badscience
The bulletin of the British Pharmacological Society, Pharmacology Matters, declined to publish the following article. Sadly the Society seems to be more interested in "reputation management" than in truth. Luckily, it is not easy to suppress criticism these days. A version of the article has appeared in Research Fortnight where it will be seen by far more people than it would have been in Pharmacology Matters. This is the original version that I submitted to them. They would not allow me to quote Lewis’s comment (apropos of the sale of homeopathic meningitis vaccine)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
If a child were to die of whooping cough or meningitis as a result of buying the fraudulent "vaccines", that would be true. It’s a sad reflection on the state of defamation law that journals are not willing to say so. Blogs are fast becoming the best source of reliable information.

|

|
Stop press. The BPS has now signed up to Alltrials (too late for the printed version)
Pharmacology society does little to defend its subject
David Colquhoun
Over the past few years a courageous group of writers, researchers and activists has worked to expose the truth about the medicines we are sold, be they conventional or alternative.
Thanks, above all, to Ben Goldacre (1), more people than ever know that the big pharma companies have been concealing evidence of the harm that their products do, or the good they fail to do. Thanks to a small army of bloggers the preposterous claims made by peddlers of homeopathic remedies and other quackery are less likely to go unchallenged.
And yet, the organization charged with safeguarding the good name of pharmacology in this country, the British Pharmacological Society (BPS), has remained silent throughout.
The pharmaceutical industry
The BPS, rather than helping, became actively complicit when, along with much of the medical establishment, it signed an agreement with the ABPI (2). This document, developed under the aegis of the Ethical Standards in Health & Life Sciences Group (ESHLSG), contained two objectionable clauses:
“Industry plays a valid and important role in the provision of medical education”
And
“Medical representatives can be a useful resource for healthcare professionals”
Given that clinical “education” has long been part of Pharma’s marketing strategy, this seems disgraceful. And most of the doctors I know and respect refuse to see reps altogether. It is hopelessly optimistic to think that can an industry person can teach clinical pharmacology without bias in favour of his own company’s products. The BPS has many members who teach pharmacology. Can they really cope so badly that we need to have industry to educate clinicians?
It’s fine, and sometimes desirable, for academics and industry to work together on drug development. But only as long as the industry partner has no say in how, or whether, the results are published. Without that proviso we can expect more corruption of the sort that’s been seen at the University of Sheffield (3).
This is very sad, because I have great reason to like the drug industry. I’ve benefitted from several of their products myself. But the industry is in trouble. Many of its products provide only marginal benefits. Furthermore, some of the things that seemed to be useful, like SSRI antidepressants, have turned out to be next to useless once hidden trials were revealed (4). The MHRA’s learning module on SSRIs doesn’t seem to have caught up with this yet.
Sadly, the reaction of industry has been to resort to dishonesty, to hide unfavourable data and to increase yet more what it spends on marketing. Between 2009 and 2012, fines of at least 10 billion dollars (5) have been imposed on some of the most eminent companies. They include Lilly, Pfizer, AstraZeneca, Merck, Abbott and GlaxoSmithKline (GSK). The biggest fine of all ($3 bn, in July 2012) went to a British company, GSK. This succession of large fines seems to be regarded by the companies as mere marketing expenses.
All these fines were levied in the USA. Where, one might ask, are the regulators in the UK? Why have there been no fines here? Why, indeed, are some of the senior managers of these companies not in jail? Why has the BPS remained silent about the prostitution of its subject? And why have the MHRA done so little to stop it?
I suggest that you support the petition for release of the results of all trials (6). It’s been supported by many individuals and a lot of organisations, including the BMJ and the Royal Statistical Society. But, disgracefully, not by the BPS.
Quackery
At least in the case of the pharmaceutical industry some of its products work. But pharmacologists should also be concerned about the quackery industry, worth about 60 billion dollars per year (as opposed to $600 bn for the pharmaceutical industry). Virtually none of their products work (7). Why has the BPS said so little about it? It has, along with most of the medical and university establishment, shrugged its shoulders about the fact that students at Westminster University have been shown dowsing with a pendulum as a method for selection of herbal “remedies”, as part of a Bachelor or “Science” degree. It is an area in which every regulatory agency has failed to ensure even minimal levels of honesty (8). And the BPS has just shrugged.
The MHRA has been worse than useless in this area: it has been actively unhelpful (9). The senior staff of the MHRA are members of the BPS which has, as usual, said next to nothing. The MHRA’s herbal medicine committee has allowed misleading labels that give indications to be put on herbal potions, and these labels fail to make it clear that no evidence whatsoever of efficacy is required to get the MHRA kitemark. The wording was suggested (not required) by European law, but that law does not prevent the MHRA from saying, as it should, “there is no reason to think that this product is effective for any of the indications on the label” (10). Arguably, the MHRA is in breach of Consumer Protection law (11, 12).
At the time, the BPS did make some objection to the labelling (13), but only under great pressure from me (indeed I wrote it) . That has not been followed up, and I can no longer find it on the BPS web site. Indeed Philip Routledge, one of the people who is responsible for the misinformation in his capacity as chair of the MHRA Herbal Medicines Advisory Committee, is, at present the president of the BPS.
The MHRA has also been responsible for misleading labelling of the products of the most obviously fraudulent products of the lot: homeopathic pills, the medicines that contain no medicine. Most of the pills (anything beyond 12x dilution) contain not a single molecule of the substance on the label. Yet they have been given a get-out clause that enables them to evade prosecution by Trading Standards (an organisation that consistently fails to apply consumer protection laws. Rose et al (2011) (12) concluded
"EU directive 200s5/29/EC is largely ineffective in preventing misleading health claims for consumer products in the UK".
It is simply bizarre that the people at the MHRA, many of who are BPS members, have sat round a table and approved the following label. This example is for Arnica 30C pills, which, of course, contain no trace of arnica (14, 8). The outcome of their deliberations is simply surreal (see the actual labels here).
"Used within the homeopathic tradition for the symptomatic relief of sprains, muscular ache; and bruising or swelling after contusions."
This will deceive the naïve into thinking that it will have some effect on sprains etc. It won’t. And the MHRA have declined to test how the label is perceived by the public, though it took some effort to get them to admit it.
"If you are allergic to any of the ingredients in this medicine, consult your doctor before taking this medicine."
The ingredients aren’t stated apart from “contains lactose and sucrose”. That’s all they contain. No arnica.
"If pregnant or breastfeeding consult your doctor before use."
Why should a few mg of lactose and sucrose have the slightest effect on a pregnant or breast-feeding mother. This is pure make-believe
"If you forget to take this product, continue to take your usual dose at the usual time, it does not matter if you have missed a dose. Do not take a double dose to make up for a missed dose."
This statement is even more bizarre. There is nothing in the pills.
"If you take too much of this product (overdose) speak to a doctor or pharmacist and take this label with you."
And this is the ultimate in nonsense. The 1023 campaign regularly swallows whole bottles, and of course nothing happens. You can’t overdose on nothing. The fact that the MHRA can insist on this label, with a straight face, is the ultimate betrayal of science and reason.
"When asked to comment, as part of the consultation on these rules, this was the response from the BPS."

This is extracted from page 16 of the “selected response” provided by the MHRA under a Freedom of Information Act request [download all]
Things have changed little since A.J. Clark wrote his book on Patent Medicines in 1938 (15). And the BPS has done next to nothing to help. Neither has the MHRA. In fact both have colluded in the failures of both honesty and reason.
A BBC South West program recently revealed that a pharmacist was selling “homeopathic vaccines” for whooping cough and meningitis (16). The MHRA have know about his homicidal practice for years, but have done nothing. The General Pharmaceutical Council let him off with a rap on the knuckles. It has been left to bloggers and TV reporters to focus attention on these scoundrels. The well-respected blogger, Andy Lewis, wrote (17)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
And the full clinical data for Tamiflu are still being concealed by Roche (18).
I think that is rather shameful.
I have been a member of the BPS for all my working life. I was happy when they made me an honorary fellow. But I now find myself asking if I can remain a member of an organisation that has done so little to defend honest scientific behaviour.
References
(1) Ben Goldacre’s Bad Pharma. Buy it now. Then do something. https://www.dcscience.net/?p=5538
(2) ABPI 2012 Guidance on collaboration between healthcare professionals and the pharmaceutical industry. http://www.abpi.org.uk/our-work/library/guidelines/Pages/collaboration-guidance.aspx
(3) Colquhoun, D. (2007) The Corporate Corruption of Higher Education: part 2 https://www.dcscience.net/?p=193
(4) Kirsch,I., B.J.Deacon, T.B.Huedo-Medina, A.Scoboria, T.J.Moore, and B.T.Johnson. 2008. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS. Med. 5:e45. http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0050045
(5) Groeger, L. (2012) Big Pharma’s Big Fines http://www.propublica.org/special/big-pharmas-big-fines
(6) All trials registered. All results reported, http://www.alltrials.net/supporters/
(7) Singh,S. and E.Ernst. 2009. Trick or Treatment. Corgi. http://en.wikipedia.org/wiki/Trick_or_Treatment
(8) Colquhoun, D. (2012) Regulation of alternative medicine: why it doesn’t work, and never can. https://www.dcscience.net/?p=5562
(9) Colquhoun, D, (2006) The MHRA breaks its founding principle: it is an intellectual disgrace. https://www.dcscience.net/?p=32
(10) Colquhoun, D. (2011). Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. https://www.dcscience.net/?p=4269
(11) Colquhoun, D. (2009) Most alternative medicine is illegal. https://www.dcscience.net/?p=30
(12) Rose,L.B., P.Posadzki, and E.Ernst. 2012. Spurious claims for health-care products: an experimental approach to evaluating current UK legislation and its implementation. Med. Leg. J. 80:13-18. https://www.dcscience.net/Rose-medico-legal-2012.pdf
(13) Colquhoun, D. (2006) Learned Societies speak out against CAM, and the MHRA. https://www.dcscience.net/?p=30
(14) MHRA Arnicare Arnica 30c pillules NR 01175/0181 http://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con049307.pdf
(15) Colquhoun, D. (2008) Patent medicines in 1938 and now: A.J.Clark’s book. https://www.dcscience.net/?p=257
(16) BBC South West on the evils of homeopathic "vaccines" http://www.youtube.com/watch?v=TZf9mUzI4RI
(17) Why Does the MHRA Not Close Down these Homeopaths? The regulators have known of serious problems for years, Nothing is done. http://www.quackometer.net/blog/2013/01/why-does-the-mhra-not-close-down-these-homeopaths.html
(18) Payne, D. (2012). Tamiflu: the battle for secret drug data http://www.bmj.com/content/345/bmj.e7303
Follow-up
25 February 2013 This post has some follow-up even before it appeared on Research Research. I noticed on the BPS web site a press release “BPS announces intention to sign All Trials Petition“. It was dated 20th February, but I didn’t notice it until after the printed edition went to press. It was expressed as a future intention to sign, though in fact they signed almost straight away (though over 100 organisations had already done so). That’s good. I suspect that when my old friend, Humphrey Rang, who is president elect of the BPS, takes charge, the Society may start to take its responsibilities to the public more seriously than it has in the past.
|
The MHRA, on the other hand, is still evading its self-declared job of ensuring the public that drugs work. |

|
13 March 2013. A reply to this piece appeared in red on Research Research, The British Pharmacological Society champions its science. It was written by Humphrey Rang who, as president elect of the BPS naturally felt obliged to defend its record. He defends the BPS membership of ESHLSG, but fails to mention that first the Lancet and then the BMA withdrew their support. Nor does he mention that medical students and doctors launched a campaign, BadGuidelines.org, against the agreement. The Medical Schools Council, which also signed the agreement, said "the scrutiny of the guidance has ‘identified deficiencies in the current statement". Didn’t they read it before signing? Rang says that the BPS is also working to improve the joint statement with the ABPI. That’s good, but one must wonder why the BPS signed up to the original form.
On the points about quackery, Rang sites the BPS statement on homeopathy (now vanished) but fails to mention that that statement was written by me in an attempt to wake the BPS from it’s slumbers on the matter of medicines that don’t work. But he doesn’t mention at all the matter of mislabelling of both homeopathic and herbal preparations.
Of course, the BPS does many good things. But like most organisations, it is too reluctant to speak out when it sees wrongdoing, and too reluctant to say "sorry we made a cock-up that time".
|
“In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established”. . . “. . . they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.” David Mattin, lately of NHS Choices |
NHS Choices is usually a good source of information for the public. But there is one exception: the information they provide about alternative medicine is poor. A Freedom of Information Act request has revealed that the attempt of NHS Choices to rewrite their pages more accurately was censored by the Department of Health in conjunction with the late Prince’s Foundation for Integrated Health. The Department of Health (DH) has misled the public.
The earliest version of the homeopathy information page recorded by the Wayback Machine was November 12 2007. It was still there on December 5 2010. The comments were mostly critical. One said, quite correctly,
|
I find it most regrettable that the way NHS has covered this subject is to give uncritical voice to the claims of homoeopathy without giving readers the information they need to evaluate those claims. To refer readers to the websites of the British Homeopathy Association is like settling the question of the shape of planet by a reference to the website of the Flat Earth Society |
There were a lot of complaints, and to the credit of NHS Choices, the page vanished. Throughout 2011, and up to October 2012 the information page on homeopathy read
|
Introduction Content on homeopathy has been removed from the website pending a review by the Department of Health policy team responsible for complementary and alternative medicines. Homeopathy is not part of mainstream medicine. Instead it is defined as a complementary or alternative medicine. If you are considering using homeopathy, talk to your GP first. For more information about homeopathy see the House of Commons Science and Technology Committee report on homeopathy published on 8 February 2010 and the Department of Health response to that report published in July 2010 (PDF, 69KB). |
Then, at the end of 2012, the page reappeared. It was a bit better than the original, but not much. Many of the comments criticise the misleading nature of the information (as well as the usual “it worked for me” comments). The “useful links” still has six links to flat-earth organisations like the Society of Homeopaths, and only one to a sensible source, the excellent pamphlet from Sense about Science. They do link at the end to the 2010 Science and Technology Committee Report: Evidence Check 2: Homeopathy (PDF, 1.61Mb), and to the Government Response to the Science and Technology Committee Report, Evidence Check 2: Homeopathy (PDF, 69kb) but no comment is made on the findings.
Policy-based evidence
I wondered why the NHS Choices page, after an absence of almost two years, had returned in such an unsatisfactory form. So I asked them. After a reminder, I was told that my queries were being dealt with not by NHS Choices, but had been referred to Dr Sunjai Gupta “the DH official with responsibility for this area”. Dr Sunjai Gupta OBE is Deputy Director of Public Health Strategy and Social Marketing, Department of Health.
Dr Gupta is not obviously sympathetic to woo. It’s hard to tell since he doesn’t seem to have published much. But one is not reassured by an article that he wrote for the Journal of Holistic Healthcare. It appears straight after an article by fantasy herbalist, Simon Mills.
Despite assurances that I’d hear from Dr Gupta shortly, nothing happened. So I sent a request for the correspondence under the Freedom of Information Act (2000). Although the request was addressed to NHS Choices, a public body, strenuous efforts were made to divert it to the Department of Health. These were resisted. Nevertheless when, after a long delay, the material arrived, it came not from NHS Choices, but from DH, who had evidently vetted it,. The emails were rather shocking [download all].
A mail dated 1 December 2009 said

This is the most direct statement I’ve seen that, in the Department of Health, policy dictates evidence. NHS Choices is meant to provide evidence, but what they say has to be checked by DH to make sure they “don’t clash with any policy messages”.
The re-written page
The original version of the re-written page was sent to me by David Mattin, who worked for NHS Choices until September 2012. You can download the whole draft here. It is an enormous improvement on the original page. For example, it says
|
“Does it work?
Many independent experts would respond to this question ‘no, homeopathy does not work’ There is no good quality clinical evidence to show that homeopathy is more successful than placebo in the treatment of any type of condition. Furthermore, if the principles of homeopath were true it would violate all the existing theories of science that we make use of today; not just our theory of medicine, but also chemistry, biology and physics. |
This original draft was sent to Mattin on 29 January 2010. After editing it for length Mattin sent it to DH for approval. Over the next two years, DH removed much of the accurate content. Mattin’s own comments on this evisceration are reproduced below.
The DH emails
All the names have been redacted. Needless to say, nobody is willing to take responsibility. But the number of people who support magic medicine is really quite small so the main players were easy to identify.
During the nearly 2 year absence of the homeopathy page, dozens of changes were made by DH. It seems that the policy message with which the NHS Choices draft failed to comply were those of the Prince’s Foundation for Integrated Health, and its successor (after April 2010), the College of Integrated Health, now known as the College of Medicine.
NHS Choices sought advice about their redrafted pages from the right person, Sir Iain Chalmers, one of the founders of the Cochrane Collaboration. On 3 Nov 2009, Chalmers advised
The most reliable source in the country - and one of the most reliable in the world - is Professor Edzard Ernst, professor of Complementary Medicine at the Peninsular Medical School, |
Ernst returned his suggestions in July 2010, but it seems that few of them survived the subsequent 18 months of revisions by DH.
On 2 December 2009, a mail from the NHS headquarters (Quarry House, Leeds) was sent to NHS Choices

This makes it perfectly clear that DH regards the Prince’s Foundation, and the equally flaky Complementary and Natural Healthcare Council (CNHC: known on the web as Ofquack) as appropriate guides for public health policy. The fact of the matter is that regulation of magic medicine by the government has been a total disaster, because, it seems, DH regards the Prince of Wales as a reliable source.
On 29 December 2009, the Prince’s Foundation went on the attack.

On 10th January 2010, two more letters were sent to DH by the Prince’s Foundation. At 13.48 they wrote

And at 22.14 on the same day, it was followed up with

The references to Devon and to Thought Field Therapy, make it very obvious that these letters were written by Dr Michael Dixon OBE, who was medical director of the Prince’s Foundation, and who is now a director of the “College of Medicine”. And the object of Dixon’s bile is obviously Edzard Ernst (the quotation is from his book, Trick or Treatment).
I find it fascinating to see just how venomous quacks become when the evidence contradicts their views. The cuddly “holistic” veneer quickly vanishes.
It gets worse. On 21 January 2010, a mail from NHS Choices to DH said

The only person in the country who fits this description is the (in)famous George Lewith. It is simply mind-boggling that DH regards him as an appropriate person to advise on anything.
After that, NHS Choices kept asking DH to sign off the documents, and changes continued to be made. Almost two years later, DH were still stalling.

