.
The BMJ itself published an editorial on the Madsen paper. It seems very odd that they should have chosen the editors of the BMJ-group journal, Acupuncture in Medicine, to comment on a paper that sounds the death knell for the subject from which they make their living. Needless to say, the editorial attempted to wriggle out of the obvious conclusions. Worse still, the Health editor of the BBC web site referred to the editorial in his defence, in response to my complaint.
Channel 4 News does a lot better than the BBC, or the BMJ editorial, with its report Acupuncture ‘fails to relieve pain’
“Claims that acupuncture can relieve pain have been undermined by the results of a new study.”
“senior researcher Asbjorn Hrobjartsson said: “Our findings question both the traditional foundation of acupuncture…and the prevailing theory that acupuncture has an important effect on pain in general”. “
The Daily Telegraph also, like almost everyone else, did better than the BBC, with “Acupuncture ‘has almost no effect in relieving pain’”
“The pain relieving effects of acupuncture are so small that they may be clinically irrelevant, according to a review of research into the treatment.”
Even Metro, the free London Newspaper, is more accurate then the BBC. They carry a short report “Acupuncture ‘has no medical point’.”
“The pain-relieving effects of acupuncture compared with a placebo are so small they may be clinically irrelevant.”
New review puts in doubt traditional foundation of acupuncture. Believe it or not, that is the title of the report on Madsen et al from the Prince’s Foundation for Integretad Health! Don’t get too excited though. They haven’t even bothered to look at the original paper, but merely cite the dreadful BBC report. Much prominence is given to the acupuncturists, White and O’Farrell, and the important finding isn’t mentioned at all. Another gamma minus.
It’s only a matter of weeks since a lot of young scientists produced a rather fine pamphlet pointing out that the “detox” industry is simply fraud. They concluded
“There is little or no proof that these products work, except to part people from their cash.”
With impeccable timing, Duchy Originals has just launched a “detox” product.
Duchy Originals is a company that was launched in 1990 by the Prince of Wales, Up to now, it has limited itself to selling overpriced and not particularly healthy stuff like Chocolate Butterscotch Biscuits and Sandringham Strawberry Preserve. Pretty yummy if you can afford them.
The move of HRH into herbal concoctions was first noted in the blogosphere (as usual) in December, by Quackometer. It was reported recently in the Daily Telegraph (23rd January).
Expect a media storm.

Aha so it is a “food supplement” not a drug. Perhaps Duchy Originals have not noticed that there are now rather strict regulations about making health claims for foods?
And guess who’s selling it? Yes our old friend, for which no deception is too gross, Boots the Chemists.
That’s £10 for 50 ml. Or £200 per litre.
And what’s in it?

Problem 1. The word detox has no agreed meaning. It is a marketing word, designed to separate the gullible from their money
Problem 2. There isn’t the slightest reason to think that either artichoke or dandelion will help with anything at all. Neither appears at all in the Cochrane reviews. So let’s check two sources that are both compiled by CAM sympathisers (just so I can’t be accused of prejudice).
National Electronic Library of CAM (NELCAM) reveals nothing useful.
- There is no good evidence that artichoke leaf extract works for lowering cholesterol. No other indications are mentioned.
- Dandelion doesn’t get any mention at all.
The US National Center for Complementary and Alternative Medicine (NCCAM) has spent almost $1 billion on testing alternative treatments So far they have produced no good new remedies (see also Integrative baloney @ Yale).They publish a database of knowledge about herbs. This is what they say.
- Dandelion. There is no compelling scientific evidence for using dandelion as a treatment for any medical condition.
- Artichoke isn’t even mentioned anywhere.
If “detox” is meant to be a euphemism for hangover cure, then look at the review by Pittler et al (2005), ‘Interventions for preventing or treating alcohol hangover: systematic review of randomised controlled trials’.
“Conclusion No compelling evidence exists to suggest that any conventional or complementary intervention is effective for preventing or treating alcohol hangover. The most effective way to avoid the symptoms of alcohol induced hangover is to practise abstinence or moderation.”
Problem 3. The claim that the product is “cleansing and purifying” is either meaningless or false. Insofar as it is meaningless, it is marketing jargon that is designed to deceive. The claim that it supports “the body’s natural elimination and detoxification processes, and helps maintain healthy digestion” is baseless. It is a false health claim that, prima facie, is contrary to the Unfair Trading law, and/or European regulation on nutrition and health claims made on food, ref 1924/2006 , and which therefore should result in prosecution.
Two more Duchy herbals
Duchy are selling also Echinacea and Hypericum (St John’s Wort).
The evidence that Echinacea helps with colds is, to put it mildly, very marginal.
Of St John’s Wort, NCCAM says
“There is some scientific evidence that St. John’s wort is useful for treating mild to moderate depression. However, two large studies, one sponsored by NCCAM, showed that the herb was no more effective than placebo in treating major depression of moderate severity.”
As well as having dubious effectiveness it is well known that St John’s Wort can interact with many other drugs, a hazard that is not mentioned by Duchy Originals
These two are slightly different because they appear to have the blessing of the MHRA.
The behaviour of the MHRA in ignoring the little question of whether the treatment works or not has been condemned widely. But at least the MHRA are quite explicit. This is what the MHRA says of St. John’s Wort (my emphasis).
“This registration is based exclusively upon evidence of traditional use of Hypericum perforatum L. as a herbal medicine and not upon data generated from clinical trials.. There is no requirement under the Traditional Herbal Registration scheme to prove scientifically that the product works.“
But that bit about “There is no requirement under the Traditional Herbal Registration scheme to prove scientifically that the product works” does not appear in the Duchy Originals advertisement. On the contrary, this is what they say.

Yes, they claim that “the two tinctures [echinacea and hypericum] -in terms of their safety, quality and efficacy -by the UK regulatory authorities”
That is simply not true.
On the contrary, anyone without specialist knowledge would interpret bits like these as claims that there will be a health benefit.
![]()
That is claim to benefit your health. So are these.

Who makes them?

Michael McIntyre is certainly a high profile herbalist.
He was founder president of the European Herbal Practitioners Association and a trustee of the Prince of Wales’s Foundation for Integrated Medicine. It seems that he a great believer in the myth of “detox”, judging by his appearance on the Firefly tonics web site. They will sell you
“Natural healthy energy” in a drink
That’s what we wanted…
A Wake up for that drowsy afternoon… Detox for a dodgy Friday morning…
Sharpen up for that interminable meeting.
We left the herbs to our wonderful herbalists.
Their De-tox contains lemon, lime, ginger, sarsparilla and angelica. I expect it tastes nice. All the rest is pure marketing rubbish. It does not speak very well of Michael McIntyre that he should lend his name to such promotions.
Nelsons, who actually make the stuff, is better known as a big player in the great homeopathic fraud business. They will sell you 30C pills of common salt at £4.60 for 84. Their main health-giving virtue is that they’re salt free.
If you want to know what use they are, you are referred here, where it is claimed that it is “used to treat watery colds, headaches, anaemia, constipation, and backache”. Needless to say there isn’t a smidgeon of reason to believe it does the slightest good for them.
And remember what Nelson’s advisor at their London pharmacy told BBC TV while recommending sugar pills to prevent malaria?
“They make it so your energy doesn’t have a malaria-shaped hole in it so the malarial mosquitos won’t come along and fill that in.”
You couldn’t make it up.
The Prince of Wales has some sensible things to say in other areas, such as the world’s over-reliance on fossil fuels. Even his ideas about medicine are, no doubt, well-intentioned. It does seem a shame that he just can’t get the hang of the need for evidence. Wishful thinking just isn’t enough.
Follow-up
Some more interesting reading about the Prince of Wales.
Michael Baum’s An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong”
Gerald Weissman’s essay Homeopathy: Holmes, Hogwarts, and the Prince of Wales.
Channel 4 TV documentary HRH “meddling in politics”
11 March 2009 The MHRA have censured Duchy Originals for the claims made for these products. and in May 2009, two complaints to the Advertising Standards Authority were upheld.
I’m perfectly happy to think of alternative medicine as being a voluntary, self-imposed tax on the gullible (to paraphrase Goldacre again). But only as long as its practitioners do no harm and only as long as they obey the law of the land. Only too often, though, they do neither.
When I talk about law, I don’t mean lawsuits for defamation. Defamation suits are what homeopaths and chiropractors like to use to silence critics. heaven knows, I’ve becomes accustomed to being defamed by people who are, in my view. fraudsters, but lawsuits are not the way to deal with it.

I’m talking about the Trading Standards laws Everyone has to obey them, and in May 2008 the law changed in a way that puts the whole health fraud industry in jeopardy.
The gist of the matter is that it is now illegal to claim that a product will benefit your health if you can’t produce evidence to justify the claim.
I’m not a lawyer, but with the help of two lawyers and a trading standards officer I’ve attempted a summary. The machinery for enforcing the law does not yet work well, but when it does, there should be some very interesting cases.
The obvious targets are homeopaths who claim to cure malaria and AIDS, and traditional Chinese Medicine people who claim to cure cancer.
But there are some less obvious targets for prosecution too. Here is a selection of possibilities to savour..
- Universities such as Westminster, Central Lancashire and the rest, which promote the spreading of false health claims
- Hospitals, like the Royal London Homeopathic Hospital, that treat patients with mistletoe and marigold paste. Can they produce any real evidence that they work?
- Edexcel, which sets examinations in alternative medicine (and charges for them)
- Ofsted and the QCA which validate these exams
- Skills for Health and a whole maze of other unelected and unaccountable quangos which offer “national occupational standards” in everything from distant healing to hot stone therapy, thereby giving official sanction to all manner of treatments for which no plausible evidence can be offered.