The admission that “We are a bit short of doctors within DH these days” is interesting.
A bit short of anyone capable of critical thinking would be more accurate.
The most interesting document that I got from DH was an intermediate draft of the rewritten page on homeopathy (undated). Download the document. Here are a couple of extracts.
It’s a story of two years of meddling and procrastination. The end result misinforms the public.
Right at the start, the NHS Choices draft says, reasonably enough
A House of Commons Science and Technology Committee report said that homeopathic remedies perform no better than placebos and that the principles on which homeopathv is based are “scientifically implausible”.
But a comment, added apparently by DH, says
Can we remove this statement? This report is really quite contentious and we may well be subject to quite a lot of challenge from the Homeopathic community if published.
What on earth? The DH seems to think that that its job is not to present the evidence, but to avoid challenges from the homeopathic community! And true enough, this piece is missing from the final version.
A bit later, the NHS Choices draft was censored again
“A 2010 Science and Technology Committee report said that scientific tests had shown that homeopathic treatments don’t work”
But again this doesn’t appear in the final version. The comment, apparently from DH, says
“The DH response to this report (point 24) doesn’t support this statement though”
That’s a gross distortion of point 24, which actually concludes
“The Government Chief Scientific Adviser cannot envisage scientifically credible proposals for funding for research into homeopathy in the future”
NHS Choices was not happy with the result
Shortly before the revised page was published, Paul Nuki, Editor in Chief of NHS Choicea, sent an email to DH.
|
Date: 7th September 2011 Time: 3:33:42 pm Hi I’ve been through the CAM articles and asked that we publish them asap as requested. For the record, we will be publishing these pieces outside of the normal editorial process. Although originally signed off by a suitably qualified clinician, the time lapse and policy changes have been so substantial as to render that null and void. We also don’t have a formal |
It doesn’t need much reading between the lines to see that he was unhappy with the result. It will be interesting to see whether the Information Standard people at the Royal Society for Public Health do anything about it.
The Department of Health has not just ignored evidence but actively opposed it.
That’s the only possible conclusion from the documents that I was sent. And it’s pretty shocking that the DH has preferred advice from the Prince’s Foundation and its handful of acolytes (in particular Michael Dixon and George Lewith) to the findings of the Science and Technology Select Committee and the views of the Chief Scientific Advisor.
In January this year, the Chief medical Officer, Dame Sally Davies, said, in a rare outburst of candour
|
‘I’m very concerned when homeopathic practitioners try to peddle this way of life to prevent malaria or other infectious disease,” she said. “I am perpetually surprised that homeopathy is available on the NHS.” Dame Sally, who is England’s most senior doctor, concluded by remarking that homeopathy “is rubbish”. |
 |
So one part of DH is working to contradict another part. the Chief Medical Officer. Perhaps Sally Davies should have a word with Dr Gupta.
This all predates the advent of Jeremy Hunt (and known defender of homeopathy) as health minister. But the sympathies of some DH people are made obvious by the presence on the DH web site of an article “Personal health budgets: A new way of accessing complementary therapies?”. This astonishing piece confirms the worst fears that quacks will see personal health budgets as a commercial opportunity to peddle their wares. The article is by Jim Rogers of Lincoln University. What his paper does not mention is Rogers’ conflict of interest. He’s a homeopath, and he has a paper in the International Journal of High Dilution Research (yes, there is a journal for every form of make-believe). You can download a reprint of this paper. It advocates more research into homeopathic provings, something that even George Lewith seems to have given up on.
It’s about time that the DH started to listen to the Chief Medical Officer. As it is, some people at DH seem to prefer the advice of the Prince’s Foundation, and to actively suppress employees who prefer evidence to anecdote.
One thing is clear. The DH is an unholy mess. Parts of it are intent on producing policy-based evidence.
Comment by David Mattin, who edited the first draft for NHS Choices
David Mattin left NHS Choices in September, 2012. He edited the new version and lived through the two years of wrangling with DH during which much of the best content was eviscerated. He sent me this statement about the affair.
|
As an editor at NHS Choices, I viewed it as my job to present evidence-based information to the public. The article we prepared on homeopathy stayed true to that central purpose: it made clear to readers that there is no good quality evidence that homeopathy is an effective treatment for any health condition, and also presented the broad scientific consensus that the supposed method of action of homeopathy is implausible.
What followed was a two year story of delay, and eventual suppression, of that article. My strong impression was of DH civil servants who lacked the courage, and, frankly, the energy to stand up to the criticism from special interest groups that they anticipated would arise because of the article; and that did indeed arise when a draft of the article and other draft content on complementary and alternative medicines fell into the hands of the Prince’s Foundation and other CAM groups.
The attitude of DH civil servants, broadly, was simply to tell us ‘we can’t say this about homeopathy, people will complain’. They seemed to have no interest in making an appraisal of the evidence on homeopathy themselves to see if what we were saying was actually true or not. We repeatedly pushed back with the message: ‘some people may very well complain, but if what we are saying about the evidence base is true – and it is – then we must simply weather those complaints, and stand by our content. Our duty is to supply our readers with the best information, not to please the homeopathy community.’ But these arguments were disregarded. The DH civil servants were almost entirely concerned with the politics of the situation – that is, the politics as they saw them – and the possibility that this article may create new work for them, and very little concerned with the evidence itself, or the presentation of this evidence to the public.
The whole episode is an insight into the way special interest groups can influence the workings of government and the public sector simply by making a lot of noise, and having a few powerful friends. In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established, and that they fund. They have sold out the NHS Choices editorial team, who work tirelessly to fulfil their remit. And, most seriously, they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.
|
Follow-up
13 February 2013 The Guardian version of this story, written by Sarah Boseley, is Prince’s charity lobbied government to water down homeopathy criticism. It’s fine as far as it goes but it doesn’t name any names. There are some good comments though.
14 February 2013. The printed Guardian gave the story full 5 column-width coverage. [download print version]
And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
On 14 February, the Guardian version was Editor’s Choice by lunchtime, and the Guardian web version already had 414 comments, mostly sensible (though this blog got far more referrals from twitter than from the Guardian)

And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
15 February 2013. The Daily Mail had very fair coverage of the story.

The Guardian closed the comments on the story when it had got 642 comments, most of them very sensible. And this page got almost 6000 hits in 24 hours. The majority of the referrals came from Twitter rather than from the Guardian, despite the direct link to the page from the Guardian.
18 February 2013. The affair featured in BMJ News [download the reprint]. The item featured prominently on the BMJ news page.


19 February 2013 Only six days of this post, the NHS Choices page has been re-written again, in a much improved form. That looks like bloggers 1, DH 0. It is baffling that it’s left to bloggers, working for nothing, to extract a bit of sense from the highly-paid civil servants at the Department of Health. But at least they listened this time, which is a lot more than happens often. Paul Nuki, who runs NHS Choices, deserves congratulations. Of course the revised page still doesn’t call a spade a spade, but it gets close at times. I like the way it starts "Homeopathy is a ‘treatment’ based". Notice the quotation marks.
Reputation management?
Incidentally, NHS Choices is outsourced to the (in)famous company, Capita. And the moderation of the comments on their site is outsourced again to Tempero, which describes itself as a "reputation management" company. Each of them creams off money meant of patient care. This discovery might explain why I and others have had comments rejected by NHS Choices several times. "Reputation management" is the antithesis of evidence. It is public relations, i.e. paid lying. That is quite wrong for a site that is meant to provide dispassionate information.
21 February 2013. Sadly a step backwards. Part of the improved page was removed. This bit.
The Chief Medical Officer, Professor Dame Sally Davies, has said there is no scientifically plausible way that homeopathy can prevent or cure diseases. She has made it clear she is particularly concerned about the use of homeopathy in developing countries as a so-called cure for malaria.
We can only speculate why this was removed, because it was true. In fact she accurately described homeopathy as "rubbish". Why she should not be quoted beats me.
Nobody could have been more surprised than I when I found myself nominated as an academic role model at UCL. I had to answer a few questions. It is not obvious to me what the object of the stunt is, but the person who asked me to do it seemed to find the answers amusing, so I’ll reproduce here what I said. I apologise for the temporary lapse into narcissism.
The final version has now been printed [download a copy]. Sadly the printed edition was “corrected” by someone who replaced “whom I asked to submit the first theoretical paper by Hawkes and me to the Royal Society” (as written below), with “paper by Hawkes and I”. Aaargh.
Your nomination – Why you were nominated as an Academic Role Model?
"David Colquhoun has made major contributions to our understanding of how ion channels (proteins which allow charged ions to pass across cell membranes) function to mediate electrical signalling in nerve and muscle cells. This work elegantly combines experimental and theoretical aspects, and resulted in David being made a Fellow of the Royal Society. David Colquhoun played a key role in resisting the notion that UCL should merge with Imperial College in 2002, by running a website opposed to the merger. He thus facilitated the continued existence of an independent UCL. He is also well-known for his principled opposition to therapies that are not based on scientific evidence, and for his blog which comments on this issue as well as on university bureaucracy and politics."
Role models’ questions
1. What is your response to being nominated?
Astounded.
We are interested in giving people a very brief ‘snapshot’ description of their career trajectory, to help a broad range of people see how you got to where you are:
2. What has your career path been?
|
My first job (in 1950s) was as an apprentice pharmacist in Timothy Whites & Taylors (Homeopathic Chemists) in Grange Road, Birkenhead. You can’t get a more humble start than that. But it got me interested in drugs, and thanks to my schoolmaster father, I got to the University of Leeds. |
 My father (1907 – 2001), in 1955 |
|
One of the courses involved some statistics, and that interested me. I think I made a semi-conscious decision that it would be sensible to be good at something that others were bad at, so I learned quite a lot of statistics and mathematics. I recall buying a Methuen’s Monograph on Determinants and Matrices in my final year, and, with the help of an Argentinian PhD student in physical chemistry (not my lecturers) I began to make sense of it. |

|
I purposely went into my final viva with it sticking out of my pocket. The examiner was Walter Perry, then professor of Pharmacology in Edinburgh (he later did a great job setting up the Open University). That’s how I came to be a PhD student in Edinburgh.
Although Perry was one of my supervisors, the only time I saw him was when he came into my lab between committee meetings for a cigarette. But he did make me an honorary lecturer so I could join the Staff Club, where I made many friends, including a young physics lecturer called Peter Higgs. The staff club exists no longer, having been destroyed in one of those acts of short-sighted academic vandalism that vice-chancellors seem so fond of.
The great university expansion in the 1960s made it easy to get a job. The most famous pharmacology department in the world was at UCL so I asked someone to introduce me to its then head, Heinz Schild, and asked him if he had a job. While interned during WW2 he had written a paper on the statistics of biological assay and wanted someone to teach it to students, so I got a job (in 1964), and have been at UCL ever since apart from 9 years. Between 1964 and 1970 I published little, but learned a great deal by writing a textbook on statistics.
That sort of statistics is now thought too difficult for undergraduates, and the famous department that attracted me was itself destroyed in another act of academic vandalism, in 2007.
I have spent my life doing things that I enjoy. Such success as I’ve had, I attribute to a liking for spending time with people cleverer than I am, and wasting time drinking coffee. I found a very clever statistician, Alan Hawkes, in the Housman Room in the late 1960s, and we began to collaborate on the theory of single ion channel analysis in a series of papers that still isn’t quite finished. He did the hard mathematics, but I knew enough about it to write it up in a more or less comprehensible form and to write computer programs to evaluate the algebra. When I got stuck, I would often ask Hyman Kestelman (co-author of the famous mathematics textbook, Massie & Kestelman) to explain, usually in what was then the Joint Staff Common Room at lunch time (it is now the Haldane room, the common room having been confiscated by unenlightened management). Before leaving for the USA in 1970, I, in league with the then professor of French, Brian Woledge, eventually got through a motion that allowed women into the Housman room.
I’d also talk as much as I could to Bernard Katz, whom I asked to submit the first theoretical paper by Hawkes and me to the Royal Society. His comments on the first draft led to the published version making a prediction about single ion channel behaviour before channels could be observed.
The next step was sheer luck. As this was going on, two young Germans, Neher & Sakmann, succeeded in observing the tiny currents that flow through single ion channel molecules, so it became possible to test the theory. In series of visits to Göttingen, Sakmann and I did experiments late into the night. Neher & Sakmann got a well-deserved Nobel Prize in 1991, and I expect I benefitted from a bit of reflected glory
The work that I have done is nothing if not basic. It doesn’t fit in with the current vogue for translational research (most of which will fail), although I would regard it as laying the basis for rational drug design. My only regret is that rational drug design has proved to be so difficult that it won’t be achieved in my lifetime (please don’t believe the hype).
We’d also like you to take a slightly more personal view:
3. What have been the highs (and the lows?) of your career so far?
The highs have been the chance to work with brilliant people and write a handful of papers that have a chance of having a lasting influence. Because I have been able to take my time on those projects there haven’t been too many lows, apart from observing the continuous loss of academic integrity caused by the intense pressure to publish or perish, and the progressive decline in collegiality in universities caused by that pressure combined with the rise in power of managerialism. Luckily the advent of blogs has allowed me to do a little about that.
I’m saddened by the fact that the innumeracy of biologists that I noticed as an undergraduate has not really improved at all (though I don’t believe it is worse). Most biologists still have difficulty with even the simplest equations. Worse still, they don’t know enough maths to communicate their problem to a mathematician, so only too often one sees collaborations with mathematicians produce useless results.
The only real failure I’ve had was when, in a fit of vanity, I applied for the chair of Pharmacology in Oxford, in 1984, and failed to get it. But in retrospect that was really a success too. I would have hated the flummery of Oxford, and as head of department (an increasingly unattractive job) I would have spent my time on pushing paper, not ion channels. In retrospect, it was a lucky escape. UCL is my sort of place (most of the time).
We would like to hear what our role models have to say about the next generation:
4. What advice would you give to people finishing off their PhD?
My career course would be almost impossible now. In fact it is very likely that I would have been fired before I got going in the present climate. There were quite long periods when I didn’t publish much. I was learning the tools of my trade, both mathematical and experimental. Now there is no time to do that. You are under pressure to publish a paper a week (for the glory of your PI and your university) and probably rarely find time to leave the lab to talk to inspiring people. If you are given any courses they’ll probably be in some inane HR nonsense, not in algebra. That is one reason we started our summer workshop, though bizarrely that has now been dropped by the graduate school in favour of Advanced Powerpoint.
The plight of recent PhDs is dire. Too many are taken on (for the benefit of the university, not of the student) and there aren’t many academic jobs. If you want to stay in academia, all I can suggest is that you get good at doing something that other people can’t do, and to resist the pressure to publish dozens of trivial papers.
Try to maintain some academic integrity despite the many pressures to do the opposite that are imposed on you by your elders (but not always betters). That may or may not be enough to get you the job that you want, but at least you’ll be able to hold your head high.
Finally, we want to give a balanced impression of our role models because many were nominated for their ability to motivate others, and to balance life and work:
5. How do you keep motivated?
Work-life balance is much talked about by HR, though they are one of the reasons why it is now almost impossible, In the past it wasn’t a great problem. I’m fascinated by the problems that I’m trying to puzzle out. I’ve had periods of a year or two when things haven’t gone well and I’ve felt as though I was a failure, but luckily they haven’t lasted too long, and they occurred in a time before some idiotic performance manager would harass you for failing to publish for a year or two. The climate of “performance management” is doing a lot to kill innovation and creativity.
6. What do you do when are not working in SLMS?
I’ve had various phases. For a while I carried on boxing (which had been compulsory at school). When I was first at UCL in 1964 I bought a 21 foot sloop (and as a consequence could barely afford to eat), and in 1970 (at Yale) I learned to fly. I had a lot of fun sailing right up to the early 1980s, when I found I could not afford a son as well as a boat. That was when running came into fashion and that could be done for the price of a pair of shoes. I did marathons and half marathons for fun (the London in 1988 was great fun). And that was supplanted by walking country trails in the early 2000s.
There is never a clear division between work and play, especially with algebra. You can continue to struggle with a derivation on a boat, or even get a new angle on it while running. That, of course, is why the transparency review is such total nonsense.
The main cause of stress has never been work for me. Stress comes mainly from the imposition of dim-witted managerialism and incompetent HR policies. And that has become progressively worse. I doubt that if I were a young academic now I’d have the time to spend the weekend sailing.
I’m not sure whether the blogging that has taken up something like half my time since my nominal retirement in 2004 counts as work or not. It certainly depends on things that I have learned in my academic work. And it’s fun to have effects in the real world after a life spent on problems that many would regard as esoteric.
If you want a hobby that costs very little, and allows you to say what you want, start a blog.
Follow-up
The Scottish Universities Medical Journal asked me to write about the regulation of alternative medicine. It’s an interesting topic and not easy to follow because of the veritable maze of more than twenty overlapping regulators and quangos which fail utterly to protect the public against health fraud. In fact they mostly promote health fraud. The paper is now published, and here is a version with embedded links (and some small updates).
We are witnessing an increasing commercialisation of medicine. It’s really taken off since the passage of the Health and Social Security Bill into law. Not only does that mean having NHS hospitals run by private companies, but it means that “any qualified provider” can bid for just about any service. The problem lies, of course, in what you consider “qualified” to mean. Any qualified homeopath or herbalist will, no doubt, be eligible. University College London Hospital advertised for a spiritual healer. The "person specification" specified a "quallfication", but only HR people think that a paper qualification means that spiritual healing is anything but a delusion.

The vocabulary of bait and switch
First, a bit of vocabulary. Alternative medicine is a term that is used for medical treatments that don’t work (or at least haven’t been shown to work). If they worked, they’d be called “medicine”. The anti-malarial, artemesinin, came originally from a Chinese herb, but once it had been purified and properly tested, it was no longer alternative. But the word alternative is not favoured by quacks. They prefer their nostrums to be described as “complementary” –it sounds more respectable. So CAM (complementary and alternative medicine became the politically-correct euphemism. Now it has gone a stage further, and the euphemism in vogue with quacks at the moment is “integrated” or “integrative” medicine. That means, very often, integrating things that don’t work with things that do. But it sounds fashionable. In reality it is designed to confuse politicians who ask for, say, integrated services for old people.
Put another way, the salespeople of quackery have become rather good at bait and switch. The wikepedia definition is as good as any.
Bait-and-switch is a form of fraud, most commonly used in retail sales but also applicable to other contexts. First, customers are “baited” by advertising for a product or service at a low price; second, the customers discover that the advertised good is not available and are “switched” to a costlier product.
As applied to the alternative medicine industry, the bait is usually in the form of some nice touchy-feely stuff which barely mentions the mystical nonsense. But when you’ve bought into it you get the whole panoply of nonsense. Steven Novella has written eloquently about the use of bait and switch in the USA to sell chiropractic, acupuncture, homeopathy and herbal medicine: "The bait is that CAM offers legitimate alternatives, the switch is that it primarily promotes treatments that don’t work or are at best untested and highly implausible.".
The "College of Medicine" provides a near-perfect example of bait and switch. It is the direct successor of the Prince of Wales’ Foundation for Integrated Health. The Prince’s Foundation was a consistent purveyor of dangerous medical myths. When it collapsed in 2010 because of a financial scandal, a company was formed called "The College for Integrated Health". A slide show, not meant for public consumption, said "The College represents a new strategy to take forward the vision of HRH Prince Charles". But it seems that too many people have now tumbled to the idea that "integrated", in this context, means barmpottery. Within less than a month, the new institution was renamed "The College of Medicine". That might be a deceptive name, but it’s a much better bait. That’s why I described the College as a fraud and delusion.
Not only did the directors, all of them quacks, devise a respectable sounding name, but they also succeeded in recruiting some respectable-sounding people to act as figureheads for the new organisation. The president of the College is Professor Sir Graham Catto, emeritus professor of medicine at the University of Aberdeen. Names like his make the bait sound even more plausible. He claims not to believe that homeopathy works, but seems quite happy to have a homeopathic pharmacist, Christine Glover, on the governing council of his college. At least half of the governing Council can safely be classified as quacks.
So the bait is clear. What about the switch? The first thing to notice is that the whole outfit is skewed towards private medicine: see The College of Medicine is in the pocket of Crapita Capita. The founder, and presumably the main provider of funds (they won’t say how much) is the huge outsourcing company, Capita. This is company known in Private Eye as Crapita. Their inefficiency is legendary. They are the folks who messed up the NHS computer system and the courts computer system. After swallowing large amounts of taxpayers’ money, they failed to deliver anything that worked. Their latest failure is the court translation service.. The president (Catto), the vice president (Harry Brunjes) and the CEO (Mark Ratnarajah) are all employees of Capita.
The second thing to notice is that their conferences and courses are a bizarre mixture of real medicine and pure quackery. Their 2012 conference had some very good speakers, but then it had a "herbal workshop" with Simon Mills (see a video) and David Peters (the man who tolerates dowsing as a way to diagnose which herb to give you). The other speaker was Dick Middleton, who represents the huge herbal company, Schwabe (I debated with him on BBC Breakfast), In fact the College’s Faculty of Self-care appears to resemble a marketing device for Schwabe.
Why regulation isn’t working, and can’t work
There are various levels of regulation. The "highest" level is the statutory regulation of osteopathy and chiropractic. The General Chiropractic Council (GCC) has exactly the same legal status as the General Medical Council (GMC). This ludicrous state of affairs arose because nobody in John Major’s government had enough scientific knowledge to realise that chiropractic, and some parts of osteopathy, are pure quackery,
The problem is that organisations like the GCC function more to promote chiropractic than to regulate them. This became very obvious when the British Chiropractic Association (BCA) decided to sue Simon Singh for defamation, after he described some of their treatments as “bogus”, “without a jot of evidence”.
In order to support Singh, several bloggers assessed the "plethora of evidence" which the BCA said could be used to justify their claims. When, 15 months later, the BCA produced its "plethora" it was shown within 24 hours that the evidence was pathetic. The demolition was summarised by lawyer, David Allen Green, in The BCA’s Worst Day.
In the wake of this, over 600 complaints were made to the GCC about unjustified claims made by chiropractors, thanks in large part to heroic work by two people, Simon Perry and Allan Henness. Simon Perry’s Fishbarrel (browser plugin) allows complaints to be made quickly and easily -try it). The majority of these complaints were rejected by the GCC, apparently on the grounds that chiropractors could not be blamed because the false claims had been endorsed by the GCC itself.
My own complaint was based on phone calls to two chiropractors, I was told such nonsense as "colic is down to, er um, faulty movement patterns in the spine". But my complaint never reached the Conduct and Competence committee because it had been judged by a preliminary investigating committee that there was no case to answer. The impression one got from this (very costly) exercise was that the GCC was there to protect chiropractors, not to protect the public.
The outcome was a disaster for chiropractors, wno emerged totally discredited. It was also a disaster for the GCC which was forced to admit that it hadn’t properly advised chiropractors about what they could and couldn’t claim. The recantation culminated in the GCC declaring, in August 2010, that the mythical "subluxation" is a "historical concept " "It is not supported by any clinical research evidence that would allow claims to be made that it is the cause of disease.". Subluxation was a product of the fevered imagination of the founder of the chiropractic cult, D.D. Palmer. It referred to an imaginary spinal lesion that he claimed to be the cause of most diseases. .Since ‘subluxation’ is the only thing that’s distinguished chiropractic from any other sort of manipulation, the admission by the GCC that it does not exist, after a century of pretending that it does, is quite an admission.
The President of the BCA himself admitted in November 2011
“The BCA sued Simon Singh personally for libel. In doing so, the BCA began one of the darkest periods in its history; one that was ultimately to cost it financially,”
As a result of all this, the deficiencies of chiropractic, and the deficiencies of its regulator were revealed, and advertisements for chiropractic are somewhat less misleading. But this change for the better was brought about entirely by the unpaid efforts of bloggers and a few journalists, and not at all by the official regulator, the GCC. which was part of the problem. not the solution. And it was certainly not helped by the organisation that is meant to regulate the GCC, the Council for Health Regulatory Excellence (CHRE) which did nothing whatsoever to stop the farce.
At the other end of the regulatory spectrum, voluntary self-regulation, is an even worse farce than the GCC. They all have grand sounding "Codes of Practice" which, in practice, the ignore totally.
The Society of Homeopaths is just a joke. When homeopaths were caught out recommending sugar pills for prevention of malaria, they did nothing (arguably such homicidal advice deserves a jail sentence).
The Complementary and Natural Healthcare Council (CNHC) is widely know in the blogosphere as Ofquack. I know about them from the inside, having been a member of their Conduct and Competence Committee, It was set up with the help of a £900,000 grant from the Department of Health to the Prince of Wales, to oversee voluntary self-regulation. It fails utterly to do anything useful.. The CNHC code of practice, paragraph 15 , states
“Any advertising you undertake in relation to your professional activities must be accurate. Advertisements must not be misleading, false, unfair or exaggerated”.
When Simon Perry made a complaint to the CNHC about claims being made by a CNHC-registered reflexologist, the Investigating Committee upheld all 15 complaints. But it then went on to say that there was no case to answer because the unjustified claims were what the person had been taught, and were made in good faith.
This is precisely the ludicrous situation which will occur again and again if reflexologists (and many other alternative therapies) are “accredited”. The CNHC said, correctly, that the reflexologist had been taught things that were not true, but then did nothing whatsoever about it apart from toning down the advertisements a bit. They still register reflexologists who make outrageously false claims.
Once again we see that no sensible regulation is possible for subjects that are pure make-believe.
The first two examples deal (or rather, fail to deal) with regulation of outright quackery. But there are dozens of other quangos that sound a lot more respectable.
European Food Standards Agency (EFSA). One of the common scams is to have have your favourite quack treatment classified as a food not as a medicine. The laws about what you can claim have been a lot laxer for foods. But the EFSA has done a pretty good job in stopping unjustified claims for health benefits from foods. Dozens of claims made by makers of probiotics have been banned. The food industry, needless to say, objects very strongly to be being forced to tell the truth. In my view, the ESFA has not gone far enough. They recently issued a directive about claims that could legally be made. Some of these betray the previously high standards of the EFSA. For example you are allowed to say that "Vitamin C contributes to the reduction of tiredness and fatigue" (as long as the product contains above a specified amount of Vitamin C. I’m not aware of any trials that show vitamin C has the slightest effect on tiredness or fatigue, Although these laws do not come into effect until December 2012, they have already been invoked by the ASA has a reason not to uphold a complaint about a multivitamin pill which claimed that it “Includes 8 nutrients that can contribute to the reduction in tiredness and fatigue”
The Advertising Standards Authority (ASA). This is almost the only organisation that has done a good job on false health claims. Their Guidance on Health Therapies & Evidence says
"Whether you use the words ‘treatment’, ‘treat’ or ‘cure’, all are likely to be seen by members of the public as claims to alleviate effectively a condition or symptom. We would advise that they are not used"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
They are spot on.
The ASA’s Guidance for Advertisers of Homeopathic Services is wonderful.
"In the simplest terms, you should avoid using efficacy claims, whether implied or direct,"
"To date, the ASA has have not seen persuasive evidence to support claims that homeopathy can treat, cure or relieve specific conditions or symptoms."
That seems to condemn the (mis)labelling allowed by the MHRA as breaking the rules.. Sadly, though, the ASA has no powers to enforce its decisions and only too often they are ignored. The Nightingale collaboration has produced an excellent letter that you can hand to any pharmacist who breaks the rules
The ASA has also judged against claims made by "Craniosacral therapists" (that’s the lunatic fringe of osteopathy). They will presumably uphold complaints about similar claims made (I’m ashamed to say) by UCLH Hospitals.
The private examination company Edexcel sets exams in antiscientific subjects, so miseducating children. The teaching of quackery to 16 year-olds has been approved by a maze of quangos, none of which will take responsibility, or justify their actions. So far I’ve located no fewer than eight of them. The Office of the Qualifications and Examinations Regulator (OfQual), Edexcel, the Qualifications and Curriculum Authority (QCA), Skills for Health, Skills for Care, National Occupational Standards (NOS), private exam company VTCT and the schools inspectorate, Ofsted.. Asking any of these people why they approve of examinations in imaginary subjects meets with blank incomprehension. They fail totally to protect tha public from utter nonsense.
The Department of Education has failed to do anything about the miseducation of children in quackery. In fact it has encouraged it by, for the first time, giving taxpayers’ money to a Steiner (Waldorf) school (at Frome, in Somerset). Steiner schools are run by a secretive and cult-like body of people (read about it). They teach about reincarnation, karma, gnomes, and all manner of nonsense, sometimes with unpleasant racial overtones. The teachers are trained in Steiner’s Anthroposophy, so if your child gets ill at school they’ll probably get homeopathic sugar pills. They might well get measles or mumps too, since Steiner people don’t believe in vaccination.
Incredibly, the University of Aberdeen came perilously close to appointing a chair in anthroposophical medicine. This disaster was aborted by bloggers, and a last minute intervention from journalists. Neither the university’s regulatory mechanisms. nor any others, seemed to realise that a chair in mystical barmpottery was a bad idea.
Trading Standards offices and the Office of Fair Trading.
It is the statutory duty of Trading Standards to enforce the Consumer Protection Regulations (2008) This European legislation is pretty good. it caused a lawyer to write " Has The UK Quietly Outlawed “Alternative” Medicine?". Unfortunately Trading Standards people have consistently refused to enforce these laws. The whole organisation is a mess. Its local office arrangement fails totally to deal with the age of the internet. The situation is so bad that a group of us decided to put them to the test. The results were published in the Medico-Legal Journal, Rose et al., 2012. "Spurious Claims for Health-care Products: An Experimental Approach to Evaluating Current UK Legislation and its Implementation". They concluded "EU directive 2005/29/EC is
largely ineffective in preventing misleading health claims for consumer products in
the UK"
Skills for Health is an enormous quango which produces HR style "competences" for everything under the son. They are mostly quite useless. But those concerned with alternative medicine are not just useless. They are positively harmful. Totally barmy. There are competences and National Occupational Standards for every lunatic made-up therapy under the sun. When I phoned them to discover who’d written them, I learned that the had been drafted by the Prince of Wales’ Foundation for Magic Medicine. And when I joked by asking if they had a competence for talking to trees, I was told, perfectly seriously, “You’d have to talk to LANTRA, the land-based organisation for that.”
That was in January 2008. A lot of correspondence with the head of Skills for Health got nowhere at all. She understood nothing and it hasn’t improved a jot.
This organisation costs a lot of taxpayers’ money and it should have been consigned to the "bonfire of the quangos" (but of course there was no such bonfire in reality). It is a disgrace.
The Quality Assurance Agency (QAA) is supposed to ensure the quality of university courses. In fact it endorses courses in nonsense alternative medicine and so does more harm than good. The worst recent failure of the QAA was in the case of the University of Wales: see Scandal of the University of Wales and the Quality Assurance Agency. The university was making money by validating thousands of external degrees in everything from fundamentalist theology to Chinese Medicine. These validations were revealed as utterly incompetent by bloggers, and later by BBC Wales journalist Ciaran Jenkins (now working for Channel 4).
The mainstream media eventually caught up with bloggers. In 2010, BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. The programme can be seen on YouTube (Part 1, and Part 2). The programme also exposed, incidentally, the uselessness of the Quality Assurance Agency (QAA) which did nothing until the scam was exposed by TV and blogs. Eventually the QAA sent nine people to Malaysia to investigate a dodgy college that had been revealed by the BBC. The trip cost £91,000. It could have been done for nothing if anyone at the QAA knew how to use Google.
The outcome was that the University of Wales stopped endorsing external courses, and it was soon shut down altogether (though bafflingly, its vice-chancellor, Marc Clement was promoted). The credit for this lies entirely with bloggers and the BBC. The QAA did nothing to help until the very last moment.
Throughout this saga Universities UK (UUK), has maintained its usual total passivity. They have done nothing whatsoever about their members who give BSc degrees in anti-scientific subjects. (UUK used to known as the Committee of Vice-Chancellors and Principals).
Council for Health Regulatory Excellence (CHRE), soon to become the PSAHSC,
Back now to the CHRE, the people who failed so signally to sort out the GCC. They are being reorganised. Their consultation document says
"The Health and Social Care Act 20122 confers a new function on the Professional Standards Authority for Health and Social Care (the renamed Council for Healthcare Regulatory Excellence). From November 2012 we will set standards for organisations that hold voluntary registers for people working in health and social care occupations and we will accredit the register if they meet those standards. It will then be known as an ‘Accredited Register’. "
They are trying to decide what the criteria should be for "accreditation" of a regulatory body. The list of those interested has some perfectly respectable organisations, like the British Psychological Society. It also contains a large number of crackpot organisations, like Crystal and Healing International, as well as joke regulators like the CNHC.
They already oversee the Health Professions Council (HPC) which is due to take over Herbal medicine and Traditional Chinese Medicine, with predictably disastrous consequences.
Two of the proposed criteria for "accreditation" appear to be directly contradictory.
Para 2.5 makes the whole accreditation pointless from the point of view of patients
2.5 It will not be an endorsement of the therapeutic validity or effectiveness of any particular discipline or treatment.
Since the only thing that matters to the patient is whether the therapy works (and is safe), accrediting of organisations that ignore this will merely give the appearance of official approval of crystal healing etc etc. This appears to contradict directly
A.7 The organisation can demonstrate that there either is a sound knowledge base underpinning the profession or it is developing one and makes that explicit to the public.
A "sound knowledge base", if it is to mean anything useful at all, means knowledge that the treatment is effective. If it doesn’t mean that, what does it mean?
It seems that the official mind has still not grasped the obvious fact that there can be no sensible regulation of subjects that are untrue nonsense. If it is nonsense, the only form of regulation that makes any sense is the law.
Please fill in the consultation. My completed return can be downloaded as an example, if you wish.
Medicines and Healthcare products Regulatory Agency (MHRA) should be a top level defender of truth. Its strapline is
"We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
The MHRA did something (they won’t tell me exactly what) about one of the most cruel scams that I’ve ever encountered, Esperanza Homeopathic Neuropeptide, peddled for multiple sclerosis, at an outrageous price ( £6,759 for 12 month’s supply). Needless to say there was not a jot of evidence that it worked (and it wasn’t actually homeopathic).
Astoundingly, Trading Standards officers refused to do anything about it.
The MHRA admit (when pushed really hard) that there is precious little evidence that any of the herbs work, and that homeopathy is nothing more than sugar pills. Their answer to that is to forget that bit about "ensuring that medicines … work"
Here’s the MHRA’s Traditional Herbal Registration Certificate for devils claw tablets.

The wording "based on traditional use only" has to be included because of European legislation. Shockingly, the MHRA have allowed them to relegate that to small print, with all the emphasis on the alleged indications. The pro-CAM agency NCCAM rates devil’s claw as "possibly effective" or "insufficient evidence" for all these indications, but that doesn’t matter because the MHRA requires no evidence whatsoever that the tablets do anything. They should, of course, added a statement to this effect to the label. They have failed in their duty to protect and inform the public by allowing this labelling.
But it gets worse. Here is the MHRA’s homeopathic marketing authorisation for the homeopathic medicinal product Arnicare Arnica 30c pillules
It is nothing short of surreal.

|

|
Since the pills contain nothing at all, they don’t have the slightest effect on sprains, muscular aches or bruising. The wording on the label is exceedingly misleading.
If you "pregnant or breastfeeding" there is no need to waste you doctor’s time before swallowing a few sugar pills.
"Do not take a double dose to make up for a missed one". Since the pills contain nothing, it doesn’t matter a damn.
"If you overdose . . " it won’t have the slightest effect because there is nothing in them
And it gets worse. The MHRA-approved label specifies ACTIVE INGREDIENT. Each pillule contains 30c Arnica Montana
No, they contain no arnica whatsoever.

|

|
It truly boggles the mind that men with dark suits and lots of letters after their names have sat for hours only to produce dishonest and misleading labels like these.
When this mislabeling was first allowed, it was condemned by just about every scientific society, but the MHRA did nothing.
The Nightingale Collaboration.
This is an excellent organisation, set up by two very smart skeptics, Alan Henness and Maria MacLachlan. Visit their site regularly, sign up for their newsletter Help with their campaigns. Make a difference.
Conclusions
The regulation of alternative medicine in the UK is a farce. It is utterly ineffective in preventing deception of patients.
Such improvements as have occurred have resulted from the activity of bloggers, and sometime the mainstream media. All the official regulators have, to varying extents, made things worse.
The CHRE proposals promise to make matters still worse by offering "accreditation" to organisations that promote nonsensical quackery. None of the official regulators seem to be able to grasp the obvious fact that is impossible to have any sensible regulation of people who promote nonsensical untruths. One gets the impression that politicians are more concerned to protect the homeopathic (etc, etc) industry than they are to protect patients.
Deception by advocates of alternative medicine harms patients. There are adequate laws that make such deception illegal, but they are not being enforced. The CHRE and its successor should restrict themselves to real medicine. The money that they spend on pseudo-regulation of quacks should be transferred to the MHRA or a reformed Trading Standards organisation so they can afford to investigate and prosecute breaches of the law. That is the only form of regulation that makes sense.
Follow-up
The shocking case of the continuing sale of “homeopathic vaccines” for meningitis, rubella, pertussis etc was highlighted in an excellent TV programme by BBC South West. The failure of the MHRA and the GPC do take any effective action is a yet another illustration of the failure of regulators to do their job. I have to agree with Andy Lewis when he concludes
“Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator.”
|
This is a very important book. Buy it now (that link is to Waterstone’s Amazon don’t pay tax in the UK, so don’t use them). When you’ve read it, do something about it. The book has lots of suggestions about what to do. |