- The Prince of Wales Foundation for Integrated Health, which notoriously offers health advice for which it cannot produce good evidence
- Perhaps even the Department of Health itself, which notoriously referred to “psychic surgery” as a profession, and which has consistently refused to refer dubious therapies to NICE for assessment.
The law, insofar as I’ve understood it, is probably such that only the first three or four of these have sufficient commercial elements for there to be any chance of a successful prosecution. That is something that will eventually have to be argued in court.
But lecanardnoir points out in his comment below that The Prince of Wales is intending to sell herbal concoctions, so perhaps he could end up in court too.
The laws
We are talking about The Consumer Protection from Unfair Trading Regulations 2008. The regulations came into force on 26 May 2008. The full regulations can be seen here, or download pdf file. They can be seen also on the UK Statute Law Database.
The Office of Fair Trading, and Department for Business, Enterprise & Regulatory Reform (BERR) published Guidance on the Consumer Protection from Unfair Trading Regulations 2008 (pdf file),
Statement of consumer protection enforcement principles (pdf file), and
The Consumer Protection from Unfair Trading Regulations: a basic guide for business (pdf file).
Has The UK Quietly Outlawed “Alternative” Medicine?
On 26 September 2008, Mondaq Business Briefing published this article by a Glasgow lawyer, Douglas McLachlan. (Oddly enough, this article was reproduced on the National Center for Homeopathy web site.)
“Proponents of the myriad of forms of alternative medicine argue that it is in some way “outside science” or that “science doesn’t understand why it works”. Critical thinking scientists disagree. The best available scientific data shows that alternative medicine simply doesn’t work, they say: studies repeatedly show that the effect of some of these alternative medical therapies is indistinguishable from the well documented, but very strange “placebo effect” ”
“Enter The Consumer Protection from Unfair Trading Regulations 2008(the “Regulations”). The Regulations came into force on 26 May 2008 to surprisingly little fanfare, despite the fact they represent the most extensive modernisation and simplification of the consumer protection framework for 20 years.”
The Regulations prohibit unfair commercial practices between traders and consumers through five prohibitions:-
- General Prohibition on Unfair Commercial
Practices (Regulation 3)- Prohibition on Misleading Actions (Regulations 5)
- Prohibition on Misleading Omissions (Regulation 6)
- Prohibition on Aggressive Commercial Practices (Regulation 7)
- Prohibition on 31 Specific Commercial Practices that are in all Circumstances Unfair (Schedule 1). One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. The definition of “product” in the Regulations includes services, so it does appear that all forms medical products and treatments will be covered.
Just look at that!
| One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations” |
Section 5 is equally powerful, and also does not contain the contentious word “cure” (see note below)
Misleading actions
5.—(1) A commercial practice is a misleading action if it satisfies the conditions in either paragraph (2) or paragraph (3).
(2) A commercial practice satisfies the conditions of this paragraph—
(a) if it contains false information and is therefore untruthful in relation to any of the matters in paragraph (4) or if it or its overall presentation in any way deceives or is likely to deceive the average consumer in relation to any of the matters in that paragraph, even if the information is factually correct; and
(b) it causes or is likely to cause the average consumer to take a transactional decision he would not have taken otherwise.
These laws are very powerful in principle, But there are two complications in practice.
One complication concerns the extent to which the onus has been moved on to the seller to prove the claims are true, rather than the accuser having to prove they are false. That is a lot more favourable to the accuser than before, but it’s complicated.
The other complication concerns enforcement of the new laws, and at the moment that is bad.
Who has to prove what?
That is still not entirely clear. McLachlan says
“If we accept that mainstream evidence based medicine is in some way accepted by mainstream science, and alternative medicine bears the “alternative” qualifier simply because it is not supported by mainstream science, then where does that leave a trader who seeks to refute any allegation that his claim is false?
Of course it is always open to the trader to show that his the alternative therapy actually works, but the weight of scientific evidence is likely to be against him.”
On the other hand, I’m advised by a Trading Standards Officer that “He doesn’t have to refute anything! The prosecution have to prove the claims are false”. This has been confirmed by another Trading Standards Officer who said
“It is not clear (though it seems to be) what difference is implied between “cure” and “treat”, or what evidence is required to demonstrate that such a cure is false “beyond reasonable doubt” in court. The regulations do not provide that the maker of claims must show that the claims are true, or set a standard indicating how such a proof may be shown.”
The main defence against prosecution seems to be the “Due diligence defence”, in paragraph 17.
Due diligence defence
17. —(1) In any proceedings against a person for an offence under regulation 9, 10, 11 or 12 it is a defence for that person to prove—
(a) that the commission of the offence was due to—
(i) a mistake;
(ii) reliance on information supplied to him by another person;
(iii) the act or default of another person;
(iv) an accident; or
(v) another cause beyond his control; and
(b) that he took all reasonable precautions and exercised all due diligence to avoid the commission of such an offence by himself or any person under his control.
If “taking all reasonable precautions” includes being aware of the lack of any good evidence that what you are selling is effective, then this defence should not be much use for most quacks.
Douglas McLachlan has clarified, below, this difficult question
False claims for health benefits of foods
A separate bit of legislation, European regulation on nutrition and health claims made on food, ref 1924/2006, in Article 6, seems clearer in specifying that the seller has to prove any claims they make.
Article 6
Scientific substantiation for claims
1. Nutrition and health claims shall be based on and substantiated by generally accepted scientific evidence.
2. A food business operator making a nutrition or health claim shall justify the use of the claim.
3. The competent authorities of the Member States may request a food business operator or a person placing a product on the market to produce all relevant elements and data establishing compliance with this Regulation.
That clearly places the onus on the seller to provide evidence for claims that are made, rather than the complainant having to ‘prove’ that the claims are false.
On the problem of “health foods” the two bits of legislation seem to overlap. Both have been discussed in “Trading regulations and health foods“, an editorial in the BMJ by M. E. J. Lean (Professor of Human Nutrition in Glasgow).
“It is already illegal under food labelling regulations (1996) to claim that food products can treat or prevent disease. However, huge numbers of such claims are still made, particularly for obesity ”
“The new regulations provide good legislation to protect vulnerable consumers from misleading “health food” claims. They now need to be enforced proactively to help direct doctors and consumers towards safe, cost effective, and evidence based management of diseases.”
In fact the European Food Standards Agency (EFSA) seems to be doing a rather good job at imposing the rules. This, predictably, provoked howls of anguish from the food industry There is a synopsis here.
“Of eight assessed claims, EFSA’s Panel on Dietetic Products, Nutrition and Allergies (NDA) rejected seven for failing to demonstrate causality between consumption of specific nutrients or foods and intended health benefits. EFSA has subsequently issued opinions on about 30 claims with seven drawing positive opinions.”
“. . . EFSA in disgust threw out 120 dossiers supposedly in support of nutrients seeking addition to the FSD’s positive list.
If EFSA was bewildered by the lack of data in the dossiers, it needn’t hav been as industry freely admitted it had in many cases submitted such hollow documents to temporarily keep nutrients on-market.”
Or, on another industry site, “EFSA’s harsh health claim regime”
“By setting an unworkably high standard for claims substantiation, EFSA is threatening R&D not to mention health claims that have long been officially approved in many jurisdictions.”
Here, of course,”unworkably high standard” just means real genuine evidence. How dare they ask for that!
Enforcement of the law
Article 19 of the Unfair Trading regulations says
19. —(1) It shall be the duty of every enforcement authority to enforce these Regulations.
(2) Where the enforcement authority is a local weights and measures authority the duty referred to in paragraph (1) shall apply to the enforcement of these Regulations within the authority’s area.
Nevertheless, enforcement is undoubtedly a weak point at the moment. The UK is obliged to enforce these laws, but at the moment it is not doing so effectively.
A letter in the BMJ from Rose & Garrow describes two complaints under the legislation in which it appears that a Trading Standards office failed to enforce the law. They comment
” . . . member states are obliged not only to enact it as national legislation but to enforce it. The evidence that the government has provided adequate resources for enforcement, in the form of staff and their proper training, is not convincing. The media, and especially the internet, are replete with false claims about health care, and sick people need protection. All EU citizens have the right to complain to the EU Commission if their government fails to provide that protection.”
This is not a good start. A lawyer has pointed out to me
“that it can sometimes be very difficult to get Trading Standards or the OFT to take an interest in something that they don’t fully understand. I think that if it doesn’t immediately leap out at them as being false (e.g “these pills cure all forms of cancer”) then it’s going to be extremely difficult. To be fair, neither Trading Standards nor the OFT were ever intended to be medical regulators and they have limited resources available to them. The new Regulations are a useful new weapon in the fight against quackery, but they are no substitute for proper regulation.”
Trading Standards originated in Weights and Measures. It was their job to check that your pint of beer was really a pint. Now they are being expected to judge medical controversies. Either they will need more people and more training, or responsibility for enforcement of the law should be transferred to some more appropriate agency (though one hesitates to suggest the MHRA after their recent pathetic performance in this area).
Who can be prosecuted?
Any “trader”, a person or a company. There is no need to have actually bought anything, and no need to have suffered actual harm. In fact there is no need for there to be a complainant at all. Trading standards officers can act on their own. But there must be a commercial element. It’s unlikely that simply preaching nonsense would be sufficient to get you prosecuted, so the Prince of Wales is, sadly, probably safe.
Universities who teach that “Amethysts emit high Yin energy” make an interesting case. They charge fees and in return they are “falsely claiming that a product is able to cure illnesses”.