Stolen from badscience.net |
Peter Medawar, the eminent biologist, in his classic book Advice to a Young Scientist, said this.
“Exaggerated claims for the efficacy of a medicament are very seldom the consequence of any intention to deceive; they are usually the outcome of a kindly conspiracy in which everybody has the very best intentions. The patient wants to get well, his physician wants to have made him better, and the pharmaceutical company would have liked to have put it into the physician’s power to have made him so. The controlled clinical trial is an attempt to avoid being taken in by this conspiracy of good will.”
There was a lot of truth in that 1979, towards the end of the heyday of small molecule pharmacology. Since then, one can argue, things have gone downhill.
First, though, think of life without general anaesthetics, local anaesthetics, antibiotics, anticoagulants and many others. They work well and have done incalculable good. And they were developed by the drug industry.
But remember also that remarkably little is known about medicine. There are huge areas in which neither causes nor cures are known. Treatments for chronic pain, back problems, many sorts of cancer and almost all mental problems are a mess. It just isn’t known what to do. Nobody is to blame for this. Serious medical research has been going on for little more than 60 years, and it turns out to be very complicated. We are doing our best, but are still ignorant about whole huge areas. That leads to a temptation to make things up. Clutching at straws is very evident when it comes to depression, pain and Alzheimer’s disease, among others.
In order to improve matters, one essential is to do fair tests on treatments that we have. Ben Goldacre’s book is a superb account of how this could be done, and how the process of testing has been subverted for commercial gain and to satisfy the vanities of academics.
Of course there is nothing new in criticisms of Big Pharma. The huge fines levied on them for false advertising are well known. The difference is that Goldacre’s book explains clearly what’s gone wrong in great detail, documents it thoroughly, and makes concrete suggestions for improving matters.
Big Pharma has undoubtedly sometimes behaved appallingly in recent years. Someone should be in jail for crimes against patients. They have behaved in much the same way that bankers have. In any huge globalised industry it is always possible to blame someone in another department for the dishonesty. But they aren’t the only people to blame. None of the problems could have arisen with the complicity of academics, universities, and a plethora of regulatory agencies and professional bodies.
The biggest scandal of all is missing data (chapter 1). Companies, and sometmes academics, have suppressed of trials that don’t favour the drugs that they are trying to sell. The antidepressant drug, reboxetine, appeared at first to be good. It had been approved by the Medicines and Healthcare products Regulatory Agency (MHRA) and there was at least one good randomized placebo-controlled trial (RCT) showing it worked. But it didn’t. The manufacturer didn’t provide a complete list of unpublished trials when asked for them. After much work it was found in 2010 that, as well as the published, favourable trial, there were six more trials which had not been published and all six showed reboxetine to be no better than placebo . In comparisons with other antidepressant drugs three small studies (507 patients) showed reboxetine to be as good as its competitors. These were published. But it came to light that data on 1657 patients had never been published and these showed reboxetine to be worse than its rivals.
When all the data for the SSRI antidepressants were unearthed (Kirsch et al., 2008) it turned out that they were no better than placebo for mild or moderate depression. This selective suppression of negative data has happened time and time again. It harms patients and deceives doctors, but, incredibly, it’s not illegal.
Disgracefully, Kirsch et al. had to use a Freedom of Information Act request to get the data from the FDA.
“The output of a regulator is often simply a crude, brief summary: almost a ‘yes’ or ‘no’ about side effects. This is the opposite of science, which is only reliable because everyone shows their working, explains how they know that something is effective or safe, shares their methods and their results, and allows others to decide if they agree with the way they processed and analysed the data.”
|
“the NICE document discussing whether it’s a good idea to have Lucentis, an extremely expensive drug, costing well over £ 1,000 per treatment, that is injected into the eye for a condition called acute macular degeneration. As you can see, the NICE document on whether this treatment is a good idea is censored. Not only is the data on the effectiveness of the treatment blanked out by thick black rectangles, in case any doctor or patient should see it, but absurdly, even the names of some trials are missing, preventing the reader from even knowing of their existence, or cross referencing information about them.Most disturbing of all, as you can see in the last bullet point, the data on adverse events is also censored.”
|
The book lists all the tricks that are used by both industry and academics. Here are some of them.
- Regulatory agencies like the MHRA, the European Medicines Agency (EMA) and the US Food and Drugs Administration (FDA) set a low bar for approval of drugs.
- Companies make universities sign gagging agreements which allow unfavourable results to be suppressed, and their existence hidden.
- Accelerated approval schemes are abused to get quick approval of ineffective drugs and the promised proper tests often don’t materialise
- Disgracefully, even when all the results have been given to the regulatory agencies (which isn’t always). The MHRA, EMA and FDA don’t make them public. We are expected to take their word.
- Although all clinical trials are meant to be registered before they start, the EMA register, unbelievably, is not public. Furthermore there is no check that the results if trials ever get published. Despite mandates that results must be published within a year of finishing the trial, many aren’t. Journals promise to check this sort of thing, but they don’t.
- When the results are published, it is not uncommon for the primary outcome, specified before it started, to have been changed to one that looks like a more favourable result. Journals are meant to check, but mostly don’t.
- Companies use scientific conferences, phony journals, make-believe “seed trials” and “continuing medical education” for surreptitious advertising.
- Companies invent new diseases, plant papers to make you think you’re abnormal, and try to sell you a “cure”. For example, female sexual dysfunction , restless legs syndrome and social anxiety disorder (i.e. shyness). This is called disease-mongering, medicalisation or over-diagnosis. It’s bad.
- Spin is rife. Companies, and authors, want to talk up their results. University PR departments want to exaggerate benefits. Journal editors want sensational papers. Read the results, not the summary. This is universal (but particularly bad in alternative medicine).
- Companies fund patient groups to lobby for pills even when the pills are known to be ineffective. The lobby that demanded that Herceptin should be available to all on the breast cancer patients on the NHS was organised by a PR company working for the manufacturer, Roche. But Herceptin doesn’t work at all in 80% of patients and gives you at best a few extra months of life in advanced cases.
- Ghostwriting of papers is serious corruption. A company writes the paper and senior academics appear as the authors, though they may never have seen the original data. Even in cases where academics have admitted to lying about whether they have seen the data, they go unpunished by their universities. See for example, the case of Professor Eastell.
- By encouraging the funding of “continuing medical education” by companies, the great and the good of academic medicine have let us down badly.
This last point is where the book ends, and it’s worth amplification.
“So what have the great and good of British medicine done to help patients, in the face of this endemic corruption, and these systematic flaws? In 2012, a collaborative document was produced by senior figures in medicine from across the board, called ‘Guidance on Collaboration Between Healthcare Professionals and the Pharmaceutical Industry’. This document was jointly approved by the ABPI, the Department of Health, the Royal Colleges of Physicians, Nursing, Psychiatrists, GPs, the Lancet, the British Medical Association, the NHS Confederation, and so on. ”
“It contains no recognition of the serious problems we have seen in this book. In fact, quite the opposite: it makes a series of assertions about them that are factually incorrect.”
“It states that drug reps ‘can be a useful resource for healthcare professionals’. Again, I’m not sure why the Royal Colleges, the BMA, the Department of Health and the NHS Confederation felt the need to reassert this to the doctors of the UK, on behalf of industry, when the evidence shows that drug reps actively distort prescribing practices. But that is the battle you face, trying to get these issues taken seriously by the pinnacle of the medical establishment.”
This is perhaps the most shameful betrayal of all. The organisations that should protect patients have sold them out.
You may have been sold out by your “elders and betters”, but you can do something. The “What to do” sections of the book should be produced as a set of flash cards, as a reminder that matters can be improved.
It is shameful that this book was not written by a clinical pharmacologist, or a senior doctor, or a Royal College, or a senior academic. Why has the British Pharmacological Society said nothing?
It is shameful too that this book was not written by one of the quacks who are keen to defend the $60 billion alternative medicine industry (which has cured virtually nothing) and who are strident in their criticism of the 600 billion dollar Pharma industry. They haven’t done the work that Goldacre has to analyse the real problems. All they have done is to advocate unfair tests, because that is the only sort their treatments can pass.
It’s weird that medicine, the most caring profession, is more corrupt than any other branch of science. The reason, needless to say, is money. Well, money and vanity. The publish or perish mentality of senior academics encourages dishonesty. It is a threat to honest science.
Goldacre’s book shows the consequences: harm to patients and huge wastage of public money.
Read it.
Do something.
Follow-up
7 October, 2012, The Observer
Goldacre wrote
"I think it’s really disappointing that nobody, not the Royal Colleges, the Academy of Medical Sciences, the British Pharmacological Society, the British Medical Association, none of these organisations have stood up and said: selective non-publication of unflattering trial data is research misconduct, and if you do it you will be booted out. And I think they really urgently should."
Exactly.
Much has been written on this blog about Dr Michael Dixon, and about the "College of Medicine", which is the direct inheritor of the mantle of the late, unlamented, Prince’s Foundation for Integrated Health. At the time of the foundation of the College it was stated that "The College represents a new strategy to take forward the vision of HRH Prince Charles".
Michael Dixon has also been chairman of the NHS Alliance since 1998. That was one of very few organisations to support Andrew Lansley’s Health Bill. No doubt he will be happy for Crapita Capita to supply alternative nonsense at public expense.
Dr Dixon took offence to a review in The Times of Mark Henderson’s new book, The Geek Manifesto.
 .
.
The review, by David Aaronovitch, said, apropos of the 1023 campaign,
" . . .there was now, almost for the first time, a group of people who were not content to see claims made for discredited treatments without making everyone aware of the science that disproved those claims. And second, what they were doing had implications for public policy."
and
"The geeks represent, for me, one of the most encouraging recent developments in British public life."
This excellent review evidently upset Dr Dixon, because on 20th May, his letter appeared in the Times.
|
David Aaronovitch is right to argue for a robust scientific approach in medicine. However, he is not being logical or scientific when he says that if something is suspected to be placebo then it has no benefit and the NHS should not pay for it. What about scientific research on remedies that many believe to be placebo? These frequently show that there is a benefit but this is confined to those who believe in the treatment given. Surely, in such cases, it would be logical to say that the treatment was beneficial albeit in a specific group of “believers”. From there, it would be good science to compare the safety costs of this supposed placebo remedy with its currently given alternative before deciding whether “believers” should be able to receive such a remedy on the NHS. The problem here is that belief and mindset play an enormous part in healing – science needs to take account of this. Patients’ symptoms are frequently metaphors and effective treatment can often be symbolic and culturally dependent. The mind, in the right circumstances, can produce its own healing chemicals often mimicking those given in conventional medicine. Until science can explain healing in psychosocial as well as biomedical language, we must be cautious about “voting for the geeks” as Mr Aaronovitch suggests. It is far better surely that individual treatment should be tailored, within reason, to the patient and their beliefs and perspectives. Further more, might it not be wiser to direct NHS resources according to pragmatic trials of cost effectiveness and safety rather than a limited interpretation of science that excludes the effect of the mind? Dr Michael Dixon Chair of Council College of Medicine. |
This letter seemed remarkable to me. It is very close to being an admission that alternative medicine is largely placebo. It called for a reply.
We have been here before. Many people have discussed the dubious ethics of deceiving patients by giving placebos while pretending they are no such thing. There is wide agreement that it is not only unethical, but also unnecessary. Kevin Smith has written a scholarly essay on the topic. Edzard Ernst wrote Mind over matter? Margaret McCartney, the Glasgow GP, and author of The Patient Paradox, has explained it. Some views of Dr Dixon’s approach are less flattering than mine. For example, from the USA, Steven Novella’s Dr. Michael Dixon – “A Pyromaniac In a Field of (Integrative) Straw Men”. And, from Majikthyse, Michael Dixon caught red-handed!, and Dr Aust’s Dr Michael Dixon is annoyed. The list is almost endless.
.Two replies were published in the Times on 26 May (and they were the lead letters -bold print). One from the excellent Evan Harris, and one from me.
![]()
Here they are as text.
|
Sir, Dr Michael Dixon’s letter (May 21) is fascinating. He is, of course, a well-known advocate of alternative medicine. Yet he seems now to believe that much alternative medicine is just a placebo. That’s something the geeks have been saying for years, and he appears, at last, to have accepted it. That being the case, it follows that we have to ask whether placebos produce useful benefits, and whether it is ethical to prescribe them. Nobody denies the existence of placebo effects. But recent research has shown that they are usually both small and transient. Often they are not big enough to provide a useful degree of relief. For example, a recent paper on acupuncture in the British Journal of General Practice showed that it had a remarkably small placebo effect. And placebos have no effect at all on the course of cancer or infectious diseases. There has been an admirable movement in medicine for doctors to be open and honest with patients. Prescribing of medicines that contain no active ingredient involves lying to patients. That is old-fashioned and unethical. It is fair to ask why so many people seem to believe in alternative medicine, if even their placebo effects are small. The answer seems to lie in the “get better anyway” effect (known to geeks as regression to the mean). Most of the conditions for which placebos seem to work are things that wax and wane naturally. You take the “cure” when you are at your worst, and next day you are better. You would have been better anyway, but it’s hard to avoid attributing the improvement to whatever you took. That is why alternative medicine is advertised largely on the basis of anecdotal testimonials. And it is doubtless why Dr Dixon advocates “pragmatic” trials: that’s a euphemism for trials without a proper control group. Psychosocial problems may indeed be very important for some patients. But deceiving such patients with dummy pills is not the proper way to deal with their problems. D. Colquhoun, FRS Professor of Pharmacology, University College London Sir, Dr Michael Dixon argues that the NHS should fund placebo treatments such as homeopathy (though he stops short of agreeing that homeopathy is a placebo) on the basis that they can offer limited help to those who “believe” in them. It is no part of modern ethical medical practice to deceive patients into thinking — or failing to disabuse them of the belief — that an inert substance or ineffective medicine has beneficial effects. This can not be justified by the hope — or even expectation — of deriving for that patient the limited psychologically based improvement in symptoms that may follow from the deployment of the placebo. Pedlars of homeopathy for profit in the private sector will, alas, always seek to fool people into believing the hocus pocus of “memory of water” and the effects of infinite dilution and a lot of bottle-shaking. But doctors have responsibilities not to deceive their patients, even out of a paternalistic wish to assist them to manage their symptoms; and public policy demands that the NHS spends its resources only on treatments that work without deception in a cost-effective way. Dr Evan Harris Oxford |
Follow-up
Our undercover investigation finds evidence of nutritional therapists giving out advice that could seriously harm patients’ health
That’s the title of an article in February’s Which? magazine. (That’s similar to Consumer Reports in the USA).
“When Which? sent researchers to investigate the quality of advice from nutritional therapists, some was so bad that patients’ health was put at risk. One nutritional therapist advised against surgery and radiotherapy to treat cancer, while another ‘diagnosed’ a problem with adrenal glands without any blood-test results. Some also used unproven testing, such as iridology or mineral testing, to identify problems or diagnose conditions.”
"We sent five undercover researchers to visit three nutritional therapists each. Every researcher was equipped with a specific health-related scenario: Helen (46) and Sarah (40), recently diagnosed with Ductal Carcinoma In Situ (DCIS), the most common type of non-invasive breast cancer; Mark (56) and Linda (52), suffering with serious fatigue for the past three months; and Emily (31), trying unsuccessfully to conceive for more than a year."
|
Sarah, posing as a patient diagnosed with DCIS, visited a nutritional therapist who advised her to delay treatment recommended by her oncologist (a lumpectomy and a course of radiotherapy). The therapist suggested that Sarah follow a no-sugar diet for three to six months and told her, ‘cancer lives off sugar; if you feed it sugar it’s going to thrive. If we starve the cancer of sugar then you have a better opportunity of the cancer going away’. When Sarah asked whether the cancer could progress during this time the therapist said it was a ‘gamble’. Dr Margaret McCartney, from our panel of experts, says: ‘If cancer treatment were as simplistic as cutting out sugar, surely we would have discovered a cure. This advice is highly irresponsible.’ Our experts rated this consultation as a ‘dangerous fail’." The Patients’ Guide to magic medicine defined “Nutritional therapy: self-styled ‘nutritionists’ making untrue claims about diet in order to sell you unnecessary supplements”. That turned out to be pretty accurate. They are part of the alternative medicine fringe. The Universities Admission Service (UCAS) no longer lists any BSc/MSc degrees in "Nutritional Therapy" or "Nutritional medicine". Westminster University closed its BSc Nutritional Therapy during last year. We still don’t know the fate of the notorious (or should I say hilarious) course run at the Northern College of Acupuncture and validated (after a fashion) by the late University of Wales, but it isn’t listed for entry in 2012. [We do now: see follow-up‘] But there are a large number of university courses called "Nutrition". How many of them teach properly, and how many of them teach the nonsense that prevails in "nutritional therapy", I don’t know. The term ‘nutrition’ has turned into a dangerous minefield. It can mean almost anything, because the term is undefined. Anyone can, and does, describe themselves as a nutritionist. At one extreme you have slick pills salesman like ‘not-a-Dr’ Gillian McKeith and Patrick Holford. At the other extreme you have a fascinating and respectable subject for study. The one thing that you need to get clear is that if you want advice about nutrition, go to a dietitian not a "nutritionist". Dietitians are the properly qualified people who work in the NHS, and who are (mostly) free of crackpot ideas. |
I suppose that one should not be surprised at the poor, and sometimes dangerous, advice that was given by nutritional therapists. Their training contains much nonsense so it isn’t surprising that they did so badly. Some of it has been revealed here. See, for example,
Another worthless validation: the University of Wales and nutritional therapy
Nutritional Fairy Tales from Thames Valley University
College of Natural Nutrition: bizarre teaching revealed
Nutriprofile: useful aid or sales scam?
Response to a threatening letter from Mr Holford
Food for the Brain: Child Survey. A proper job?
Teaching bad science to children: OfQual and Edexcel are to blame
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
The level of knowledge of both physiology and chemistry shown my some of the therapists was shocking. One recommended avoiding margarine, because it’s “two chemical bonds away from pure plastic”. Another said that Flora margarine contains lots of trans fat, which has not been true for a long time.
One graduate ot the late Thames Valley University course said “”advantage of the wholemeal or the wholegrain … is that they contain more fibre and the fibre stops the sugars being absorbed quite as quickly”. Not so. Brown and white bread have much the same glycaemic index (60 – 70).
Quack diagnosis
One alarming fact was that several therapists offered methods of diagnosis for allergy and for deficiencies that have been known for many years not to work. There isn’t anything controversial about iridology, hair mineral analysis, taste tests. kinesiology. or the Vega test. They are pure quackery.
“Professor David Colquhoun, from our panel of experts, said: ‘Sadly, nutritional therapy is plagued by “diagnostic tests” that are little more than quackery; they are tools to aid sales, rather than tools to diagnose deficiencies. Iridology and hair analysis simply don’t work.”
Unnecessary treatments
One therapist advised a researcher to have an optimum nutritional evaluation test, costing £312, and a cellular nutrition profile, costing £156. Apparently, these would allow the therapist to give a
more targeted service by establishing what vitamin and mineral deficiencies he had.
Our experts were not convinced by these tests and certainly didn’t think they were worth the money; any necessary testing
could be done by a GP for free.
In 12 of the 15 consultations, researchers were prescribed a huge range of supplements, costing up to £70 per month. It was not revealed whether or not the prescriber made money from this, but usually you were asked to give the prescriber’s name "to get a discount". So it’s a fair guess that they got kickbacks.
British Association for Applied Nutrition & Nutritional Therapy (BANT)
Despite the low standards of advice, 13 out of the 14 therapists who were visited were registered with BANT, the British Association for Applied Nutrition & Nutritional Therapy. This is what passes for a professional association for nutritional therapists, though like all such bodies in alternative medicine, it is entirely ineffective as a regulator. Rather it serves to protect whatever untrue claims they make. BANT’s code of practice says that its members won’t diagnose, but in fact many of the therapists diagnosed conditions and created treatment plans. You can be confident that BANT will do nothing to stop this bad practice.
You can find out a lot about BANT from these sources:
British Association for Nutritional Therapy – when an organisation looks like a regulator, quacks like a regulator, but isn’t a regulator
Why it is easy to get the incorrect impression that BANT is a regulator
Nutritional Therapists Fail to Join Ofquack
BANT: A Profile
Matthias Rath drops his million pound legal case against me and the Guardian.
Only 3 of the 14 therapists were registered with the Complementary and Natural Healthcare Council (the CNHC, more commonly know as Ofquack). They are meant to be the official regulator, launched with a good chunk of taxpayers’ money, but registration is voluntary and not many have volunteered. As a requlator, Ofquack is a bad joke.
Conclusion
|
"Dr Margaret McCartney says: ‘This investigation appears to show that high street nutritional therapists are a waste of money. If you have symptoms please see your GP, not someone who can’t diagnose accurately.’ If you’re looking for tailored dietary advice, visit a registered dietitian.
" |
There is a discussion of this topic on the Which? magazine site.
Follow-up
The excellent Quackometer has posted simultaneously on the great nutritional therapy scam.
16 January 2012 The British Dietetic Association issued a press release that describes very clearly the many differences between a real dietitian and a "nutritional therapist". Download Leading UK Nutrition Association Urges Awareness Between Dietitians and Nutritionists (pdf).
16 January 2012 BANT issued a press release. Download Are Nutritional Therapists Gambling with Your Health?. It answers none of the serious questions raised by the Which? investigation. BANT moans that that Which? “did not provide all the promised transcripts/questionnaires in a timely fashion”. In fact they got them before Christmas and were given until January 15th to respond.
16 January 2012. BBC Radio 4 programme, You and Yours, had an item with Jenny Driscoll from Which? magazine and BANT chairperson, Catherine Honeywell. She did, inter alia, admit that some of the behaviour of the therapists were irresponsible. It remains to be seen if they do anything about it. don’t hold your breath. Hear it on BBC iPlayer.
16 January 2012. There was pretty god coverage of the story, even in the Daily Mail.
17 January 2012 Another question answered. I just learned that the ludicrous course in Nutritional Therapy, previously validated by the University of Wales (and a contributor to its downfall), is now being validated by, yes, you guessed, Middlesex University. Professor Driscoll seems determined to lead his univerity to the bottom of the academic heap. His new partnership with the Northern college of Acupuncture is just one of a long list of validations that almost rivals that of the late University of Wales. The course has, of course, an enthusiastic testimonial, from a student. It starts
I work full time as a team leader for a pension company but I am also a kinesiologist and work in my spare time doing kinesiology, reiki and Indian head massage.
Evidently she’s a believer in the barmiest and totally disproved forms of magic medicine. And Middlesex University will give her a Master of Science degree. I have to say I find it worrying that she’s a team leader for a pension company. Does she also believe in the value of worthless derivatives. I wonder?
17 January 2012 The discussion is going on at the Which? web site. A Chris James cast doubt on the reaults because ot the small sample size, and asked for confidence limits, so I gave them.
Chris James
It is easy enough to calculate limits yourself -you don’t even need to be able to do the maths -there are web calculators that do it for you, e.g. http://www.causascientia.org/math_stat/ProportionCI.html
14/15 = 93% failed. 95% confidence limits for this are 69.8% to 98.4%
6/15 = 40% gave dangerous advice 95% confidence limits 19.7% to 64.6%
So despite the small sample size we can say that it’s likely that at least 70% (and possibly 98%) of nutritional therapists fail.
And it is likely that at least 20% (and possibly 65%) of nutritional therapists give dangerous advice.
These results give real cause for concern, despite the small sample size.
For statistical enthusiasts, these limits are Bayesian with a uniform prior. Very much the same result is given by the standard analysis which is explained in section 7.7 of Lectures on Biostatistics [download pdf 10.5 Mb]
18 January 2012. BANT has, at last, produced an “updated response”. The good thing is that it starts by saying
” . . it is completely outside the BANT Code of Practice to advise a client to withhold any treatment for cancer for any period of time in order to follow a nutritional approach. Were a client to be advised in such a way we would expect to receive a complaint against the practitioner.”
I hope that this will happen. This statement, the only admission of guilt in BANT’s response, is rather spoiled by a later suggestion that no such recommendation was made. It looked very clear to both Which? magazine and to the three members of the expert panel.
The rest of the response admits no fault of any sort.
I’m sorry to say that the response by BANT shows very clearly what is wrong in nutritional therapy. Any organisation which can see nothing wrong in the advice given in 14 of the 15 consultations is, I’d argue, a threat to the health of the nation. Rather than saying we’ll try to improve, they just deny everything.
The response seems to show that the professional organisation for nutritional therapists is not part of the solution. Rather it is part of the problem.
Since writing about anti-scientific degrees in Nature (March 2007), much has been revealed about the nonsense that is taught on these degrees. New Year’s day seems like a good time to assess how far we’ve got, five years on.
At the beginning of 2007 UCAS (the universities central admission service) offered 45 different BSc degrees in quackery, at 16 universities.
Now there are only 24 such degrees.
If you exclude chiropractic and osteopathy, which all run at private colleges, with some sort of "validation" from a university, there are now only 18 BSc/MSc courses being offered in eight universities.
Degrees in homeopathy, naturopathy and "nutritional therapy", reflexology and aromatherapy have vanished altogether from UCAS.
In the race to provide BScs in anti-science, Middlesex University has now overhauled the long-standing leader, Westminster, by a short head.
 Michael Driscoll, vice-chancellor of Middlesex |
|
Let’s see what’s gone.
The University of Central Lancashire (UCLAN) was the first to see sense. In August 2008 they announced closure of their “BSc” degree in homeopathy. On September 2008 they announced an internal review of their courses in homeopathy. herbalism and acupuncture. The report of this review closed down all of them in July 2009. I first asked for their teaching materials in July 2006. I finally got them in December 2010, after winning an appeal to the Information Commissioner, and then winning an appeal against that decision at an Information tribunal . By the time I got them, the course had been closed for over two years. That is just as well, because it turned out that UCLAN’s students were being taught dangerous nonsense. No wonder they tried so hard to conceal it.
Salford University was the next to go. They shut down their courses in complementary medicine, homeopathy and acupuncture. In January 2009 they announced " they are no longer considered “a sound academic fit” ". Shortly afterwards. a letter appeared in The Times from three heavyweights (plus me) congratulating the vice-chancellor on his decision.
University of Westminster
For many years, Westminster was the biggest supplier of BSc degrees in quackery. At the beginning of 2007 they offered 14 different BSc degrees in homeopathy, naturopathy, nutritional therapy, "complementary therapies", (western) herbal medicine and traditional Chinese medicine with acupuncture. Some of their courses were so bizarre that some of the students and even staff sent me slides which taught things like "amethysts emit high Yin energy". Like UCLAN, Westminster also held an internal review. Unlike UCLAN it came to the absurd conclusion that all would be well if they injected more science into the courses. The incompetence of the review meant that those who wrote it hadn’t noticed that if you try to put science into homeopathy or naturopathy, the whole subject vanishes in a puff of smoke. Nevertheless Westminster closed down entry to BSc homeopathy in March 2009 (though the subject remained as part of other courses).
Three years after the Nature article, all five BSc homeopathy degrees had shut their doors.
During 2011, Westminster shut down Naturopathy, Nutritional therapy, Therapeutic bodywork and Complementary Medicine. See, for example,
More dangerous nonsense from the University of Westminster: when will Professor Geoffrey Petts do something about it?
Now Westminster has only four courses in two subjects. They still teach some dangerous and untrue things, but I suspect the writing is on the wall for these too.
I have seen a document, dated 11 April 2011, which states
“The following courses have been identified as ‘at risk’ (School definition) and will be discussed at the APRG and University Review Group2, due to poor recruitment and high cost of delivery:
Integrated Health Scheme: BSc Complementary Medicine, Naturopathy; BSc Chinese Medicine; BSc Nutritional Therapy; BSc Herbal Medicine”
All but Chinese medicine and Herbal medicine have already gone. Almost there.
University of Wales
Since my first post in 2008 about the validation scam operated by the University of Wales, and some good investigations by BBC Wales TV, the outcome was the most spectacular so far. The entire institution collapsed. They no longer "validate" external degrees at dodgy business colleges, loony religious colleges or magic medicine colleges.
Another worthless validation: the University of Wales and nutritional therapy (October 2008) This is a ‘degree’ in nutrtional therapy. It is even more hilarious than usual, but it passed the validation anyway.
Scandal of the University of Wales and the Quality Assurance Agency (November 2010). This post followed the BBC Wales TV programme. At last the QAA began to notice, yet further confirmation of its utter ineptitude.
The University of Wales disgraced (but its vice chancellor is promoted) (October, 2011) The eventual collapse of the university was well-deserved. But it is very weird that the people who were responsible for it have still got their jobs. In fact the vice-chancellor, Marc Clement, was promoted despite his mendacious claim to be unaware of what was going on.
It remains to be seen how many of the many quack courses that were validated by the University of Wales will be taken on by other universities. The McTimoney College of Chiropractic is owned by BPP University (so much for their quality control, as explained in Private Eye). but still claims to be validated by Wales until 2017.
Some of the more minor players
Edinburgh Napier University. After an FOI request (rejected), Napier closed their herbal medicine degree in 2010.
Hot and cold herbal nonsense from Napier University Edinburgh: another course shuts. (June 2010)
As expected, the Scottish Information Commissioner agreed with that for England and Wales and ordered material to be sent. Edinburgh Napier University teaches reflexology, aromatherapy and therapeutic touch. Scottish Information Commissioner says you should know. Some of the horrors so discovered appeared in Yet more dangerous nonsense inflicted on students by Edinburgh Napier University. The embarrassment seems to have worked. Their remaining degrees in aromatherapy and reflexology have now vanished from UCAS too. All that remains is a couple of part time “Certificates of Credit” for aromatherapy and reflexology
Anglia Ruskin Univerity Not only have BSc degrees gone in aromatherapy and reflexology, but their midwifery degree now states "We are unable to accept qualifications in aromatherapy, massage and reflexology."
University of Derby Reflexology and aromatherapy have gone, though doubtless Spa management therapies have much nonsense left
University of Greenwich. BSc in Complementary Therapies (Nutritional Health) and BSc in Complementary Therapies (Nutritional Health) have been shut. The BSc Acupuncture is listed on their web site but it is under review, and is not listed in UCAS for 2012. (Acupuncture is run at International College of Oriental medicine, validated by Greenwich.). Only osteopathy (MOst) is still running, and that is a validation of an external course run at The European School of Osteopathy, in Maidstone
Thames Valley University was renamed the University of West London in 2010. The nonsense that was run there (e.g. Nutritional Fairy Tales from Thames Valley University) seems to have vanished. Their previous alt med guru, Nicola Robinson, appears now to be at London South Bank University (ranked 116 out of the 116 UK universities)
What’s left?
Chiropractic Surprisingly, given the total discreditation of chiropractic in the wake of the Simon Singh affair, and the internecine warfare that followed it, none of the chiropractic courses have shut yet. Some are clearly in trouble, so watch this space.
Osteopathy has also had no course closures since 2007. Like chiropractic it also suffers from internecine warfare. The General Osteopathic Council refuses to disown the utter nonsense of "craniosacral" osteopathy. But the more sensible practitioners do so and are roughly as effective as physiotherapists (though there are real doubts about how effective that is).
Excluding chiropractic and osteopathy, this is all that’s left. It now consists almost entirely of Chinese medicine and a bit of herbal.
Glyndwr university (Known as North East Wales Institute until 2008) Ranked 104 out of 116 UK universities
BSc Acupuncture (B341) BSc
BSc Complementary Therapies for Healthcare (B343)
Cardiff Metropolitan University (UWIC) (Known as University of Wales Institute Cardiff (UWIC) until Nov 2011.) The vice-chancellor of Cardiff Metropolitan, Antony Chapman, is in the QAA’s board of directors, so perhaps it isn’t surprising that the QAA has done nothing.
BSc Complementary Therapies (3 years) (B390)
BSc Complementary Therapies (4 yrs inc Foundation) (B300)
University of Lincoln
Acupuncture (B343) 3FT Hon BSc
Herbal Medicine (B342) 3FT Hon BSc
University of East London Ranked 113 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
London South Bank University Ranked 116 out of 116 UK universities
Acupuncture (B343) 4FT Deg MCM
The Manchester Metropolitan University Ranked 93 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
Middlesex University
Acupuncture (B348) 3FT Hon BSc
Ayurvedic Medicine (A900) 4FT Oth MCM
Herbal Medicine (B347) 3FT Hon BSc
Traditional Chinese Medicine (BT31) 4FT Hon BSc
University of Westminster
Chinese Medicine: Acupuncture (B343) 3FT Hon BSc
Chinese Medicine: Acupuncture with Foundation (B341) 4FT/5FT Hon BSc/MSci
Herbal Medicine (B342) 3FT Hon BSc
Herbal Medicine with Foundation Year (B340) 4FT/5FT Hon BSc/MSci
It seems that acupuncture hangs on in universities that are right at the bottom of the rankings.
Manchester Metropolitan gets the booby prize for actually starting a new course, just as all around are closing theirs. Dr Peter Banister, who was on the committee that approved the course (but now retired), has told me ” I am sceptical in the current economic climate whether it will prove to be successful”. Let’s hope he’s right.
But well done Westminster. Your position as the leader in antiscientific degrees has now been claimed by Middlesex University. Their "degrees" in Ayurveda mark out Middlesex University as the new King of Woo.
Over to you, Professor Driscoll. As vice-chancellor of Middlesex University, the buck stops with you.
Both still teach Chinese and herbal medicine, which are potentially dangerous. There is not a single product from either that has marketing authorisation from the MHRA, though the MHRA has betrayed its trust by allowing misleading labelling of herbal medicines without requiring any evidence whatsoever that they work, see, for example
Why degrees in Chinese medicine are a danger to patients
More quackedemia. Dangerous Chinese medicine taught at Middlesex University
Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me
Sub-degree courses
In contrast to the large reduction in the number of BSc and MSc degrees, there has actually been an increase in two year foundation degrees and HND courses in complementary medicine, at places right near the bottom of the academic heap. The subject is sinking to the bottom. With luck it will vanish entirely from universities before too long.
Research-intensive Universities
Although all of the degrees in magic medicine are from post-1992 universities, the subject has crept into more prestigious universities. Of these, the University of Southampton is perhaps the worst, because of the presence of George Lewith, and his defender, Stephen Holgate. Others have staunch defenders of quackery, including the University of Warwick, University of Edinburgh and St Batholomew’s.
Why have all these courses closed?
One reason is certainly the embarrassment caused by exposure of what’s taught on the courses. Professors Petts (Westminster) and Driscoll (Middlesex) must be aware that googling their names produces references to this and other skeptical blogs on the front page. Thanks to some plain brown emails, and, after a three year battle, the Freedom of Information Act, it has been possible to show here the nonsense that has been foisted on students by some universities. Not only is this a burden on the taxpayer, but, more importantly, some of it is a danger to patients.
When a course closes, it is often said that it is because of falling student numbers (though UCLAN and Salford did not use that excuse). Insofar as that is true, the credit must go to the whole of the skeptical movement that has grown so remarkably in the last few years. Ben Goldacre’s "ragged band of bloggers" have produced a real change in universities and in society as a whole.
The people who should have done the job have either been passive or an active hindrance. The list is long. Vice-chancellors and Universities UK (UUK), the Quality Assurance Agency (QAA), the Hiigher Education Funding Council England (HEFCE), Skills for Health, the Medicines and Health Regulatory Authority ( MHRA) , the Health Professions Council (HPC), the Department of Health, the Prince of Wales and his reincarnated propaganda organisation, the "College of Medicine", the King’s Fund, the Universities and Colleges Union (UCU), OfQual, Edexcel, National Occupational Standards and Qualifications and the Curriculum Authority (QCA).
Whatever happened to that "bonfire of the quangos"?
Follow-up
2 January 2012 The McTimoney College of Chiropractic (owned by BPP University) claims that its “validation” by the University of Wales will continue until 2017. This contradicts the statement from UoW. Watch this space.
3 January 2012. Thanks to Neil O’Connell for drawing my attention to a paper in Pain. The paper is particularly interesting because it comes from the Southampton group which has previously been sympathetic to acupuncture. Its authors include George Lewith. It shows, yet again that there is no detectable difference between real and sham acupuncture treatment. It also shows that the empathy of the practitioner has little effect: in fact the stern authoritarian practitioner may have been more effective.
Patients receiving acupuncture demonstrated clinically important improvements from baseline (i.e., a 29.5% reduction in pain), but despite this, acupuncture has no specific efficacy over placebo for this group of patients. The clinical effect of acupuncture treatment and associated controls is not related to the use of an acupuncture needle, nor mediated by empathy, but is practitioner related and may be linked to the perceived authority of the practitioner.”
Sadly. the trial didn’t include a no-treatment group, so it is impossible to say how much of the improvement is regression to the mean and how much is a placebo effect. The authors admit that it could be mostly the former.
Surely now the misplaced confidence in acupuncture shown by some medical and university people must be in tatters.
In yet another sign that even acupuncture advovates are beginning to notice that it doesn’t work, a recent article Paradoxes in Acupuncture Research: Strategies for Moving Forward, shows some fascinating squirming.
3 January 2012. The Daily Telegraph has carried a piece about closure of university courses, written by Michael Hanlon. On 31 January they carried a much longer piece.
3 January 2012. It is a great pity that some physiotherapists seem to have fallen hook, line and sinker for the myths of acupuncture. Physiotherapists are, by and large, the respectable face of manipulative therapy. Their evidence base is certainly not all one would wish, but at least they are free of the outrageous mumbo humbo of chiropractors. Well, most of them are, but not the Acupuncture Association of Chartered Physiotherapists (AACP), or, still worse, The Association of Chartered Physiotherapists in Energy Medicine, a group that is truly away with the fairies. These organisations are bringing a very respectable job into disrepute. And the Health Professions Council, which is meant to be their regulator, has, like most regulators, done nothing whatsoever to stop it.
5 January 2012. Times Higher Education gives a history of the demise of the University of Wales, Boom or Bust. It’s a useful timeline, but like so many journalists, it’s unwilling to admit that bloggers were on to the problem long before the BBC, never mind the QAA.
There was also a leader on the same topic, Perils of the export business. It again fails to take the QAA to task for its failures.
Interviews for Deutsche Welle and Middle East Broadcasting Center TV.
17 January 2012 Another question answered. I just learned that the ludicrous course in Nutritional Therapy, previously validated by the University of Wales (and a contributor to its downfall), is now being validated by, yes, you guessed, Middlesex University. Professor Driscoll seems determined to lead his univerity to the bottom of the academic heap. His new partnership with the Northern college of Acupuncture is just one of a long list of validations that almost rivals that of the late University of Wales. The course has, of course, an enthusiastic testimonial, from a student. It starts
I work full time as a team leader for a pension company but I am also a kinesiologist and work in my spare time doing kinesiology, reiki and Indian head massage.
Evidently she’s a believer in the barmiest and totally disproved forms of magic medicine. And Middlesex University will give her a Master of Science degree. I have to say I find it worrying that she’s a team leader for a pension company. Does she also believe in the value of worthless derivatives. I wonder?
18 January 2012. the story has gone international, with an interview that I did for Deutsche Welle, UK universities drop alternative medicine degree programs. I’m quoted as saying “They’re dishonest, they teach things that aren’t true, and things that are dangerous to patients in some cases”. That seems fair enough.
There is also an interesting item from July 2010 about pressure to drop payment for homeopathy by German health insurance
31 January 2012
The Daily Telegraph carried a prominent 1200 word account (the title wasn’t mine). The published version was edited slightly.
The offering of quack cancer treatments at an exorbitant price is simple cruelty. The nature of the Burzynski clinic has been known for some time. But it has come to a head with some utterly vile threatening letters sent to the admirable Andrew Lewis, because he told a few truths about Stanislaw Burzynski’s despicable outfit. Please read his original post, The False Hope of the Burzynski Clinic.
I have to add by two-pennorth worth to the row that has blown up in the blogosphere at the outrageous behaviour of Burzynski. I hope other bloggers will do the same. There is safety in numbers. We need a Streisand effect to face down these pathetic bullies. It’s the "I am Spartacus" principle.
I won’t repeat all the details. They have spread like wildfire round the web. Briefly, it was sparked off by tragic case of a 4-year old girl, Billie Bainbridge who has a rare form of brain cancer. Well-intentioned pop stars have been trying to raise £200,000 to "enrol her into a clinical trial" at Burzynski clinic in Texas, despite the fact that Dr Stanislaw Burzynski has already been on trial for cancer fraud. In fact his clinic is not allowed to treat cancer patients, but it has evaded that ban, for many years, by pretending to run clinical trials. Normally patients volunteer for clinical trials. Sometimes they are paid a modest amount. Never, in the civilised world, are people asked to pay hundreds of thousands of pounds to be a guinea pig. Dorothy Bishop has written about The Weird World of US ethics regulation.
There is nothing new about this. The Cancerbusters site won the Anus Maximus Award for the year 2000. The award was announced in the following words:
The top award this year goes to the acolytes of Dr Stanislaw Burzynski who have created an advertising site at www.cancerbusters.com using a five-year-old boy named Thomas Navarro. Thomas is dying of cancer and this site exploits that tragedy to try and get the law changed so that quacks can have the untrammelled right to deceive desperate, sick people by promising them magic cures for cancer, AIDS and other diseases for which no cure is yet available. While this site is specifically a Burzynski promotion, his competitors support the site and mention it because if the campaign is successful it will dramatically increase the size of the market for quackery and therefore their opportunities to make money. [The boy died in November 2001]
The letters sent to Andrew Lewis are unspeakably nasty. They come from someone who calls himself "Marc Stephens" who claims to represent the company.
|
Le Canard Noir / Andy Lewis, I represent the Burzynski Clinic, Burzynski Research Institute, and Dr. Stanislaw Burzynski. It has been brought to our attention that you have content on your websites http://www.quackometer.net/blog/2011/11/the-false-hope-of-the-burzynski-clinic.html that is in violation of multiple laws. Please allow this correspondence to serve as notice to you that you published libelous and defamatory information. This correspondence constitutes a demand that you immediately cease and desist in your actions defaming and libeling my clients. Please be advised that my clients consider the content of your posting to be legally actionable under numerous legal causes of action, including but not limited to: defamation Libel, defamation per se, and tortious interference with business contracts and business relationships. The information you assert in your article is factually incorrect, and posted with either actual knowledge, or reckless disregard for its falsity. The various terms you use in your article connote dishonesty, untrustworthiness, illegality, and fraud. You, maliciously with the intent to harm my clients and to destroy his business, state information which is wholly without support, and which damages my clients’ reputations in the community. The purpose of your posting is to create in the public the belief that my clients are disreputable, are engaged in on-going criminal activity, and must be avoided by the public. You have a right to freedom of speech, and you have a right to voice your opinion, but you do not have the right to post libelous statements regardless if you think its your opinion or not. You are highly aware of defamation laws. You actually wrote an article about defamation on your site. In addition, I have information linking you to a network of individuals that disseminate false information. So the courts will apparently see the context of your article, and your act as Malicious. You have multiple third parties that viewed and commented on your article, which clearly makes this matter defamation libel. Once I obtain a subpoena for your personal information, I will not settle this case with you. Shut the article down IMMEDIATELY. GOVERN YOURSELF ACCORDINGLY. Regards, Marc Stephens |
Then later, at the end of another “foam-flecked angry rant”
|
. . . If you had no history of lying, and if you were not apart of a fraud network I would take the time to explain your article word for word, but you already know what defamation is. I’ve already recorded all of your articles from previous years as well as legal notice sent by other attorneys for different matters. As I mentioned, I am not playing games with you. You have a history of being stubborn which will play right into my hands. Be smart and considerate for your family and new child, and shut the article down..Immediately. FINAL WARNING. Regards, Marc Stephens |
Despite the attempt at legal style, "Marc Stephens" is not registered as an attorney in Texas.
Andy Lewis did not yield to this crude bullying. His post is still there for all to read. Before the days of the internet he would have been on his own. But now already dozens of blogs have drawn attention to what’s going on. Soon it will be hundreds. Burzynski can’t sue all of us. It’s the Streisand effect, or the "I am Spartacus" response.
Come on. Marc Stephens, make my day.
Some notes on the science
The Burzynski treatment is piss. Literally. A mixture of substances extracted from the patient’s own urine is dubbed with the preoposterous pseudoscientific name "antineoplastons". There are no such things as "neoplastons". And the chemicals are now made in the lab like any other drug.
|
The main component seems to be a simple organic chemical, phenylacetic acid (PA). It is produced in normal metabolism but the liver copes with it by converting it to phenylacetyl glutamine (PAG), which is excreted in the urine.
|