In my view they are behaving illegally, but we shan’t know until a university is taken to court. Watch this space.
The fact remains that the UK is obliged to enforce the law and presumably it will do so eventually. When it does, alternative medicine will have to change very radically. If it were prevented from making false claims, there would be very little of it left apart from tea and sympathy
Follow-up
New Zealand must have similar laws.
Just as I was about to post this I found that in New Zealand a
“couple who sold homeopathic remedies claiming to cure bird flu, herpes and Sars (severe acute respiratory syndrome) have been convicted of breaching the Fair Trading Act.”
They were ordered to pay fines and court costs totalling $23,400.
A clarification form Douglas McLachlan
On the difficult question of who must prove what, Douglas McLachlan, who wrote Has The UK Quietly Outlawed “Alternative” Medicine?, has kindly sent the following clarification.
“I would agree that it is still for the prosecution to prove that the trader committed the offence beyond a reasonable doubt, and that burden of proof is always on the prosecution at the outset, but I think if a trader makes a claim regarding his product and best scientific evidence available indicates that that claim is false, then it will be on the trader to substantiate the claim in order to defend himself. How will the trader do so? Perhaps the trader might call witness after witness in court to provide anecdotal evidence of their experiences, or “experts” that support their claim – in which case it will be for the prosecution to explain the scientific method to the Judge and to convince the Judge that its Study evidence is to be preferred.
Unfortunately, once human personalities get involved things could get clouded – I could imagine a small time seller of snake oil having serious difficulty, but a well funded homeopathy company engaging smart lawyers to quote flawed studies and lead anecdotal evidence to muddy the waters just enough for a Judge to give the trader the benefit of the doubt. That seems to be what happens in the wider public debate, so it’s easy to envisage it happening a courtroom.”
The “average consumer”.
(3) A commercial practice is unfair if—
(a) it contravenes the requirements of professional diligence; and
(b) it materially distorts or is likely to materially distort the economic behaviour of the average consumer with regard to the product.
It seems,therefore, that what matters is whether the “average consumer” would infer from what is said that a claim was being made to cure a disease. The legal view cited by Mojo (comment #2, below) is that expressions such as “can be used to treat” or “can help with” would be considered by the average consumer as implying successful treatment or cure.
The drugstore detox delusion. A nice analysis “detox” at .Science-based Pharmacy
Today brings a small setback for those of us interested in spreading sensible ideas about science. According to a press release
“The BMJ Group is to begin publishing a medical journal on acupuncture from next year, it was announced today (Tuesday 11 November 2008).
This will be the first complementary medicine title that the BMJ Group has published.”
And they are proud of that? What one earth is going on? The BMJ group is a publishing company which says, of itself,
“Our brand stands for medical credibility. We are one of the world’s best known and most respected medical publishers.”
Well perhaps it used to be.
They have certainly picked a very bad moment for this venture. In the last year there have been at least five good books that assess the evidence carefully and honestly. Of these, the ones that are perhaps the best on the subject of acupuncture are Singh & Ernst’s Trick or Treatment and Barker Bausell’s Snake Oil Science. Both Ernst and Bausell have first hand experience of acupuncture research. And crucially, none of these authors has any financial interest in whether the judgement goes for acupuncture or against it.
Here are quotations from Singh & Ernst’s conclusions
“Reliable conclusions from systematic reviews make it clear that acupuncture does not work for a whole range of conditions, except as a placebo.”
“There are some high quality trials that support the use of acupuncture for some types of pain and nausea, but there are also high quality trials that contradict this conclusion. In short, the evidence is neither consistent nor convincing – it is borderline.”
The House of Lords’ report in 2000 tended to give acupuncture the benefit of the (very considerable) doubt that existed at the time the report was written. Since that time there have been a lot of very well-designed trials of acupuncture.
Now it is quite clear that, for most (and quite possibly all) conditions, acupuncture is no more than a particularly theatrical placebo. Perhaps that is not surprising insofar as the modern western practice of acupuncture owes more to Chinese nationalistic propaganda that started in the time of Mao-Tse Tung than it owes to ancient wisdom (which often turns out to be bunk anyway).
The BMJ Group has decided to endorse acupuncture at a time when it is emerging that the evidence for any specific effect is very thin indeed. Well done.
The journal in question is this.
Acupuncture in Medicine is a quarterly title, which aims to build the evidence base for acupuncture. It is currently self-published by the British Medical Acupuncture Society (BMAS).
One good thing can be said about the Society and the Journal. That is that they don’t espouse all the mumbo-jumbo about ‘meridians’ and ‘Qi’. This, of course, puts them at odds with the vast majority of acupuncture teaching. This sort of internecine warfare between competing sects is characteristic of all sorts of alternative medicine. But that is just ideology. What matters is whether or not sticking needles in you is actually anything more than a placebo.
British Medical Acupuncture Society (BMAS)
The British Medical Acupuncture Society (BMAS). is “a registered charity established to encourage the use and scientific understanding of acupuncture within medicine for the public benefit.”. The phrase “encourage the use” suggests that they do not even envisage the possibility that it might not work. Their web site includes these claims.
Acupuncture can help in a variety of conditions:
- Pain relief for a wide range of painful conditions
- Nausea, especially postoperative nausea and vomiting
- Overactive bladder, also known as bladder detrusor instability
- Menstrual and menopausal problems, eg period pains and hot flushes
- Allergies such as hay fever and some types of allergic rashes
- Some other skin problems such as ulcers, itching and localised rashes
- Sinus problems and more
Presumably the word “help” is chosen carefully to fall just short of “cure”. The claims are vaguely worded, but let’s see what we can find about them from systematic reviews. It appears that the BMAS is being rather optimistic about the evidence.
BMJ Clinical Evidence is considered reliable and is particular interesting because it is owned by the BMJ Publishing Group.
Low Back Pain (chronic) Acupuncture is listed as being of “unknown effectiveness”.
Dysmenorrhoea Acupuncture is listed as being of “unknown effectiveness”.
Osteoarthritis of the knee. Acupuncture is listed as being of “unknown effectiveness”.
Psoriasis (chronic plaque) Acupuncture is listed as being of “unknown effectiveness”.
Neck pain “Acupuncture may be more effective than some types of sham treatment (not further defined) or inactive treatment (not further defined) at improving pain relief at the end of treatment or in the short term (less than 3 months), but not in the intermediate term (not defined) or in the long term (not defined)”
Headache (chronic tension-type) Acupuncture is listed as being of “unknown effectiveness”.
What about the greatest authority, the Cochrane Reviews?
Cochrane Reviews
Low back pain The data do not allow firm conclusions about the effectiveness of acupuncture for acute low-back pain. For chronic low-back pain, acupuncture is more effective for pain relief and functional improvement than no treatment or sham treatment immediately after treatment and in the short-term only. Acupuncture is not more effective than other conventional and “alternative” treatments. The data suggest that acupuncture and dry-needling may be useful adjuncts to other therapies for chronic low-back pain. Because most of the studies were of lower methodological quality, there certainly is a further need for higher quality trials in this area.
Chronic asthma. There is not enough evidence to make recommendations about the value of acupuncture in asthma treatment. Further research needs to consider the complexities and different types of acupuncture.
But most of the vaguely-worded claims made by BMAS have not been the subject of Cochrane reviews. The obvious interpretation of that is that there is not enough evidence to make it worth writing a review. In which case, why does BMAS claim that acupuncture can “help”?
Bandolier is another excellent source of high quality information, This was their view in September 2006
“Large, high-quality randomised trials of acupuncture have been published since the reviews. In fibromyalgia, chemotherapy-induced nausea and vomiting, breech presentation, tension headache, and migraine, all were negative compared with sham acupuncture. One in osteoarthritis of the knee, had statistical improvement over sham acupuncture at three months, but not later. Both large trials and this review of reviews come to the same general conclusion; that over a whole range of conditions and outcomes acupuncture cannot yet be shown to be effective.”
After thousands of years of acupuncture (or at least almost 40 years in the West) there seems to be very little to show for it.
The journal: Acupuncture in Medicine
What about the journal in question? Like all journals devoted to alternative medicine, it claims to be evidence-based. And like all journals devoted to alternative medicine it suffers from a fatal conflict of interest. If this journal were ever to conclude that acupuncture is a placebo, it would destroy the journal and the livelihoods of many of the people who write for it.
Scanning the first three issues of 2008 shows that it is very much like other alternative medicine journals. Most of the papers don’t address the critical question, is it a placebo. And most papers end up rather limply, with a statement along the lines “acupuncture may be useful for ***. More research is needed.”
The editor in chief of the journal is Dr Adrian White, and its editor is Michael Cummings. White is quoted by Ernst in the Guardian in 2004.
“We need to provide hard evidence to support what we all see in our clinics every day: that the modern approach to acupuncture works, and is highly relevant to the new, patient-centred NHS.” .
That means the answer is assumed in advance. That just isn’t science.. ‘We know the answer, all we have to do now is get some evidence’.
Why should the BMJ Group want to do a thing like this?
The press release says
Commenting on the move, BMJ and BMJ Journals Publishing Director, Peter Ashman, said “The journal is a good complement for our existing portfolio of journals and we’re certain that the Society’s members and other subscribers will appreciate the benefits of the decision the BMAS has made on their behalf.”
He continued: “The BMAS is ambitious for its journal to grow and flourish and we’re looking forward to working with the Society to develop an editorial and commercial strategy which will achieve the aims of BMAS and those of its members, while reaching out to the wider global community interested in this fascinating area of medicine.”