|
Saul Green has summarised the evidence
Burzynski has never demonstrated that A-2.1 (PA) or “soluble A-10” (PA and PAG) are effective against cancer or that tumor cells from patients treated with these antineoplastons have been “normalized.” Tests of antineoplastons at the National Cancer Institute have never been positive. The drug company Sigma-Tau Pharmaceuticals could not duplicate Burzynski’s claims for AS-2.1 and A-10. The Japanese National Cancer Institute has reported that antineoplastons did not work in their studies. No Burzynski coauthors have endorsed his use of antineoplastons in cancer patients.
Cancer Research UK has a summary of the current evidence, Hope or false hope?
Despite it being illegal to advertise cancer cures in most country, the list of people who flout the law to make money from the desperate is enormous/ You can find a list of them at Quackwatch. Burzynski isn’t the only one but he could well be the most expensive.
Latest developments
You can follow the ever-growing list of publications by people who are determined to resist Burzynski at Josephine Jones "Stanislaw, Streisand and Spartacus". There is also a list at anarchic_teapot’s blog
Follow-up
Saturday 26 November Another frothy threat from Burzynski’s alleged representative. Lot’s of RED ARROWS.
Monday 28 November The Streisand effect is developing rapidly. The definitive lists of posts are here and here. But there are two that I must mention.
Today Rhys Morgan has published Threats from The Burzynski Clinic. The same “Marc Stephens” has made the same sort of threats against him as he made against Lewis. Rhys Morgan is still at school, and is now 17 years old. He was the hero of the MMS scandal.
David Gorski, a real oncologist, has gone into the evidence in excellent detall with Stanislaw Burzynski: Bad medicine, a bad movie, and bad P.R.
Almost all the revelations about what’s taught on university courses in alternative medicine have come from post-1992 universities. (For readers not in the UK, post-1992 universities are the many new univerities created in 1992, from former polytechnics etc, and Russell group universities are the "top 20" research-intensive universities)
It is true that all the undergraduate courses are in post-1992 universities, but the advance of quackademia is by no means limited to them. The teaching at St Bartholomew’s Hospital Medical School, one of the oldest, was pretty disgraceful for example, though after protests from their own students, and from me, it is now better, I believe.

Quackery creeps into all universities to varying extents. The good ones (like Southampton) don’t run "BSc" degrees, but it still infiltrates through two main sources,
The first is via their HR departments, which are run by people who tend to be (I quote) "credulous and moronic" when it comes to science.
The other main source is in teaching to medical students. The General Medical Council says that medical students must know something about alterantive medicine and that’s quite right, A lot of their patients will use it. The problem is that the guidance is shockingly vague .
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
In many medical schools, the information that medical students get is quite accurate. At UCL and at King’s (London) I have done some of the familiarisation myself. In other good medical schools, the students get some shocking stuff. St Bartholomew’s Hospital medical School was one example. Edinburgh University was another.
But there is one Russell group university where alternative myths are propagated more than any other that I know about. That is the University of Southampton.
In general, Southampton is a good place, I worked there for three years myself (1972 – 1975). The very first noise spectra I measured were calculated on a PDP computer in their excellent Institute of Sound and Vibration Research, before I wrote my own programs to do it.
But Southanpton also has a The Complementary and Integrated Medicine Research Unit . Oddly the unit’s web site, http://www.cam-research-group.co.uk, is not a university address, and a search of the university’s web site for “Complementary and Integrated Medicine Research Unit” produces no result. Nevertheless the unit is “within the School of Medicine at the University of Southampton”
Notice the usual euphemisms ‘complementary’ and ‘integrated’ in the title: the word ‘alternative’ is never used. This sort of word play is part of the bait and switch approach of alternative medicine.
The unit is quite big: ten research staff, four PhD students and two support staff It is headed by George Lewith.
Teaching about alternative medicine to Southampton medical students.
The whole medical class seems to get quite a lot compared with other places I know about. That’s 250 students (210 on the 5-year course plus another 40 from the 4-year graduate-entry route).
Year 1: Lecture by David Owen on ‘holism’ within the Foundation Course given to all 210 medical students doing the standard (5-year) course.
Year 2: Lecture by Lewith (on complementary medicine, focusing on acupuncture for pain) given within the nervous systems course to the whole medical student year-group (210 students).
Year 3 SBOM (scientific basis of medicine) symposium: The 3-hour session (“Complementary or Alternative Medicine: You Decide”). I’m told that attendance at this symposium is often pretty low, but many do turn up and all of them are officially ‘expected’ to attend.
There is also an optional CAM special study module chosen by 20 students in year 3, but also a small number of medical students (perhaps 2 – 3 each year?) choose to do a BMedSci research project supervised by the CAM research group and involving 16-18 weeks of study from October to May in Year 4. The CAM research group also supervise postgraduate students doing PhD research.
As always, a list of lectures doesn’t tell you much. What we need to know is what’s taught to the students and something about the people who teach it. The other interesting question is how it comes about that alternative medicine has been allowed to become so prominent in a Russell group university. It must have support from on high. In this case it isn’t hard to find out where it comes from. Here are some details.
Year 1 Dr David Owen
David Owen is not part of Lewith’s group, but a member of the Division of Medical Education headed by Dr Faith Hill (of whom, more below). He’s one of the many part-time academics in this area, being also a founder of The Natural Practice .
Owen is an advocate of homeopathy (a past president of the Faculty of Homeopathy). Homeopathy is, of course, the most barmy and discredited of all the popular sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes it).
And he’s also a member of the British Society of Environmental Medicine (BSEM). That sounds like a very respectable title, but don’t be deceived. It is an organisation that promotes all sorts of seriously fringe ideas. All you have to do is notice that the star speaker at their 2011 conference was none other than used-to-be a doctor, Andrew Wakefield, a man who has been responsible for the death of children from measles by causing an unfounded scare about vaccination on the basis of data that turned out to have been falsified. There is still a letter of support for Wakefield on the BSEM web site.
The BSEM specialises in exaggerated claims about ‘environmental toxins’ and uses phony allergy tests like kinesiology and the Vega test that misdiagnose allergies, but provide en excuse to prescribe expensive but unproven nutritional supplements, or expensive psychobabble like "neuro-linguistic programming".
Other registered "ecological physicians" include the infamous Dr Sarah Myhill, who, in 2010, was the subject of a damning verdict by the GMC, and Southampton’s George Lewith.
If it is wrong to expose medical students to someone who believes that dose-response curves have a negative slope (the smaller the dose the bigger the effect -I know, it’s crazy), then it is downright wicked to expose students to a supporter of Andrew Wakefield.
David Owen’s appearance on Radio Oxford, with the indomitable Andy Lewis appears on his Quackometer blog.
Year 2 Dr George Lewith
Lewith is a mystery wrapped in an enigma. He’s participated in some research that is quite good by the (generally pathetic) standards of the world of alternative medicine.
In 2001 he showed that the Vega test did not work as a method of allergy diagnosis. "Conclusion Electrodermal testing cannot be used to diagnose environmental allergies", published in the BMJ .[download reprint].
In 2003 he published "A randomized, double-blind, placebo-controlled proving trial of Belladonna 30C” [download reprint] that showed homeopathic pills with no active ingredients had no effects: The conclusion was "”Ultramolecular homeopathy has no observable clinical effects" (the word ultramolecular, in this context, means that the belladonna pills contained no belladonna).
In 2010 he again concluded that homeopathic pills were no more than placebos, as described in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). [download reprint]
What i cannot understand is that, despite his own findings, his private practice continues to prescribe the Vega machine and continues to prescribe homeopathic pills. And he continues to preach this subject to unfortunate medical students.
Lewith is also one of the practitioners recommended by BSEM. He’s a director of the "College of Medicine". And he’s also an advisor to a charity called Yes To Life. (see A thoroughly dangerous charity: YesToLife promotes nonsense cancer treatments).
3rd year Student Selected Unit
The teaching team includes:
- David Owen – Principal Clinical Teaching Fellow SoM, Holistic Physician
- George Lewith – Professor of Health Research and Consultant Physician
- Caroline Eyles – Homeopathic Physician
- Susan Woodhead – Acupuncturist
- Elaine Cooke – Chiropractic Practitioner
- Phine Dahle – Psychotherapist
- Keith Carr – Reiki Master
- Christine Rose – Homeopath and GP
- David Nicolson – Nutritionalist
- Shelley Baker – Aromatherapist
- Cheryl Dunford – Hypnotherapist
- Dedj Leibbrandt – Herbalist
More details of the teaching team here. There is not a single sceptic among them, so the students don’t get a debate, just propaganda.
In this case. there’s no need for the Freedom of Information Act. The handouts. and the powerpoints are on their web site. They seem to be proud of them
Let’s look at some examples
Chiropractic makes an interesting case, because, in the wake of the Singh-BCA libel case, the claims of chiropractors have been scrutinised as never before and most of their claims have turned out to be bogus. There is a close relationship between Lewith’s unit and the Anglo-European Chiropractic College (the 3rd year module includes a visit there). In fact the handout provided for students, Evidence for Chiropractic Care , was written by the College. It’s interesting because it provides no real evidence whatsoever for the effectiveness of chiropractic care. It’s fairly honest in stating that the view at present is that, for low back pain, it isn’t possible to detect any difference between the usefulness of manipulation by a physiotherapist, by an osteopath or by a chiropractor. Of course it does not draw the obvious conclusion that this makes chiropractic and osteopathy entirely redundant -you can get the same result without all the absurd mumbo jumbo that chiropractors and osteopaths love, or their high-pressure salesmanship and superfluous X-rays. Neither does it mention the sad, but entirely possible, outcome that none of the manipulations are effective for low back pain. There is, for example, no mention of the fascinating paper by Artus et al [download reprint]. This paper concludes
"symptoms seem to improve in a similar pattern in clinical trials following a wide
variety of active as well as inactive treatments."
This paper was brought to my attention through the blog run by the exellent physiotherapist, Neil O’Connell. He comments
“If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery.”
This sort of critical thinking is conspicuously absent from this (and all the other) Southampton handouts. The handout is a superb example of bait and switch: No nonsense about infant colic, innate energy or imaginary subluxations appears in it.
Acupuncture is another interesting case because there is quite a lot of research evidence, in stark contrast to the rest of traditional Chinese medicine, for which there is very little research.
|
There is a powerpoint show by Susan Woodhead (though it is labelled British Acupuncture Council). The message is simple and totally uncritical. It works. |

|
In fact there is now a broad consensus about acupuncture.
(1) Real acupuncture and sham acupuncture have been found to be indistinguishable in many trials. This is the case regardless of whether the sham is a retractable needle (or even a toothpick) in the "right" places, or whether it is real needles inserted in the "wrong" places. The latter finding shows clearly that all that stuff about meridians and flow of Qi is sheer hocus pocus. It dates from a pre-scientific age and it was wrong.
(2) A non-blind comparison of acupuncture versus no acupuncture shows an advantage for acupuncture. But the advantage is usually too small to be of any clinical significance. In all probability it is a placebo effect -it’s hard to imagine a more theatrical event than having someone in a white coat stick long needles into you, like a voodoo doll. Sadly, the placebo effect isn’t big enough to be of much use.
Needless to say, none of this is conveyed to the medical students of Southampton. Instead they are shown crude ancient ideas that date from long before anything was known about physiology as though they were actually true. These folks truly live in some alternative universe. Here are some samples from the acupuncture powerpoint show by Susan Woodhead.



Well this is certainly a "different diagnostic language", but no attempt is made to say which one is right. In the mind of the acupuncurist it seems both are true. It is a characteristic of alternative medicine advocates that they have no difficulty in believing simultaneously several mutually contradictory propositions.
As a final exmple of barminess, just look at the acupuncture points (allegedly) on the ear The fact that it is a favoured by some people in the Pentagon as battlefield acupuncture, is more reminiscent of the mad general, Jack D. Ripper, in Dr Strangelove than it is of science.