Yes, you got it. Money. The same motive that causes some vice-chancellors to bring their university into disrepute by awarding BSc degrees in subjects that are not only not science, but which are oftenly openly anti-science.
Conscience doesn’t seem to bother these people, so let’s put the problem in purely cash terms.
Both the BMJ Group and the vice-chancellors will have to decide whether the cash they gain is sufficient to counterbalance the corrosive effects of their actions on their own reputations.
Follow-up
Only a couple of days later, two new trials show acupuncture is no different from sham controls for helping IVF pregnancy rates. James Randerson in the Guardian writes thus.
“Acupuncture aimed at improving IVF success rates is widely offered by fertility clinics in the UK. In the first of the studies, researchers in Hong Kong split 370 women receiving IVF into two groups. One group received real acupuncture before and after having an IVF embryo implanted into their uterus. The other had the same procedure, except the treatment used retractable needles that did not penetrate the skin.”
“Of the 185 who received the sham treatment, 91 achieved a clinical pregnancy (foetal heartbeat identified using ultrasound) and 71 had a successful delivery. This compared with 72 clinical pregnancies in the true acupuncture group and 55 live births. The differences between the groups were not statistically significant.”
“In a second study, researchers in Chicago used a similar design in which 124 women received true or sham acupuncture. The control group had their skin punctured by real acupuncture needles, but not at genuine “Qi-lines” on the body. In the true acupuncture group, 43.9% achieved a clinical pregnancy, compared with 55.2% of the women given the sham treatment. “
The original paper for the first study can be seen here.
Alfred Joseph Clark FRS held the established chair of Pharmacology at UCL from 1919 to 1926, when he left for Edinburgh. In the 1920s and 30s, Clark was a great pioneer in the application of quantitative physical ideas to pharmacology. As well as his classic scientific works, like The Mode of Action of Drugs on Cells (1933) he wrote, and felt strongly, about the fraud perpetrated on the public by patent medicine salesmen. In 1938 (while in Edinburgh) he published a slim volume called Patent Medicines. The parallels with today are astonishing.
 
Alfred Joseph Clark FRS (1885 – 1941) |
 |
I was lucky to be given a copy of this book by David Clark, A.J. Clark’s eldest son, who is now 88. I visited him in Cambridge on 17 September 2008, because he thought that, as holder of the A.J. Clark chair at UCL from 1985 to 2004, I’d be a good person to look after this and several other books from his father’s library. They would have gone to the Department of Pharmacology if we still had one, but that has been swept away by mindless administrators with little understanding of how to get good science.
Quotations from the book are in italic, and are interspersed with comments from me.
The book starts with a quotation from the House of Commons Select Committee report on Patent Medicines. The report was submitted to the House on 4 August 1914, so there is no need to explain why it had little effect. The report differs from recent ones in that it is not stifled by the sort of political correctness that makes politicians refer to fraudsters as “professions”.
The problem
“2.2 The situation, therefore, as regards the sale and advertisement of proprietary medicines and articles may be summarised as follows:
For all practical purposes British law is powerless to prevent any person from procuring any drug, or making any mixture, whether patent or without any therapeutical activity whatever (as long as it does not contain a scheduled poison), advertising it in any decent terms as a cure for any disease or ailment, recommending it by bogus testimonials and the invented opinions and facsimile signatures of fictitious physicians, and selling it under any name he chooses, on payment of a small stamp duty. For any price he can persuade a credulous public to pay.”
Select Committee on Patent Medicines. 1914
“The writer has endeavoured in the present article to analyse the reasons for the amazing immunity of patent medicines form all attempts to curb their activity, to estimate the results and to suggest the obvious measures of reform that are needed.”
| Clark, writing in 1938, was surprised that so little had changed since 1914. What would he have thought if he had known that now, almost 100 years after the 1914 report, the fraudsters are still getting away with it? Chapter 2 starts thus. |
 |
THE LAW
The Select Committee appointed by the House of Commons in 1914 ‘to consider and inquire into the question of the sale of Patent and Proprietary Medicines’ stated its opinion in 28 pages of terse and uncompromising invective. Its general conclusions were as follows:
That the trade in secret remedies constituted a grave and widespread public evil.
That the existing law was chaotic and had proved inoperative and that consequently the traffic in secret remedies was practically uncontrolled.
In particular it concluded ‘”that this is an intolerable state of things and that new legislation to deal with it, rather than merely the amendment of existing laws, is urgently needed in the public interest.”
The “widespread public evil”continues almost unabated, and rather than introduce sensible legislation to cope with it, the government has instead given a stamp of approval for quackery by introducing utterly ineffective voluntary “self-regulation”.
Another Bill to deal with patent medicines was introduced in 1931, without success, and finally in 1936, a Medical and Surgical Appliances (Advertisement) Bill was introduced. This Bill had a very limited scope. Its purpose was to alleviate some of the worst abuses of the quack medicine trade by prohibiting the advertisement of cures for certain diseases such as blindness, Bright’s disease [nephritis] , cancer, consumption [tuberculosis], epilepsy, fits, locomotor ataxy, fits, lupus or paralysis.
The agreement of many interests was secured for this measure. The president of the Advertising Association stated that the proposed Bill would not affect adversely any legitimate trade interest. Opposition to the Bill was, however, whipped up amongst psychic healers, anti-vivisectionists and other opponents of medicine and at the second reading in March 1936, the Bill was opposed and the House was counted out during the ensuing debate. The immediate reason for this fate was that the Bill came up for second reading on the day of the Grand National! This is only one example of the remarkable luck that has attended the patent medicine vendors.
(Page 14).
The “remarkable luck” of patent medicine vendors continues to this day, Although, in principle, advertisement of cures for venereal diseases was banned in 1917, and for cancer in 1939, it takes only a few minutes with Google to find that these laws are regularly flouted by quacks, In practice quacks get away with selling vitamin pills for AIDS, sugar pills for malaria and homeopathic pills for rabies, polio anthrax and just about anything else you can think of. Most of these advertisements are contrary to the published codes of ethics of the organisations to which the quack in question belongs but nothing ever happens.
Self-regulation simply does not work, and there is still no effective enforcement even of existing laws..
“It has already been stated that British law allows the advertiser of a secret remedy to tell any lie or make any claim that he fancies will sell his goods and the completeness of this licence is best illustrated by the consideration of a few specific points.
Advertisements for secret remedies very frequently contain a list of testimonials from medical men, which usually are in an anonymous form, stating that ………….. M.D., F.R.C.S., has found the remedy infallible. Occasionally, however, the name and address of a doctor is given and anyone unaware of the vagaries of English law would imagine that such use of a doctor’s name and professional reputation could not be made with impunity without his consent. In 1899, however, the Sallyco Mineral Water Company advertised that ‘Dr. Morgan Dochrill, physician to St. John’s Hospital, London and many of the leading physicians are presenting ‘Sallyco’ as an habitual drink. Dr. Dochrill says nothing has done his gout so much good.
Dr. Dochrill, whose name and title were correctly stated above, sued the company but failed in his case. ”
“The statement that the law does not prevent the recommending of a secret remedy by the use of bogus testimonials and facsimile signatures of fictitious physicians is obviously an understatement since it is doubtful how far it interferes with the use of bogus testimonials from real physicians.”
Dodgy testimonials are still a mainstay of dodgy salesman. One is reminded of the unauthorised citation of testimonials from Dr John Marks and Professor Jonathan Waxman by Patrick Holford to aid his sales of unnecessary vitamin supplements. There is more on this at Holfordwatch.
The man in the street knows that the merits of any article are usually exaggerated in advertisements and is in the habit of discounting a large proportion of such claims, but, outside the realm of secret remedies, the law is fairly strict as regards definite misstatements concerning goods offered for sale and hence the everyday experience of the man in the street does not prepare him for dealing with advertisements which are not merely exaggerations but plain straightforward lies from beginning to end.
Scientific training is undoubtedly a handicap in estimating popular gullibility as regards nostrums. One imagines that no one today would be willing to spend money on pills guaranteed to prevent earthquakes but yet the claims of many of the remedies offered appear equally absurd to anyone with an elementary
knowledge of physiology or even of chemistry. A study of the successes and failures suggests that success depends chiefly on not over-rating the public intelligence. (Page 34)
This may have changed a bit since A.J. Clark was writing in 1938. Now the main clients of quacks seem to be the well-off “worried-well”. But it remains as true as ever that “Scientific training is undoubtedly a handicap in estimating popular gullibility as regards nostrums.” In 2008, it is perhaps more a problem of Ben Goldacre’s dictum ““My basic hypothesis is this: the people who run the media are humanities graduates with little understanding of science, who wear their ignorance as a badge of honour.”
Clark refers (page 36) to a successful conviction for fraud in the USA in 1917. The subject was a widely advertised ‘get fat quick’ pill that contained lecithin, proteins and sugar. The BMA analysis (in 1912)
suggested that the cost of the ingredients in a box of 30 tablets sold for 4/6 was 1 1/4 d. [4/6 meant 4 shillings and six pence, or 22.5 pence since 1971, and 1 1/4 old pence, a penny farthing, is 0.52 new pence]. He comments thus.
The trial revealed many interesting facts. The formula was devised after a short consultation with the expert of one of the largest drug manufacturers in the U.S.A. This firm manufactured the tablets and sold them to the proprietary medicine company at about 3/- per 1000, whilst they were retailed to the public at the rate of £7 10s. per 1000. The firm is estimated to have made a profit of about $3,000,000.
These trials in the U.S.A. revealed the fact that in a considerable proportion of cases the ‘private formula’ department of the large and well known drug firm already mentioned had first provided the formula for the nostrum and subsequently had prepared it wholesale.
Nothing much has changed here either. The alternative medicine industry (and it is a very big industry) is fond of denouncing the evils of the pharmaceutical industry, and sadly, occasionally they are right. One of the less honest practices of the pharmaceutical industry (though one never mentioned by quacks) is buying heavily into alternative medicine. Goldacre points out
“there is little difference between the vitamin and pharmaceutical industries. Key players in both include multinationals such as Roche and Aventis; BioCare, the vitamin pill producer that media nutritionist Patrick Holford works for, is part-owned by Elder Pharmaceuticals.”
And then. of course, there is the deeply dishonest promotion by Boots the Chemists of homeopathic miseducation, of vitamins and of CoQ10 supplements.
The manner in which secret remedies can survive repeated exposure is shown by the following summary of the life history of a vendor of a consumption [tuberculosis] cure.
1904, 1906: Convicted of violating the law in South Africa.
1908: Exposed in British Medical Association report and also attacked by Truth.
1910: Sued by a widow. The judge stated: ‘I think this is an intentional and well-considered fraud. It is a scandalous thing that poor people should be imposed upon and led to part with their money, and to hope that those dear to them would be cured by those processes which were nothing but quack remedies and had not the slightest value of any kind.’
1914: A libel action against the British Medical Association was lost.
1915 The cure was introduced into the United States.
1919 The cure was sold in Canada.
1924 Articles by men with medical qualifications appeared in the Swiss medical journal boosting
the cure.
Secret remedies have a vitality that resembles that of the more noxious weeds and the examples mentioned suggest that nothing can do them any serious harm.
Most of the time, quacks get away with claims every bit as outrageous today. But Clark does give one example of a successful prosecution. It resulted from an exposé in the newspapers -wait for it -in the Daily Mail.
There is, however, one example which proves that a proprietary remedy can be squashed by exposure if this is accompanied by adequate publicity.
The preparation Yadil was introduced as an antiseptic and was at first advertised to the medical profession. The proprietor claimed that the remedy was not secret and that the active principle was ‘tri-methenal allylic carbide’. The drug acquired popularity in the influenza epidemic of 1918 and the proprietor became more and more ambitious in his therapeutic claims. The special virtue claimed for Yadil was that it would kill any harmful organism that had invaded the body. A more specific claim was that consumption in the first stage was cured with two or three pints whilst advanced cases might require a little more. Other advertisements suggested that it was a cure for most known diseases from cancer downwards.
These claims were supported by an extraordinarily intense advertising campaign. Most papers, and even magazines circulating amongst the wealthier classes, carried full page and even double page advertisements. The Daily Mail refused these advertisements and in 1924 published a three column article by Sir William Pope, professor of Chemistry in the University of Cambridge. He stated that
the name ‘tri-methenal allylic carbide’ was meaningless gibberish and was not the chemical definition of any known substance. He concluded that Yadil consisted of :
‘About one per cent of the chemical compound formaldehyde.
About four per cent of glycerine.
About ninety-five per cent of water and, lastly, a smell.
He calculated that the materials contained in a gallon cost about 1/6, whilst the mixture was sold at £4 10s. per gallon.
This exposure was completely successful and the matter is of historic interest in that it is the only example of the career of a proprietary medicine being arrested by the action of the Press.
Clark goes on to talk of the law of libel.
“On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”
The law of libel to this day remains a serious risk to freedom of speech of both individuals and the media. Its use by rogues to suppress fair comment is routine. My first encounter was when a couple of herbalists
threatened to sue UCL because I said that the term ‘blood cleanser’ is gobbledygook. The fact that the statement was obviously true didn’t deter them for a moment. The herbalists were bluffing no doubt, but they caused enough nuisance that I was asked to take my pages off UCL’s server. A week later I was invited back but by then I’d set up a much better blog and the publicity resulted in an enormous increase in readership, so the outcome was good for me (but bad for herbalists).
It was also good in the end for Andy Lewis when his immortal page “The gentle art of homoeopathic killing” (about the great malaria scandal) was suppressed. The Society of Homeopaths’ lawyers didn’t go for him personally but for his ISP who gave in shamefully and removed the page. As a result the missing page reappeared in dozens of web sites round the world and shot to the top in a Google search.
Chiropractors are perhaps the group most likely to try to suppress contrary opinions by law not argument. The only lawyers’ letter that has been sent to me personally, alleged defamation in an editorial that I wrote for the New Zealand Medical Journal. That was a little scary, but the journal stuck up for its right to speak and the threat went away after chiropractors were allowed right of reply (but we got the last word).
Simon Singh, one of the best science communicators we have, has not been so lucky. He is going to have to defend in court an action brought by the British Chiropractic Association because of innocent opinions expressed in the Guardian.
Chapter 6 is about “The harm done by patent medicines”. It starts thus.
“The trade in secret remedies obviously represents a ridiculous waste of money but some may argue that, since we are a free country and it pleases people to waste their money in this particular way, there is no call for any legislative interference. The trade in quack medicines cannot, however, be regarded as a harmless one. The Poisons Acts fortunately prevent the sale of a large number of dangerous drugs, but there are numerous other ways in which injury can be produced by these remedies.”
The most serious harm, he thought, resulted from self-medication, and he doesn’t mince his words.
“The most serious objection to quack medicines is however that their advertisements encourage self-medication as a substitute for adequate treatment and they probably do more harm in this than in any other manner.
The nature of the problem can best be illustrated by considering a simple example such as diabetes. In this case no actual cure is known to medicine but, on the other hand, if a patient is treated adequately by insulin combined with appropriate diet, he can be maintained in practically normal health, in spite of his disability, for an indefinite period. The expectation of life of the majority of intelligent diabetics, who make no mistakes in their regime, is not much less than that of normal persons. The regime is both irksome and unpleasant, but anyone who persuades diabetics to abandon it, is committing manslaughter as certainly as if he fired a machine gun into a crowded street.
As regards serious chronic disease the influence of secret remedies may be said to range from murderous to merely harmful.
‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous, since they are likely to cause the death of anyone who is unfortunate enough to believe in their efficacy and thus delay adequate treatment until too late.
The phrase “‘Cures for consumption, cancer and diabetes may fairly be classed as murderous” made Clark himself the victim of suppression of freedom of speech by lawyers. His son, David Clark, wrote of his father in “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3)
“Although tolerant of many human foibles, A. J. had always disapproved fiercely of quacks, particularly the charlatans who sold fraudulent medicines. During his visits to London he met Raymond Postgate, then a crusading left wing journalist, who persuaded A.J. to write a pamphlet which was published in an ephemeral series called ‘Fact‘ in March 1938. It was a lively polemical piece. . To A.J.’s surprise and dismay he was sued for libel by a notorious
rogue who peddled a quack cure for for tuberculosis. This man said that A.J.’s remarks (such as “‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”) were libellous and would damage his business. A.J. was determined to fight, and he and Trixie decided to put their savings at stake if necessary. The B.M.A. and the Medical Defence Union agreed to support him and they all went to lawyers. He was shocked when they advised him that he would be bound to lose for he had damaged the man’s livelihood! Finally, after much heart searching, he made an apology, saying that he had not meant that particular man’s nostrum”
Talk about déjà vu!
On page 68 there is another very familiar story. It could have been written today.
“The fact that the public is acquiring more knowledge of health matters and is becoming more suspicious of the cruder forms of lies is also helping to weed out the worst types of patent medicine advertisements. For example, in 1751 a bottle of oil was advertised as a cure for scurvy, leprosy and consumption but today such claims would not be effective in promoting the sale of a remedy. The modern advertiser would probably claim that the oil was rich in all the vitamins and the elements essential for life and would confine his claims to a statement that it would alleviate all minor forms of physical or mental ill-health.
The average patent medicine advertised today makes plausible rather than absurd claims and in general the advertisements have changed to conform with a change in the level of the public’s knowledge.
It is somewhat misleading, however, to speak of this as an improvement, since the law has not altered and hence the change only means that the public is being swindled in a somewhat more skilful manner.
The ideal method of obtaining an adequate vitamin supply is to select a diet containing an abundant supply of fresh foods, but unfortunately the populace is accustomed to live very largely on preserved or partially purified food stuffs and such processes usually remove most of the vitamins.”
The first part of the passage above is reminiscent of something that A.J Clark wrote in the BMJ in 1927. Nowadays it is almost unquotable and I was told by a journal editor that it was unacceptable even with asterisks. That seems to me a bit silly. Words had different connotations in 1927.
“The less intelligent revert to the oldest form of belief and seek someone who will make strong magic for them and defeat the evil spirits by some potent charm. This is the feeling to which the quack appeals; he claims to be above the laws of science and to possess some charm for defeating disease of any variety.
The nature of the charm changes with the growth of education. A naked n****r howling to the beat of a tom-tom does not impress a European, and most modern Europeans would be either amused or disgusted by the Black mass that was popular in the seventeenth century. Today some travesty of physical science appears to be the most popular form of incantation.”
A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927
Apart from some of the vocabulary, what better description could one have of the tendency of homeopaths to harp on meaninglessly about quantum theory or the “scienciness” and “referenciness” of
modern books on nutritional therapy?
So has anything changed?
Thus far, the outcome might be thought gloomy. Judging by Clark’s account, remarkably little has changed since 1938, or even since 1914. The libel law in the UK is as bad now as it was then. Recently the United Nations Human Rights Committee said UK laws block matters of public interest and encourage libel tourism (report here, see also here). It is unfit for a free society and it should be changed.