There is an equally uncritical handout on acupuncture by Val Hopwood. It’s dated March 2003, a time before some of the most valuable experiments were done.
The handout says "sham acupuncture
is generally less effective than true acupuncture", precisely the opposite of what’s known now. And there are some bits that give you a good laugh, always helpful in teaching. I like
“There is little doubt that an intact functioning nervous system is required for acupuncture to produce
analgesia or, for that matter, any physiological changes”
and
Modern techniques: These include hybrid techniques such as electro-acupuncture . . . and Ryadoraku [sic] therapy and Vega testing.
Vega testing!! That’s been disproved dozens of times (not least by George Lewith). And actually the other made-up nonsense is spelled Ryodoraku.
It’s true that there is a short paragraph at the end of the handout headed "Scientific evaluation of acupuncture" but it doesn’t cite a single reference and reads more like excuses for why acupuncture so often fails when it’s tested properly.
Homeopathy. Finally a bit about that most boring of topics, the laughable medicine that contains no medicine, homeopathy. Caroline Eyles is a member for the Society of Homeopaths, the organisation that did nothing when its members were caught out in the murderous practice of recommending homeopathy for prevention of malaria. The Society of Homeopaths also endorses Jeremy Sherr, a man so crazy that he believes he can cure AIDS and malaria with sugar pills.
The homeopathy handout given to the students has 367 references, but somehow manages to omit the references to their own boss’s work showing that the pills are placebos. The handout has all the sciencey-sounding words, abused by people who don’t understand them.
"The remedy will be particularly effective if matched to the specific/particular characteristics of the individual (the ‘totality’ of the patient) on all levels, including the emotional and mental levels, as well as just the physical symptoms. ‘Resonance’ with the remedy’s curative power will then be at it’s [sic] best."
The handout is totally misleading about the current state of research. It says
"increasing clinical research confirms it’s [sic] clinical effectiveness in treating patients, including babies and animals (where a placebo effect would be hard to justify)."
|
The powerpont show by Caroline Eyles shows all the insight of a mediaeval vitalist |
|
Anyone who has to rely on the utterly discredited Jacques Benveniste as evidence is clearly clutching at straws. What’s more interesting about this slide the admission that "reproducibility is a problem -oops, an issue" and that RCTs (done largely by homeopaths of course) have "various methodological flaws and poor external validity". You’d think that if that was the best that could be produced after 200 yours, they’d shut up shop and get another job. But, like aging vicars who long since stopped believing in god, but are damned if they’ll give up the nice country rectory, they struggle on, sounding increasingly desperate.
How have topics like this become so embedded in a medical course at a Russell group university?
The details above are a bit tedious and repetitive. It’s already established that hardly any alternative medicine works. Don’t take my word for it. Check the web site of the US National Center for Complementary and Alternative Medicine (NCCAM) who, at a cost of over $2 billion have produced nothing useful.
A rather more interesting question is how a good university like Southampton comes to be exposing its medical students to teaching like this. There must be some powerful allies higher up in the university. In this case it’s pretty obvious who thay are.
Professor Stephen Holgate MD DSc CSc FRCP FRCPath FIBiol FBMS FMed Sci CBE has to be the primary suspect, He’s listed as one of Southampton’s Outstanding Academics. His work is nothing to do with alternative medicine but he’s been a long term supporter of the late unlamented Prince of Wales’ Foundation, and he’s now on the advisory board of it’s successor, the so called "College of Medicine" (for more information about that place see the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health, and also Don’t be deceived. The new “College of Medicine” is a fraud and delusion ). His description on that site reads thus.
"Stephen Holgate is MRC Clinical Professor of Immunopharmacology at the University of Southampton School of Medicine and Honorary Consultant Physician at Southampton University Hospital Trust. He is also chair of the MRC’s Populations and Systems Medicine Board. Specialising in respiratory medicine, he is the author of over 800 peer-reviewed papers and contributions to scientific journals and editor of major textbooks on asthma and rhinitis. He is Co-Editor of Clinical and Experimental Allergy, Associate Editor of Clinical Science and on the editorial board of 25 other scientific journals."
Clearly a busy man. Personally I’m deeply suspicious of anyone who claims to be the author of over 800 papers. He graduated in medicine in 1971, so that is an average of over 20 papers a year since then, one every two or three weeks. I’d have trouble reading that many, never mind writing them.
Holgate’s long-standing interest in alternative medicine is baffling. He’s published on the topic with George Lewith, who, incidentally, is one of the directors of the "College of Medicine"..
It may be unkind to mention that, for many years now, I’ve been hearing rumours that Holgate is suffering from an unusually bad case of Knight starvation.
The Division of Medical Education appears to be the other big source of support for. anti-scientific medicine. That is very odd, I know, but it was also the medical education people who were responsible for mis-educating medical students at. St. Bartholomew’s and at Edinburgh university. Southampton’s Division of Medical Education has a mind-boggling 60 academic and support staff. Two of them are of particular interest here.
Faith Hill is director of the division. Her profile doesn’t say anything about alternative medicine, but her interest is clear from a 2003 paper, Complementary and alternative medicine: the next generation of health promotion?. The research consisted of reporting anecdotes from interviews of 52 unnamed people (this sort of thing seems to pass for research in the social sciences). It starts badly by misrepresenting the conclusions of the House of Lords report (2000) on CAM. Although it comes to no useful conclusions, it certainly shows a high tolerance of nonsensical treatments.
Chris Stephens is Associate Dean of Medical Education & Student Experience. His sympathy is shown by a paper he wrote In 2001, with David Owen (the homeopath, above) and George Lewith: Can doctors respond to patients’ increasing interest in complementary and alternative medicine?. Two of the conclusions of this paper were as follows.
"Doctors are training in complementary and alternative medicine and report benefits both for their patients and themselves"
Well, no actually. It wasn’t true then, and it’s probably even less true now. There’s now a lot more evidence and most of it shows alternative medicine doesn’t work.
"Doctors need to address training in and practice of complementary and alternative medicine within their own organisations"
Yes they certainly need to do that.
And the first thing that Drs Hill and Stephens should do is look a bit more closely about what’s taught in their own university, I hope that this post helps them,
Follow-up
4 July 2011. A correspondent has just pointed out that Chris Stephens is a member of the General Chiropractic Council. The GCC is a truly pathetic pseudo-regulator. In the wake of the Simon Singh affair it has been kept busy fending off well-justified complaints against untrue claims made by chiropractors. The GCC is a sad joke, but it’s even sadder to see a Dean of Medical Education at the University of Southampton being involved with an organisation that has treated little matters of truth with such disdain.
A rather unkind tweet from (ex)-chiropractor @RichardLanigan.
“Chris is just another light weight academic who likes being on committees. Regulatory bodies are full of them”
The Atlantic is an American magazine founded (as The Atlantic Monthly) in Boston, Massachusetts, in 1857. It is a literary and cultural magazine with a very distinguished history. Its contributors include Mark Twain and Martin Luther King. So it was pretty exciting to be asked to write something for it, even with a 12 hour deadline.

Sadly though, in recent years, the coverage of science in The Atlantic has been less than good The inimitable David Gorski has explained the problem in Blatant pro-alternative medicine propaganda in The Atlantic. The immediate cause of the kerfuffle was the publication of an article, The Triumph of New-Age Medicine. It was written by a journalist, David Freedman. It is very long and really not very good. It has been deconstructed also by Steven Novella.
Freedman’s article is very long, but it boils down to saying I know it doesn’t work but isn’t it nice. The article was followed up with Fix or Fraud: a ‘debate’., The debate is rather disappointing. It suffers from the problem, not unknown at the BBC, of thinking that ‘balance’ means giving equal time to people who think the earth is flat as it gives to people who think it is a oblate spheroid. The debate consists of 800 word contributions from seven people, six of whom are flat earthers, and one of which is very good. Try Steven Salzberg, A ‘triumph’ of hype over reality for some real sense. One of the flat earthers is director of a National Institutes of Health institute, NCCAM.
And this is a magazine that published not only Mark Twain, but Abraham Flexner, the man who, in 1910, put US medical education on a firm scientific footing, You can read Flexner in their archive. Mark Twain said
[A reply to letters recommending remedies]:
Dear Sir (or Madam):–I try every remedy sent to me. I am now on No. 67. Yours is 2,653. I am looking forward to its beneficial results. – quoted in My Father Mark Twain, by Clara Clemens
"allopathy is good for the sane and homeopathy for the insane"
So here is the piece, produced rather rapidly, for the debate. This is the original unedited version, slightly longer than appears in The Atlantic.
The title for The Atlantic piece, America, Land of the Health Hucksters, was theirs not mine. There is no shortage of health hucksters in the UK. but at least they mostly haven’t become as embedded within univerities and hospitals as much as in the USA.
|
David Freeman’s article, “The Triumph of New Age Medicine” starts by admitting that most alternative treatments don’t work, and ends by recommending them. He takes a lot more words to say it, but that seems a fair synopsis. It is the sort of thing you might expect in a cheap supermarket magazine, not in Atlantic. The article is a prime example of rather effective sales technique, much beloved of used car salesmen and health hucksters. It’s called bait and switch. It’s true that medicine can’t cure everything. That’s hardly surprising given that serious research has been going on for barely 100 years, and it turns out that the humans are quite complicated. But the answer to the limitations of medicine is not to invent fairy stories, which is what the alternative medicine industry does. There is no sensible option but to keep the research going and to test its results honestly. It’s sad but true that Big Pharma has at times corrupted medicine, by concealing negative results. But that corruption has been revealed by real scientists, not by health hucksters. In the end, science is self-correcting and the truth emerges. Health hucksters, on the other hand, seem incapable of giving up their beliefs whatever the evidence says. The idea of patient-centered care is fashionable and care is great, if you can’t cure. But there’s a whole spectrum in the wellbeing industry, from serious attempts to make people happier, to the downright nuts. The problem is that caring for patients make a very good bait, and the switch to woo tends to follow not far behind. I write from the perspective of someone who lives in a country that achieves health care for all its citizens at half the cost of the US system, and gets better outcomes in life expectancy and infant mortality. The view from outside is that US medicine rather resembles US religion. It has been taken over by fundamentalists who become very rich by persuading a gullible public to believe things that aren’t true. One of Freedman’s problems is, I think, that he vastly overestimates the power of the placebo effect. It exists, for sure, but in most cases, it seems to be small, erratic and transient. Acupuncture is a good example. It’s quite clear now that real acupuncture and sham acupuncture are indistinguishable, so it’s also quite clear that the ‘principles’ on which it’s based are simply hokum. If you do a non-blind comparison of acupuncture with no acupuncture, there is in some trials (not all) a small advantage for the acupuncture group. But it is too small to be of much benefit to the patient. By far the more important reason why ineffective voodoo like acupuncture appears to work is the “get better anyway” effect (known technically as regression to the mean). You take the needles or pills when you are at your worst, the next day you feel better. It’s natural to attribute the fact that you feel better to the needles or pills, when all you are seeing is natural fluctuations in the condition. It’s like Echinacea will cure your cold in only seven days when otherwise it would have taken a week. If the article itself was naïve and uncritical, the follow up was worse. It is rather surprising to me that a magazine like Atlantic should think it worth printing an advertorial for Andrew Weil’s business. Surely, though, Josephine Briggs, as director of an NIH institute is more serious? Sadly, no. Her piece is a masterpiece of clutching at straws. The fact is that her institute has spent over $ 2 billion of US taxpayers’ money and, for all that money it has produced not a single useful treatment. All that NCCAM has done is to show that several things do not work, something we pretty much knew already. If I were a US taxpayer, I’d be somewhat displeased by that. It should be shut down now. At first sight Dean Ornish sounds more respectable. He bases his arguments on diet and life style changes, which aren’t alternative at all. He’s done some research too. The problem is that it’s mostly preliminary and inconclusive research, on the basis of which he vastly exaggerates the strength of the evidence for what can be achieved by diet alone. It’s classical bait and switch again. The respectable, if ill-founded, arguments get you the foot in the door, and the woo follows later. This is all very sad for a country that realized quite early that the interests of patients were best served by using treatments that had been shown to work. The Flexner report of 1910 led the world in the rational education of physicians. But now even places like Yale and Harvard peddle snake oil to their students through their "integrative medicine" departments. It’s hard to see why the USA is in the vanguard of substituting wishful thinking for common sense and reason. The main reason, I’d guess, is money. Through NCCAM and the Bravewell Collaborative, large amounts of money have been thrown to the winds and businesses like Yale and Harvard have been quick to abandon their principles and grab the money. Another reason for the popularity of alternative medicine in parts of academia is that it’s a great deal easier to do ‘science’ when you are allowed to make up the answers. The "integrative medicine" symposium held at Yale in 2008 boggled the mind. Dr David Katz listed a lot of things he’d tried and which failed to work, His conclusion was not that they should be abandoned, but that we needed a "more fluid concept of evidence". You can see it on YouTube, Senator Tom Harkin’s promotion of NCCAM has done for the U.S. reputation in medicine what Dick Cheney did for the U.S. reputation in torture. It is hard to look at the USA from outside without thinking of the decline and fall of the Roman Empire. One had hoped that era was over with the election of Obama, but the hucksters won’t give up without a fight. They are making too much money to do that. |
Follow-up
The comments that appeared in The Atlantic on this piece were mostly less than enlightening -not quite what one expected of an intellectual magazine. Nevertheless I tried to answer all but the plain abusive comments.
More interesting, though, was an editorial by Jennie Rothenberg Gritz, the Atlantic Senior Editor who asked me to contribute. The Man Who Invented Medical School. It picked up on my mention of Abraham Flexner, and his famous 1910 report [download from Carnegie Foundation] which first put US medial education on a form rational footing. based on science. Now, 100 years later that’s being unpicked both in the USA and here. ms Gritz seemed to think that Flexner would have approved of Dean Ornish. In a response I begged to differ. I’m pretty sure that Felxner would have been furious of he could have seen the reecent march of quackademia, particularly, but not exclusively, in the USA. It is exactly the sort of thing his report set out, successfully, to abolish. He wrote, for example,
“the practitioner is subjected, year in, year out, to the steady bombardment of the unscrupulous manufacturer, persuasive to the uncritical, on the principle that “what I tell you three times is true.” Against bad example and persistent asseveration, only precise scientific concepts and a critical
appreciation of the nature and limits of actual demonstration can protect the young physician.” (Flexner report, 1910, pp 64-65)
It is this very “appreciation of the nature and limits of actual demonstration” that is now being abandoned by the alternative medicine industry. despite the fact that real medicine was in its infancy at the time he w as writing, he was very perceptive about the problems. Perhaps Freedman should read the report.
David Katz seems to have spotted my piece in The Atlantic, and has responded at great length in the Huffington Post (quite appropriate, given the consistent support of HuffPo for nonsense medicine). HuffPo allows only short comments with no links so I’ll reply to him here.
I fear that Dr Katz doth protest a great deal too much. He seems to object to a comment that I made about him in The Atlantic.
“… [He] listed a lot of things he’d tried and which failed to work. His conclusion was not that they should be abandoned, but that we needed a ‘a more fluid concept of evidence.'”
You don’t have to take my word for it. You can take it from the words of Dr Katz.
"What do we do when the evidence we have learned, or if we care to be more provocative, with which we have been indoctrinated, does now fully meet the needs of our patients"
It seems odd to me to regard teaching about how you distinguish what;s true and what isn’t as "indoctrination", though I can understand that knowledge of that subject could well diminish the income of alternative practitioners. You went on to say
"Some years ago the CDC funded us with a million dollars to do what they referred to initially as a systematic review of the evidence base for complementary and alternative medicine, Anybody who’s ever been involved in systematic reviews knows that’s a very silly thing. . . . Well we knew it was silly but a million dollars sounded real [mumbled] took the money and then we figurered we’d figure out what to do with it [smiles broadly]. That’s what we did ". . .
I do hope you told the CDC that you did not spend the million dollars for the sensible purpose for which it was awarded.
This infusion of calcium, magnesium and D vitamins and vitamin C ameliorates the symptoms of fibromyalgia. . . . We did typical placebo controlled randomized double-blind trial for several months . . . we saw an improvement in both our treatment and placebo groups . . .
You then describe how you tested yoga for asthma and homeopathy for attention deficit hyperactivity disorder, Neither of them worked either. Your reaction to this string of failures was just to say “we need a more fluid concept of evidence”
After telling an anecdote about one patient who got better after taking homeopathic treatment you said £I don’t care to get into a discussion of how, or even whether, homeopathy works”. Why not? It seems it doesn’t matter much to you whether the things you sell to patients work or not.
You then went on to describe quite accurately that anti-oxidants don’t work and neither do multivitamin supplements for prevention of cardiovascular problems, And once again you fail to accept the evidence, even evidence you have found yourself. Your response was
“So here too is an invitation to think more fluidly about of evidence. Absence of evidence is not evidence of absence.”
That last statement is the eternal cry of every quack. It’s true, of course, but that does not mean that absence of evidence gives you a licence to invent the answer. But inventing the answer is what you do, time after time, You seem quite incapable of saying the most important thing that anyone in your position should. I don’t know the answer.
This is a slightly-modified version of the article that appeared in BMJ blogs yesterday, but with more links to original sources, and a picture. There are already some comments in the BMJ.
The original article, diplomatically, did not link directly to UCL’s Grand Challenge of Human Wellbeing, a well-meaning initiative which, I suspect, will not prove to be value for money when it comes to practical action.
Neither, when referring to the bad effects of disempowerment on human wellbeing (as elucidated by, among others, UCL’s Michael Marmot), did I mention the several ways in which staff have been disempowered and rendered voiceless at UCL during the last five years. Although these actions have undoubtedly had a bad effect on the wellbeing of UCL’s staff, it seemed a litlle unfair to single out UCL since similar things are happening in most universities. Indeed the fact that it has been far worse at Imperial College (at least in medicine) has probably saved UCL from being denuded. One must be thankful for small mercies.
There is, i think, a lesson to be learned from the fact that formal initiatives in wellbeing are springing up at a time when university managers are set on taking actions that have exactly the opposite effect. A ‘change manager’ is not an adequate substitute for a vote. Who do they imagine is being fooled?
The A to Z of the wellbeing industry
From angelic reiki to patient-centred care
Nobody could possibly be against wellbeing. It would be like opposing motherhood and apple pie. There is a whole spectrum of activities under the wellbeing banner, from the undoubtedly well-meaning patient-centred care at one end, to downright barmy new-age claptrap at the other end. The only question that really matters is, how much of it works?
Let’s start at the fruitcake end of the spectrum.
One thing is obvious. Wellbeing is big business. And if it is no more than a branch of the multi-billion-dollar positive-thinking industry, save your money and get on with your life.
In June 2010, Northamptonshire NHS Foundation Trust sponsored a “Festival of Wellbeing” that included a complementary therapy taster day. In a BBC interview one practitioner used the advertising opportunity, paid for by the NHS, to say “I’m an angelic reiki master teacher and also an angel therapist.” “Angels are just flying spirits, 100 percent just pure light from heaven. They are all around us. Everybody has a guardian angel.” Another said “I am a member of the British Society of Dowsers and use a crystal pendulum to dowse in treatment sessions. Sessions may include a combination of meditation, colour breathing, crystals, colour scarves, and use of a light box.” You couldn’t make it up.
The enormous positive-thinking industry is no better. Barbara Ehrenreich’s book, Smile Or Die: How Positive Thinking Fooled America and the World, explains how dangerous the industry is, because, as much as guardian angels, it is based on myth and delusion. It simply doesn’t work (except for those who make fortunes by promoting it). She argues that it fosters the sort of delusion that gave us the financial crisis (and pessimistic bankers were fired for being right). Her interest in the industry started when she was diagnosed with cancer. She says
”When I was diagnosed, what I found was constant exhortations to be positive, to be cheerful, to even embrace the disease as if it were a gift. If that’s a gift, take me off your Christmas list,”
It is quite clear that positive thinking does nothing whatsoever to prolong your life (Schofield et al 2004; Coyne et al 2007; 2,3), any more than it will cure tuberculosis or cholera. “Encouraging patients to “be positive” only may add to the burden of having cancer while providing little benefit” (Schofield et al 2004). Far from being helpful, it can be rather cruel.
Just about every government department, the NHS, BIS, HEFCE, and NICE, has produced long reports on wellbeing and stress at work. It’s well known that income is correlated strongly with health (Marmot, M., 2004). For every tube stop you go east of Westminster you lose a year of life expectancy (London Health Observatory). It’s been proposed that what matters is inequality of income (Wilkinson & Pickett, 2009). The nature of the evidence doesn’t allow such a firm conclusion (Lynch et al. 2004), but that isn’t really the point. The real problem is that nobody has come up with good solutions. Sadly the recommendations at the ends of all these reports don’t amount to a hill of beans. Nobody knows what to do, partly because pilot studies are rarely randomised so causality is always dubious, and partly because the obvious steps are either managerially inconvenient, ideologically unacceptable, or too expensive.
Take two examples:
Sir Michael Marmot’s famous Whitehall study (Marmot, M., 2004) has shown that a major correlate of illness is lack of control over one’s own fate: disempowerment. What has been done about it?
In universities it has proved useful to managers to increase centralisation and to disempower academics, precisely the opposite of what Marmot recommends.
|
As long as it’s convenient to managers they are not going to change policy. Rather, they hand the job to the HR department which appoints highly paid “change managers,” who add to the stress by sending you stupid graphs that show you emerging from the slough of despond into eternal light once you realise that you really wanted to be disempowered after all. Or they send you on some silly “resilience” course. |
|
A second example comes from debt. According to a BIS report (Mental Capital and Wellbeing), debt is an even stronger risk factor for mental disorder than low income. So what is the government’s response to that? To treble tuition fees to ensure that almost all graduates will stay in debt for most of their lifetime. And this was done despite the fact that the £9k fees will save nothing for the taxpayer: in fact they’ll cost more than the £3k fees. The rise has happened, presumably, because the ideological reasons overrode the government’s own ideas on how to make people happy.
Nothing illustrates better the futility of the wellbeing industry than the response that is reported to have been given to a reporter who posed as an applicant for a “health, safety, and wellbeing adviser” with a local council. When he asked what “wellbeing” advice would involve, a member of the council’s human resources team said: “We are not really sure yet as we have only just added that to the role. We’ll want someone to make sure that staff take breaks, go for walks — that kind of stuff.”
The latest wellbeing notion to re-emerge is the happiness survey. Jeremy Bentham advocated “the greatest happiness for the greatest number,” but neglected to say how you measure it. A YouGov poll asks, “what about your general well-being right now, on a scale from 1 to 10.” I have not the slightest idea about how to answer such a question. As always some things are good, some are bad, and anyway wellbeing relative to whom? Writing this is fun. Trying to solve an algebraic problem is fun. Constant battling with university management in order to be able to do these things is not fun. The whole exercise smacks of the sort of intellectual arrogance that led psychologists in the 1930s to claim that they could sum up a person’s intelligence in a single number. That claim was wrong and it did great social harm.
HEFCE has spent a large amount of money setting up “pilot studies” of wellbeing in nine universities. Only one is randomised, so there will be no evidence for causality. The design of the pilots is contracted to a private company, Robertson Cooper, which declines to give full details but it seems likely that the results will be about as useless as the notorious Durham fish oil “trials”(Goldacre, 2008).
Lastly we get to the sensible end of the spectrum: patient-centred care. Again this has turned into an industry with endless meetings and reports and very few conclusions. Epstein & Street (2011) say
“Helping patients to be more active in consultations changes centuries of physician-dominated dialogues to those that engage patients as active participants. Training physicians to be more mindful, informative, and empathic transforms their role from one characterized by authority to one that has the goals of partnership, solidarity, empathy, and collaboration.”
That’s fine, but the question that is constantly avoided is what happens when a patient with metastatic breast cancer expresses a strong preference for Vitamin C or Gerson therapy, as advocated by the YesToLife charity. The fact of the matter is that the relationship can’t be equal when one party, usually (but not invariably) the doctor, knows a lot more about the problem than the other.
What really matters above all to patients is getting better. Anyone in their right mind would prefer a grumpy condescending doctor who correctly diagnoses their tumour, to an empathetic doctor who misses it. It’s fine for medical students to learn social skills but there is a real danger of so much time being spent on it that they can no longer make a correct diagnosis. Put another way, there is confusion between caring and curing. It is curing that matters most to patients. It is this confusion that forms the basis of the bait and switch tactics (see also here) used by magic medicine advocates to gain the respectability that they crave but rarely deserve.
If, as is only too often the case, the patient can’t be cured, then certainly they should be cared for. That’s a moral obligation when medicine fails in its primary aim. There is a lot of talk about individualised care. It is a buzzword of quacks and also of the libertarian wing which says NICE is too prescriptive. It sounds great, but it helps only if the individualised treatment actually works.
Nobody knows how often medicine fails to be “patient-centred.”. Even less does anyone know whether patient-centred care can improve the actual health of patients. There is a strong tendency to do small pilot trials that are as likely to mislead as inform. One properly randomised trial (Kinmonth et al., 1998) concluded
“those committed to achieving the benefits of patient centred consulting should not lose the focus on disease management.”
Non-randomised studies may produce more optimistic conclusions (e.g. Hojat et al, 2011), but there is no way to tell if this is simply because doctors find it easy to be empathetic with patients who have better outcomes.
Obviously I’m in favour of doctors being nice to patients and to listening to their wishes. But there is a real danger that it will be seen as more important than curing. There is also a real danger that it will open the doors to all sorts of quacks who claim to provide individualised empathic treatment, but end up recommending Gerson therapy for metastatic breast cancer. The new College of Medicine, which in reality is simply a reincarnation of the late unlamented Prince’s Foundation for Integrated Health, lists as its founder Capita, the private healthcare provider that will, no doubt, be happy to back the herbalists and homeopaths in the College of Medicine, and, no doubt, to make a profit from selling their wares to the NHS.
In my own experience as a patient, there is not nearly as much of a problem with patient centred care as the industry makes out. Others have been less lucky, as shown by the mid-Staffordshire disaster (Delamothe, 2010), That seems to have resulted from PR being given priority over patients. Perhaps all that’s needed is to save money on all the endless reports and meetings (“the best substitute for work”), ban use of PR agencies (paid lying) and to spend the money on more doctors and nurses so they can give time to people who need it. This is a job that will be hindered considerably by the government’s proposals to sell off NHS work to private providers who will be happy to make money from junk medicine.
Reference
Wilkinson. R & Pickett, K. 2009 , The Spirit Level, ISBN 978 1 84614 039 6
A footnote on Robertson Cooper and "resilience"
I took up the offer of Robertson Cooper to do their free "resilience" assessment, the company to which HEFCE has paid an undisclosed amount of money.