But there are positive sides too. Firstly the advent of scientific bloggers has begun to have some real influence. People are no longer reliant on journalists to interpret (or, often, misinterpret) results for them. They can now get real experts and links to original sources. Just one of these, Ben Goldacre’s badscience.net, and his weekly column in the Guardian has worked wonders in educating the public and improving journalism. Young people can, and do, contribute to the debate because they can blog anonymously if they are frightened that their employer might object.
Perhaps still more important, the law changed this year. Now, at last, it may be possible to prosecute successfully those who make fraudulent health claims. Sad to say, this was not an initiative of the UK government, which remains as devoted as ever to supporting quacks. Remember that, quite shamefully, the only reason given by the Medicines and Health Regulatory Authority (MHRA) gave for allowing false labelling of homeopathic pills was to support the “homeopathic industry”. They suggested (falsely) that the EU required them to take this irresponsible step, which was condemned by just about every scientific organisation. But the new unfair trading regulations did come from the EU. After almost 100 years since the 1914 report, we have at last some decent legislation. Let’s hope it’s enforced.
Postcript
The back cover of the series of ‘Fact‘ books in which A.J. Clark’s article appeared is reproduced below, simply because of the historical portrait of the 1930s that it gives.
Follow-up
This post got a lot of hits from Ben Goldacre’s miniblog which read
- Prof David Colquhoun gets into a time machine and meets himself
A truly classic DC post.
Thanks, Ben.
After the announcement that the University of Central Lancashire (Uclan) was suspending its homeopathy “BSc” course, it seems that their vice chancellor has listened to the pressure, both internal and external, to stop bringing his university into disrepute.
An internal review of all their courses in alternative medicine was announced shortly after the course closure. Congratulations to Malcolm McVicar for grasping the nettle at last. Let’s hope other universities follow his example soon.
I have acquired, indirectly, a copy of the announcement of the welcome news.
| Homeopathy, Herbalism and cupuncture Concern has been expressed by some colleagues as to whether the University should offer courses in homeopathy, Herbalism and Acupuncture. Therefore, to facilitate proper discussion on this matter I have set up a working party to review the issues. I have asked Eileen Martin, Pro Vice-Chancellor and Dean of the Faculty of Health, to lead this working party and report to me as soon as possible. Whilst the review is taking place, we need to recognise that there are students and staff studying and teaching on these courses which have satisfied the University’s quality assurance procedures and been duly validated. I would therefore ask that colleagues would refrain from comment or speculation which would cause concern to these students and staff. Staff who wish to express their views on this issue should direct these to Eileen Martin, by the end of September. Regards Malcolm McVicar Vice-Chancellor |
Times Higher Education today reports
“The University of Central Lancashire is to review all its courses in homoeopathy, herbalism and acupuncture after some staff said it should not be offering degrees in “quackery”, Times Higher Education has learnt.
A university spokesman said: “As a university we value and practise transparency and tolerance and welcome all academic viewpoints.”
(Later, an almost identical version of the story ran on the Times Online.)
So far, so good. But of course the outcome of a committee depends entirely on who is appointed to it. Quite often such committees do no more than provide an internal whitewash.
It does seem a bit odd to appoint as chair the dean of the faculty where all these course are run, and presumably generate income. Eileen Martin has often appeared to be proud of them in the past. Furthermore, the whole investigation will (or should) turn on the assessment of evidence. It needs some knowledge of the design of clinical trials and their statistical analysis, As far as I can see, Ms Martin has essentially no research publications whatsoever.
I also worry about a bit about “satisfied the University’s quality assurance procedures and been duly validated”. One point of the investigation should be recognise frankly that the validation process is entirely circular, and consequently worth next to nothing. It must be hard for a vice-chancellor to admit that, but it will be an essential step in restoring confidence in Uclan.
Let’s not prejudge though. If there are enough good scientists on the committee, the result will be good.
I hope that transparency extends to letting us know who will be doing the judging. Everything depends on that.
Follow-up
Well well, there’s a coincidence, Once again, the week after a there is an announcement about degrees in witchcraft, what should pop up again in the column of the inimitable Laurie Taylor in THE. The University of Poppleton’s own Department of Palmistry.
| Letter to the editor
Dear Sir I was shocked to see yet another scurrilous attack upon the work of my department in The Poppletonian. Although Palmistry is in its early days as an academic discipline it cannot hope to progress while there are people like your correspondent who insist on referring to it as “a load of superstitious nonsense which doesn’t deserve a place on the end of the pier let alone in a university”. A large number of people claim to have derived considerable benefit from learning about life lines, head lines and heart lines and the role of the six major mounts in predicting their future. All of us in the Palmistry Department believe it vitally important that these claims are rigorously examined. How else can science advance? Yours sincerely, |
Samuel Hahnemann (1755 – 1843) was the originator of homeopathy. He was clearly a well-intentioned man.. There is good reason to believe that he thought dilution could not go on for ever, but he died 22 years before it became possible to calculate that his favourite 30C dilution already contained nothing at all.

| The bible of homeopaths is Hahnemann’s Organon der rationellen Heilkunde, “Organon of the Medical Art”. His views on dosage, as expressed in the six editions of this book are almost as self-contradictory as the other bible. Hahnemann’s writing about ‘vital spirits’ sounds very silly now, but it is language that was quite common at the end of the 18th century, before much was known about medicine or physiology. But his interest in chemistry was entirely sensible. |  |
Before 1800 Hahnemann started out with the very high doses that were conventional at the time. Unlike most of his contemporaries, he was smart enough to realise that giving 50 g of antimony was killing people so he kept reducing the dose until it was no longer toxic. Unfortunately he (like almost everyone else at the time) didn’t know about controls so he mistook lack of toxicity (because the dose was zero) for a beneficial effect. Nonetheless, for most of his life he did not advocate the extreme dilutions that many modern homeopaths use routinely.
In The Life and Letters of Dr Samuel Hahnemann by Thomas Lindsley Bradford, M.D.(or see Google books edition of the Organon), there is an interesting passage. According to the edition here pp. 237 – 238), this was a note attached to para. #283 in the first edition of the Organon.
| ” The doctrine of the divisibility of matter teaches us that we cannot make a part so small that it shall cease to be something, and that it shall not share all the properties of the whole.” |
Here Hahnemann refers to the doctrine of divisibility, but appears to be saying that dilution can go on for ever. But he also says something that directly contradicts this view (Organon, Dudgeon’s translation see also here, page 239 ). The emphasis is mine.
| “I must say that these procedures seem to show chiefly how high one can go with the potentized attenuation of medicines without their action on the human health becoming nil.“ |
Although this claims that you can dilute a lot, it also admits that if the dilution goes too far the effect would eventually vanish, contrary to the usual homeopathic “principle” that it should keep getting stronger and stronger. and contrary to Hahnemann’s suggestions in other places that he thought matter was infinitely divisible.
This passage shows quite clearly that Hahnemann did not believe that his medicines would work if they were diluted so much that that there were no molecules left. That he believed this is confirmed by a letter that Hahnemann wrote in a letter to a Dr Schreter dated September 13th, 1829. This letter reprimanded Schreter for advocating extremely high dilutions.
| “there must be some limit to the thing. It cannot go on to infinity” The original German version was “Es muss ein Ende geben, es kann nicht bis ins Unendliche weitergehen” |
This confirms that Hahnemann was aware of, and accepted, that matter was not infinitely divisible and his medicines would not work if they contained nothing of the original material.
This attitude is actually not at all surprising, because Hahnemann was an educated man and he had a particular interest in chemistry. He cannot have failed to be aware of Dalton’s atomic theory, which was published between 1805 – 1810, while Hahnemann was writing the first edition of the Organon.
Peter Morrell, in Hahnemann and Homeopathy, says
“These were obviously developments that Hahnemann could not have failed to know about and indeed, was thoroughly excited about, It is clear from many of his asides that he regarded chemistry as the most important science.”
What is astonishing is that I can find no example of Hahnemann ever having mentioned Dalton or Avogadro. Perhaps he was a bit scared by the implications of their suggestions that molecules could not be divided without changing their nature.
The first edition of the Organon was published in 1810. but in the 5th edition appeared 1833, ten years before his death, These dates turn out to be important.
John Dalton (1776 – 1844) was able to estimate relative atomic masses of various molecules, the smallest unit that a chemical can exist in without losing irs identity. His values were soon improved by Amadeo
Avogadro (1776 – 1856), in 1811. Avogadro made the very important proposal that the volume of a gas (strictly, of an ideal gas ) is proportional to the number of atoms or molecules that are present. More precisely, the relationship between the masses of the same volume of different gases (at the same temperature and pressure) corresponds to the relationship between their respective molecular weights. Hence, the relative molecular mass of a gas can be calculated from the mass of a sample of known volume.
BUT neither Avogadro nor Dalton knew how many molecules there were in a given mass of a substance
This is absolutely crucial because it means that, although Hahnemann realised that there was a limit to the dilutions that could be used, he had no way of knowing what that limit was,

The answer to that question was discovered only in 1865, 22 years after the death of Hahnemann. It was discovered not by Avogadro, but by Johann Josef Loschmidt (1821 – 1895). It is Loschmidt, not Avogadro, who discovered the crucial numerical value of ‘Avogadro’s number‘, and in the German literature it is known, properly, as Loschmidt’sche Zahl.
This number is 6.022 x 1023 molecules per mole. One mole of a pure compound is its molecular mass in grams. The molecular mass of carbon (relative to hydrogen) is 12, so 12 grams of carbon contain 6.022 x 1023 carbon atoms. The molecular mass of of strychnine is 334.4 so 334.4 grams of strychnine contain 6.022 x 1023 strychnine molecules.
Armed with the numerical value of Avogadro’s number, it is easy to calculate that a 30 C homeopathic dilution contains nothing whatsoever. More precisely, it would contain, on average, a single molecule in spherical pill with a diameter equal to the distance from the earth to the sun.
But Hahnemann could not have known that. If had lived another 25 years he would almost certainly have renounced the idea of using 30 C dilutions.
He had a good excuse for getting it wrong. He was dead before the knowledge existed to do the calculation
But modern homeopaths have no excuse whatsoever for believing the impossible.
Hahnemann would have thought they were nuts, I suspect. He was too intelligent to believe that medicines that contain no medicine could be effective. In his words, “It cannot go on to infinity”.
Acknowledgement
I very grateful to ‘ Lindy’ for help in checking the references that are cited here, and for helpful discussions.
This, I fear, is pure plagiarism, Robert Shrimsley’s piece in today’s Financial Times was so funny that it just begged to be quoted. Here it is.
|
Surely this is a call to action. The news that Radovan Karadzic has been hiding out as some kind of homeopath has confirmed all prejudices about alternative medicine. I have had my doubts about this vicious breed ever since we were gulled into giving the kids valerian and hops to calm them down on an overnight flight and they went absolutely wild. Talk about a crime against humanity. Incidentally old Rad is not exactly an advert for homeopathy if this week’s photographs are anything to go by. Before he got into all this complementary healing, he was a sprightly, globally-feared warlord and international criminal. Now, after a decade of mixing his own marjoram, he is a strangely bearded hippy, blathering on about the need to nurture your inner self. Of course with hindsight health shops of the world were an obvious hiding place for genocidal maniacs. Remember all that talk of cleansing impurities? Well, I think we now know what that was all about. Some of you may be thinking that Karadzic was an aberration in an otherwise harmless community. But I ask you, how likely is it that the butcher of Belgrade could have kept up the pretence for so long without ever giving himself away. Were no suspicions aroused by the publication of his first book Radovan’s Remedies . Did no one notice that his patented treatment for stress prescribed ground echinacea root, essence of basil and the blood of a thousand Bosnians. Anyway, now that these collected homeopaths, herbologists and healers have finally been exposed as nothing more than a front organisation for the world’s most wanted, we will doubtless see swift action. How long can it be until the National Security Agency, operating undercover in Greenwich Village, finally pinpoints the precise location of Osama bin Laden’s reiki parlour? Crack teams of CIA operatives will surely be rounding up reflexologists in their search for Ratko Mladic. We can be confident that even now special rendition flights, crammed full of ayurvedic surgeons are en route to Guantánamo, where skilled interrogators will rearrange their chakras at no extra charge. Homeopaths will be forced to take two Disprins every four hours until they crack. US authorities have, however, pledged not to use the cruel practice of water-boarding – except perhaps on hydrotherapists. Of course we may snare a few, genuinely innocent aromatherapists on the way but as they say in the trade, you can’t make a poultice without grinding some ginger. |
During the last year, there has been a very welcome flurry of good and informative books about alternative medicine. They are all written in a style that requires little scientific background, even the one that is intended for medical students.
CAM, Cumming | Trick or Treatment | Snake Oil Science |
Testing treatments | Suckers | Healing, Hype or Harm
I’ll start with the bad one, which has not been mentioned on this blog before.
Complementary and Alternative medicine. An illustrated text.
by Allan D. Cumming, Karen R. Simpson and David Brown (and 12 others). 94 pages, Churchill Livingstone; 1 edition (8 Dec 2006).
| The authors of this book sound impressive
Allan Cumming, BSc(Hons), MBChB, MD, FRCP(E), Professor of Medical Education and Director of Undergraduate Learning and Teaching, and Honorary Consultant Physician, College of Medicine and Veterinary Medicine, University of Edinburgh, Edinburgh, UK; Karen Simpson, BA(Hons), RN, RNT, Fellow in Medical Education, College of Medicine and Veterinary Medicine David Brown, MBChB, DRCOG, General Practitioner, The Murrayfield Medical Centre, and Honorary Clinical Tutor, University of Edinburgh |
 |
Sadly, this is a book so utterly stifled by political correctness that it ends up saying nothing useful at all. The slim volume is, I have to say, quite remarkably devoid of useful information. Partly that is a result of out-of-date and selective references (specially in the chapters written by alternative practitioners),
But the lack of information goes beyond the usual distortions and wishful thinking. I get the strong impression is that it results not so much for a strong commitment to alternative medicine (at least by Cumming) as from the fact that the first two authors are involved with medical education. It seems that they belong to that singularly barmy fringe of educationalists who hold that the teacher must not give information to s student for fear of imparting bias. Rather the student must be told how to find out the information themselves. There is just one little problem with this view. It would take about 200 years to graduate in medicine.
There is something that worries me about medical education specialists. Just look at the welcome given by Yale’s Dean of Medical Education, Richard Belitsky, to Yale’s own division of “fluid concepts of evidence”, as described at Integrative baloney @ Yale, and as featured on YouTube. There are a lot of cryptic allusions to alternative forms of evidence in Cumming’s book too, but nothing in enough detail to be useful to the reader.
What should a book about Alternative medicine tell you? My list would look something like this.
- Why people are so keen to deceive themselves about the efficacy of a treatment
- Why it is that are so often deceived into thinking that something works when it doesn’t
- How to tell whether a medicine works better than placebo or not,
- Summaries of the evidence concerning the efficacy and safety of the main types of alternative treatments.
The Cumming book contains chapters with titles like these. It asks most of the right questions, but fails to answer any of them. There is, time and time again, the usual pious talk about the importance of evidence, but then very little attempt to tell you what the evidence says. When an attempt is made to mention evidence, it is usually partial and out of date. Nowhere are you told clearly about the hazards that will be encountered when trying to find out whether a treatment works.
| The usual silly reflexology diagram is reproduced in Cumming’s introductory chapter, but with no comment at all, The fact that it is obviously total baloney is carefully hidden from the reader.. What is the poor medical student meant to think when they perceive that it is totally incompatible with all the physiology they have learned? No guidance is offered. | 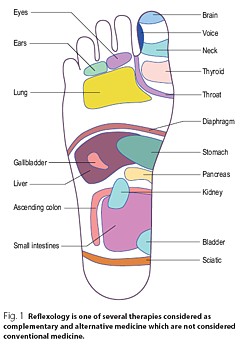 |
| You will look in vain for a decent account of how to do a good randomised controlled trial, though you do get a rather puerile cartoon, The chapter about evidence is written by a librarian. Since the question of evidence is crucial, this is a fatal omission. |  |
Despite the lack of presentation of evidence that any of it works, there seems to be an assumption throughout the book that is is desirable to integrate alternative medicine into clinical practice. In Cumming’s chapter (page 6) we see
Since it would not be in the interests of patients to integrate treatments that don’t work with treatments that do work, I see only two ways to explain this attitude. Either the authors have assumed than most alternative methods work (in which case they haven’t read the evidence), or they think integration is a good idea even if the treatment doesn’t work. Neither case strikes me as good medical education.
The early chapters are merely vague and uninformative. Some of the later chapters are simply a disgrace.
Most obviously the chapter on homeopathy is highly selective and inaccurate, That is hardly surprising because it is was written by Thomas Whitmarsh, a consultant physician at Glasgow Homeopathic Hospital (one that has still survived). It has all the usual religious zeal of the homeopath. I honestly don’t know whether people like Whitmarsh are incapable of understanding what constitutes evidence, or are simply too blinded by faith to even try. Since the only other possibility is that they are dishonest, I suppose it must be one of the former.
The chapter on “Nutritional therapy” is also written by a convert and is equally misleading piece of special pleading.
The same is true of the chapter on Prayer and Faith Healing. This chapter reproduces the header of the Cochrane Review on “Intercessory prayer for the alleviation of Ill Health”, but then proceeds to ignore entirely its conclusion “Most of the studies show no real differences”).
If you want to know about alternative medicine, don’t buy this book. Although this book was written for medical students, you will learn a great deal more from any of the following books, all of which were written for the general public.
Trick or Treatment
by Simon Singh and Edzard Ernst, Bantam Press, 2008
| Simon Singh is the author of many well-known science books, like Fermat’s Last Theorem. Edzard Ernst is the UK’s first professor of complementary and alternative medicine.
Ernst, unlike Cumming et. al is a real expert in alternative medicine. He practised it at an early stage in his career and has now devoted all his efforts to careful, fair and honest assessment of the evidence. That is what this book is about. It is a very good account of the subject and it should be read by everyone, and certainly by every medical student. |
 |
Singh and Ernst follow the sensible pattern laid out above, The first chapter goes in detail into how you distinguish truth from fiction (a little detail often forgotten in this area).
The authors argue, very convincingly, that the development of medicine during the 19th and 20th century depended very clearly on the acceptance of evidence not anecdote. There is a fascinating history of clinical trials, from James Lind (lemons and scurvy), John Snow and the Broad Street pump, Florence Nightingale’s contribution not just to hygiene, but also to the statistical analysis that was needed to demonstrate the strength of her conclusions (she became the first female member of the Royal Statistical Society, and had studied under Cayley and Sylvester, pioneers of matrix algebra).
There are detailed assessments of the evidence for acupuncture, homeopathy, chiropractic and herbalism, and shorter synopses for dozens of others. The assessments are fair, even generous in marginal cases.
Acupunture. Like the other good books (but not Cumming’s), it is pointed out that acupuncture in the West is not so much the product of ancient wisdom (which is usually wrong anyway), but rather a product of Chinese nationalist propaganda engineered by Mao Tse-tung after 1949. It spread to the West after Nixon’s visit Their fabricated demonstrations of open heart surgery under acupuncture have been known since the 70s but quite recently they managed again to deceive the BBC It was Singh who revealed the deception. The conclusion is ” . . . this chapter demonstrates that acupuncture is very likely to be acting as nothing more than a placebo . . . ”
Homeopathy. “hundreds of trials have failed to deliver significant or convincing evidence to support the use of homeopathy for the treatment of any particular ailment. On the contrary, it would be to say that there is a mountain of evidence to suggest that homeopathic remedies simply do not work”.
Chiropractic. Like the other good books (but not Cumming’s) there is a good account of the origins of chiropractic (see, especially, Suckers). D.D. Palmer, grocer, spiritual healer, magnetic therapist and fairground quack, finally found a way to get rich by removing entirely imaginary ‘subluxations’. They point out the dangers of chiropractic (the subject of court action), and they point out that physiotherapy is just as effective and safer.
Herbalism. There is a useful table that summarises the evidence. They conclude that a few work and most don’t Unlike homeopathy, there is nothing absurd about herbalism, but the evidence that most of them do any good is very thin indeed.
| “We argue that it is now the time for the tricks to stop, and for the real treatments to take priority. In the name of honesty, progress and good healthcare, we call for scientific standards, evaluation and regulation to be applied to all types of medicine, so that patients can be confident that they are receiving treatments that demonstrably generate more harm than good.” |
Snake Oil Science, The Truth about Complementary and Alternative Medicine.
R. Barker Bausell, Oxford University Press, 2007
Another wonderful book from someone who has been involved himself in acupuncture research, Bausell is a statistician and experimental designer who was Research Director of a Complementary and Alternative Medicine Specialised Research Center at the University of Maryland.
This book gives a superb account of how you find out the truth about medicines, and of how easy it is to be deceived about their efficacy.
I can’t do better than quote the review by Robert Park of the American Physical Society (his own book, Voodoo Science, is also excellent)
| “Hang up your lantern, Diogenes, an honest man has been found. Barker Bausell, a biostatistician, has stepped out of the shadows to give us an insider’s look at how clinical evidence is manipulated to package and market the placebo effect. Labeled as ‘Complementary and Alternative Medicine’, the placebo effect is being sold, not just to a gullible public, but to an increasing number of health professionals as well. Bausell knows every trick and explains each one in clear language” |  |
Bausell’s conclusion is stronger than that of Singh and Ernst.
“There is no compelling, credible scientific evidence to suggest that any CAM therapy benefits any medical condition or reduces any medical symptom (pain or otherwise) better than a placebo”.
Here are two quotations from Bausell that I love.
[Page 22] ” seriously doubt, however, that there is a traditional Chinese medicine practitioner anywhere who ever stopped performing acupuncture on an afflicted body in the presence of similarly definitive negative evidence. CAM therapists simply do not value (and most cases, in my experience, do not understand) the scientific process”
And even better,
[Page39] “But why should nonscientists care one iota about something as esoteric as causal inference? I believe that the answer to this question is because the making of causal inferences is part of our job description as Homo Sapiens.”
Testing Treatments: Better Research for Better Healthcare
by Imogen Evans, Hazel Thornton, Iain Chalmers, British Library, 15 May 2006
You don’t even need to pay for this excellent book (but buy it anyway, eg from Amazon). If you can’t afford, £15 then download it from the James Lind Library.
| This book is a unlike all the others, because it is barely mentions alternative medicine. What it does, and does very well, is to describe he harm that can be done to patients when they are treated on the basis of guesswork or ideology, rather than on the basis of proper tests. This, of course, is true whether or not the treatment is labelled ‘alternative’.
It is worth noting that one of the authors of this book is someone who has devoted much of his life to the honest assessement of evidence, Sir Iain Chalmers, one of the founders of the Cochrane Collaboration , and Editor of the James Lind Library . |
 |
A central theme is that randomised double blind trial are essentially the only way to be sure you have the right answer. One of the examples that the authors use to illustrate this is Hormone Replacement Therapy (HRT). For over 20 years, women were told that HRT would reduce their risk of heart attacks and strokes. But when, eventually, proper randomised trials were done, it was found that precisely the opposite was true. The lives of many women were cut short because the RCT had not been done,
The reason why the observational studies gave the wrong answer is pretty obvious. HRT was used predominantly by the wealthier and better-educated women. Income is just about the best predictor of longevity. The samples were biassed, and when a proper RCT was done it was revealed that the people who used HRT voluntarily lived longer despite the HRT, not because of it. It is worth remembering that there are very few RCTs that test the effects of diet. And diet differs a lot between rich and poor people. That, no doubt, is why there are so many conflicting recommendations about diet. And that is why “nutritional therapy” is little more than quackery. Sadly, the media just love crap epidemiology. One of the best discussions of this topics was in Radio 4 Programme. “The Rise of the Lifestyle Nutritionists“, by Ben Goldacre.
One of the big problems in all assessment is the influence of money, in other words corruption, The alternative industry is entirely corrupt of course, but the pharmaceutical industry has been increasingly bad. Testing Treatments reproduces this trenchant comment.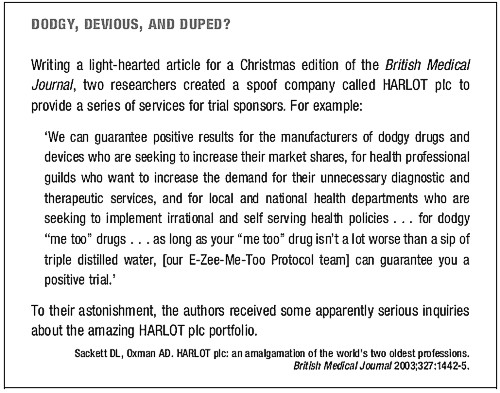
Suckers. How Alternative Medicine Makes Fools of Us All
Rose Shapiro, Random House, London 2008
| I love this book. It is well-researched, feisty and a thoroughly good read.
It was put well in the review by George Monbiot.
The chapters on osteopathy and chiropractic are particularly fascinating. |
 |
This passage describes the founder of the chiropractic religion.
“By the 1890s Palmer had established a magnetic healing practice in Davenport, Iowa, and was styling himself ‘doctor’. Not everyone was convinced as a piece about him in an 1894 edition of the local paper, the Davenport Leader, shows.”
A crank on magnetism has a crazy notion hat he can cure the sick and crippled with his magnetic hands. His victims are the eak-minded, ignorant and superstitious, those foolish people who have been sick for years and have become tired of the regular physician and want health by the short-cut method . . . he has certainly profited by the ignorance of his victims . . . His increase in business shows what can be done in Davenport, even by a quack”
Over 100 years later, it seems that the “weak-minded, ignorant and superstitious” include the UK’s Department of Health, who have given these quacks a similar status to the General Medical Council.
The intellectual standards of a 19th Century mid-western provincial newspaper leader writer are rather better than the intellectual standards of the Department of Health, and of several university vice-chancellors in 2007.
Healing Hype or Harm
Edited by Imprint Academic (1 Jun 2008)
Download the contents page
My own chapter in this compilation of essays, “Alternative medicine in UK Universities” is an extended version of what was published in Nature last year (I don’t use the term CAM because I don’t believe anything can be labelled ‘complementary’ until it has been shown to work). Download a copy if the corrected proof of this chapter (pdf).
| Perhaps the best two chapters, though, are “CAM and Politics” by Rose and Ernst, and “CAM in Court” by John Garrow.
CAM and politics gives us some horrifiying examples of the total ignorance of almost all politicians and civil servants about the scientific method (and their refusal to listen to anyone who does understand it). CAM in Court has some fascinating examples of prosecutions for defrauding the public. Recent changes in the law mean we may be seeing a lot more of these soon. Rational argument doesn’t work well very well with irrational people. But a few homeopaths in jail for killing people with malaria would probably be rather effective. |
 |
Follow-up
Healing, Hype or Harm has had some nice reviews, That isn’t so surprising from the excellent Harriet Hall at Science-Based Medicine. The introduction to my chapter was a fable about the replacemment of the Department of Physics and Astronomy by the new Department of Alternative Physics and Astrology. It was an unashamedly based on Laurie Taylor’e University of Poppleton column. Hall refers to it as “Crislip-style”, a new term to me. I guess the incomparable Laurie Taylor is not well-known in the USA, Luckily Hall gives a link to Mark Crislip’s lovely article, Alternative Flight,
“Americans want choice. Americans are increasingly using alternative aviation. A recent government study suggests that 75% of Americans have attempted some form of alternative flight, which includes everything from ultralights to falling, tripping and use of bungee cords.”
“Current airplane design is based upon a white male Western European model of what powered flight should look like. Long metal tubes with wings are a phallic design that insults the sensibilities of women, who have an alternative, more natural, emotional, way of understanding airplane design. In the one size fits all design of allopathic airlines, alternative designs are ignored and airplane design utilizing the ideas and esthetics of indigenous peoples and ancient flying traditions are derided as primitive and unscientific, despite centuries of successful use.”
Metapsychology Online Reviews doesn’t sound like a promising title for a good review of Healing, Hype or Harm, but in fact their review by Kevin Purday is very sympathetic. I like the ending.
“One may not agree with everything that is written in this book but it is wonderful that academic honesty is still alive and well.”