The first problem arose when it asked about your job. There was no option for scientist, mathematician, university or research, so I was forced to choose "education and training". (a funny juxtaposition since training is arguably the antithesis of education). It had 195 questions. mostly as unanswerable as in the YouGov happiness survey. I particularly liked question 124 "I see little point in many of the theoretical models I come across". The theoretical models that I come across most are Markov models for the intramolecular changes in a receptor molecule when it binds a ligand (try, for example, Joint distributions of apparent open and shut times of single-ion channels and maximum likelihood fitting of mechanisms). I doubt the person who wrote the question has ever heard of a model of that sort. The answer to that question (and most of the others) would not be worth the paper they are written on.
The whole exercise struck me as the worst sort of vacuous HR psychobabble. It is worrying that HEFCE thinks it is worth spending money on it.
Follow-up
I’m bored stiff with that barmiest of all the widespread forms of alternative medicine, homeopathy. It is clearly heading back to where it was in 1960, a small lunatic fringe of medicine. Nevertheless it’s worth looking at a recent development.
A paper has appeared by that arch defender of all things alternative, George Lewith.
The paper in question is “Homeopathy has clinical benefits in rheumatoid arthritis patients that are attributable to the
consultation process but not the homeopathic remedy: a randomized controlled clinical trial”, Sarah Brien, Laurie Lachance, Phil Prescott, Clare McDermott and George Lewith. [read it here]. It was published in Rheumatology.
Conclusion. Homeopathic consultations but not homeopathic remedies are associated with clinically relevant benefits for patients with active but relatively stable RA.
So yet another case where the homeopathic pills turn out the same as placebos, Hardly surprising since the pills are the same as the placebos, but it’s always good to hear it from someone whose private practice sells homeopathy for money.
The conclusion isn’t actually very novel, because Fisher & Scott (2001) had already found nine years ago that homeopathy was ineffective in reducing the symptoms if joint inflammation in RA. That is Peter Fisher, the Queens’ homeopathic physician, and Clinical Director of the Royal Hospital for Integrated Medicine (recently renamed to remove ‘homeopathy’ from its title). That paper ends with the remarkable statement [download the paper]
- "Over these years we have come to believe that conventional RCTs [randomised controlled trials] are unlikely to capture the possible benefits of homeopathy . . . . It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response."
That seemed to me at the time to amount to an admission that it was all ‘placebo effect’, though Fisher continues to deny that this is the case.
"Homeopathy has clinical benefits in rheumatoid arthritis patients" -the title says. But does it?
In fact this is mere spin. What the paper actually shows is that an empathetic consultation has some benefit (and even this is inconsistent). This is hardly surprising, but there is really not the slightest reason to suppose that the benefit, such as it is, has anything whatsoever to do with homeopathy.
Homeopathy, non-specific effects and good medicine is the title of an excellent editorial, in the same issue of Rheumatology, by Edzard Ernst. He points out that "The recognition of the therapeutic value of an empathetic consultation is by no means a new insight". Any therapy that provides only non-specific effects is unacceptable. Any good doctor provides that and, when it exists, real effective treatments too.
Lewith’s private clinic

The Centre for Complementary and Integrated Medicine is run by Drs Nick Avery and George Lewith. It is always a bit galling to real scientists, who often work 60 hours a week or more to get results, that people like Lewith get a professorial salary (in his case from the University of Southampton) but still have time to make more money by doing another job at the same time.
Avery is a homeopath. I wonder whether we can now look forward to the web site being changed in the near future so that there is a clear statement that the pills have no effect?
There is, at least, now no longer any mention of the Vega test on Lewith’s site. That is a test for food allergy that has been shown again and again to be fraudulent. The Environmental medicine page is brief, and avoids making any claims at all. It now contains the somewhat coy statement
“Specific food avoidance regimes are a controversial area and one in which there may be conflict between conventionally trained allergists and CAM practitioners.”
However the page about fibromyalgia still mentions homeopathy favourably. And it still fails to refer to my reanalysis of one of the positive trials which revealed a simple statistical mistake.
The front page of their web site boasts that "Dr George Lewith is now one of The Lifestyle 50!". " The Times, in an article on September 6th 2008, included George Lewith in The Lifestyle 50, this newspaper’s listing of the “top 50 people who influence the way we eat, exercise and think about ourselves”. Dr Lewith is included in the Alternatives category". It doesn’t mention that this is an honour he shares with such medical luminaries as Gillian ("I’m not a doctor") McKeith, Jennifer Ariston and the Pope,
But let’s end this on a happier note. There is one thing that I agree with wholeheartedly. Lewith says
"The use of bottled water seems to me to be a multi-billion pound industry, based on some of the cleverest marketing that I have ever encountered. There is absolutely no evidence that bottled water is any safer, better, or more “energising” than the water you get from the tap."
No connection of course with the multi-million pound industry of selling homeopathic water by clever marketing.
Some limitations of the paper by Brien et al.
Like any good trial, this one defined in advance a primary and secondary outcome.
The primary outcome was ACR20. which means the propertion of patients that showed an improvement of at least 20% of the number of tender and swollen joint counts and 20% improvement in 3 of the 5 remaining ACR core set measures (see Felsen 1995). Although it isn’t stressed in the paper, there was no detectable difference between consultation vs no consultation for this primary outcome.
The secondary outcome was 28-joint DAS (DAS-28), tender and swollen joint count, disease severity, pain, weekly patient
and physician GA and pain, and inflammatory markers (see, for example, Stucki. 1996). It was only on this outcome that an effect was seen between consultation and no consultation. The "effect size" (standardized mean score differences, adjusted for baseline differences) was an improvement of 0.7 in DAS-28 score, which runs on a scale from 0 – 10. Although this improvement is probably real (statistically significant), it is barely bigger than improvement of 0.6 which is said to be the smallest change that is clinically significant (Stucki. 1996).
Not only is the improvement by the consultation small in clinical terms. It is also rather inconsistent. for example Table 6 shows that the consultation seemded to result in a detectable effect on swollen joint count, but not on tender joint count. Neither was there any significant effect of the consultation on the response to “considering all the ways your arthritis affects you, please make a vertical line to show how well you are now”. There appeared to be an improvement on “negative mood score”, but not on “positive mood score”. Effects of the consultation on pain scores was marginal at best.
It seems to me that the conclusion that the consultation process helps patients, though not entirely implausible, gets marginal support from this study. It may be real, but if so it isn’t a large effect.
Like most alternative medicine advocates, the authors of this paper make the mistake of confusing caring and curing. Caring is good if there is nothing else that can be done (as is only too often the case). But what patients really want is cures and they’ll never get that from an empathetic consultation.
The problem of Human Resources
What does all this mean for alternative medicine on the NHS? Nobody denies the desirability of empathy. In fact it is now talked about so much that there is a danger that scientific medical education will be marginalised. My own experience of the NHS is that most doctors are quite good at empathy, without any need to resort to hocus pocus like homeopathy and all the myriad forms of mythical medicine.
It must be said that Drs Avery and Lewith have had proper medical training. Their views on alternative medicine seem bizarre to me, but at least they should do no great harm. Sadly, the same can’t be said for the majority of homeopaths who have no medical training and who continue to andanger the public by recommending sugar pills for anything from malaria to Dengue fever. People like that have no place in the NHS. Indeed some are in jail.
Not long ago, I was invited to tour the oncology wards at UCL hospital with their chief spiritual healer, Angie Buxton-King. Although in her private practice she offers some pretty bizarre services like healing humans and animals at a distance, I had the impression that on the wards she did a pretty good job holding hands with people who were nervous about injections and chatting to people in for their third lot of chemotherapy. I asked if she would object to being called a "supportive health care worker" rather than a spiritual healer. Somewhat reluctantly she said that she wouldn’t mind that. But it can’t be done because of the absurd box-ticking mentality of HR departments. There is no job-description for someone who holds hands with patients, and no formal qualifications. On the other hand, if you are sufficiently brainless, you can tick a box for a healer. Once again I wish that HR departments would not hinder academic integrity.
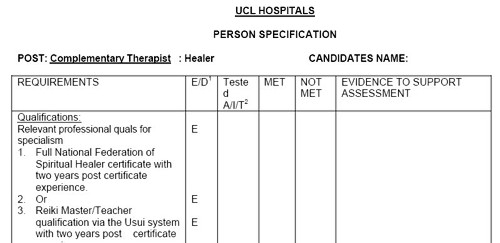
Follow-up
Steven Novella, at Science-Based medicine, has also written about this paper.
The mainstream media eventually catch up with bloggers. BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. It also exposed the uselessness of the Quality Assurance Agency (QAA). Both these things have been written about repeatedly here for some years. It was good to see them getting wider publicity.
Watch the video of the programme (Part 1, and Part 2) "Week In Week Out – University Challenged." “The programme examines how pop stars and evangelical Christians are running colleges offering courses validated by the University of Wales.” (I make a brief appearance, talking about validation of degrees in Chinese Medicine).

In October 2008 I posted Another worthless validation: the University of Wales and nutritional therapy. With the help of the Freedom of Information Act, it was possible to reveal the mind-boggling incompetence of the validation process used by the University of Wales.
McTimoney College of Chiropractic
The Chiropractic “degrees” from the McTimoney College of Chiropractic are also validated by the University of Wales by an equally incompetent, or perhaps I should say bogus, procedure. More details can be found at The McTimoney Chiropractic Association would seem to believe that chiropractic is “bogus”, and in a later post, Not much Freedom of Information at University of Wales, University of Kingston, Robert Gordon University or Napier University.
Andy Lewis has also written about chiropractic in The University of Wales is Responsible for Enabling Bogus* Chiropractic Claims to be Made.
Sadly the BBC programme did not have much to say about these domestic courses, but otherwise it was excoriating. In particular it had extensive interviews with Nigel Palastanga, whose astonishing admission that courses were validated withour seeing what was taught on them was revealed here two years ago. After that revelation, the vice-chancellor of UoW, Marc Clement BSc PhD CEng CPhys FIET FInstP, promoted Palastanga to be pro-vice-chancellor in charge of Learning, Teaching and Enhancement (I know, you couldn’t make it up).

In the documentary Palastanga said
"It’s a major business. We earn a considerable amount of money."
That was obvious two years ago, but it’s good to hear it from the horse’s mouth.
After a section that revealed a bit about what goes on at two very fundamentalist bible colleges which gave University of Wales degrees, A. C. Grayling commented thus.
"They are there to train advocates for the biblical message and that is absolutely not, by a very very long chalk, what a university should be doing.. . . A respectable British Higher education institution like the University of Wales shouldn’t be touching them with a bargepole."
Undaunted, Palastanga responded
“That’s his opinion. I would say they are validated to the highest standards. They match what are called QAA benchmark. We have serious academics looking at them, and their academic standards are established at the very highest level.”
And if you believe that, you will truly believe anything.
You can download here one of many moderator’s reports obtained under the Freedom of Information Act. This one is for the BSc (Hons) Chiropractic. It is entirely typical of theuncritical boxticking approach to validation, Nowhere does it say "subluxation is nonsense", though even the GCC now admit that.
Traditional Chinese Medicine
The University of Wales validates several courses in what almost everyone but them classifies as quackery. As well as chiropractic and “nutritional therapy”, there is herbalism. For example a course at a college in Barcelona issues University of Wales degrees in Traditional Chinese medicine, a subject that is a menace to public health.. I was asked to comment on the course, and on a bag of herbs that the presenter had been sold to treat depression.
|
Radix Bupleuri Chinensis
Radix Angelicae Sinensis Radix Paeoniae Lactiflorae Rhizoma Atractylodis Macrocephalae Sclerotium Poriae Cocos Radix Glycyrrhizae Uralensis Cortex Moutan Radicis (Paeonia Suffruticosa) Fructus Gardeniae Jasminoidis Herba Menthae Haplocalycis Zingiber officinale rhizome-fresh |
 Ingredients of a custom mixture. |
There is no good evidence that any of the ingredients help depression, in fact next to nothing is known about most of them, apart from liquorice and ginger. Swallowing them would be rather reckless. They fall right into the description of any herbal medicine, in the Patients’ Guide, "Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety. "
Of the degrees, I said
"There’s no evidence that it [the herbs] does you any good. It may be dangerous because you have no idea of the dose. Degrees in Chinese Medicine consist of three years spent memorising myths and pre-scientific, er, untruths. That isn’t a degree, it’s a travesty."
Palastanga. responded
"We’ve had long debates in the Health Committee about where we would draw the line about what we validate. They have to demonstrate to us that there is some scientific basis for the practice, that there is an established curriculum, that there is an established safe practice."
The presenter asked him "So you are confident that Chinese medicine works? Palastanga replied
" I didn’t say that. I said that there is evidence that it does work . . We are trying to enforce these professions to undertake effective research."
That statement is simply not true, as shown by the response of the validation committee to the application for validation of the course in “Nutritional Therapy” at the Northern College of Acupuncture, documented previously. The fact of the matter is that the validation proceeded without looking at what was actually taught, and without even a detailed timetable of lectures. The committee looked only at the official documents presented to it and was totally negligent in failing to discover some of the bizarre beliefs of the people who were giving the course.
Palastanga went on to raise the usual straw man argument, about how little regular medicine is based on good evidence (though admittedly that is certainly true in his own field -he is a physiotherapist).
Fazley International College Kuala Lumpur

This business college in Kuala Lumpur offered University of Wales degrees. Its 32-year old president is a part time pop star with impressive looking qualifications

The presenter pointed out that
" His doctorate and his MBA were awarded in that citadel of education, Cambridge. Here he is, pictured at the city’s prestigious business school. He was there for all of four days and walked away with a doctorate. But the degree was not from the University of Cambridge, but from the now defunct "European Business School Cambridge". It never had the right to award degrees."
Neither the University of Wales nor the QAA had noticed this unfortunate fact. Once the TV team had done their job for them, the UoW withdrew support. though, as of 15 November 2010, that is not obvious from Fazley’s web site.
Mr (not Dr) Fazley seemed rather pleased about how students were attracted by the connection with the Prince of Wales. The fact that he is Chancellor of the University of Wales seems not inappropriate, given the amount of quackery they promote.
Quality Assurance Agency (QAA)
In 2007, I wrote, in Nature (see also here),
“Why don’t regulators prevent BSc degrees in anti-science? The Quality Assurance Agency for Higher Education (QAA) claims that “We safeguard and help to improve the academic standards and quality of higher education in the UK.” It costs taxpayers £11.5 million (US$22 million) annually. It is, of course, not unreasonable that governments should ask whether universities are doing a good job. But why has the QAA not noticed that some universities are awarding BSc degrees in subjects that are not, actually, science? The QAA report on the University of Westminster courses awards a perfect score for ‘curriculum design, content and organization,’ despite this content consisting largely of what I consider to be early-nineteenth-century myths, not science. It happens because the QAA judges courses only against the aims set by those who run the QAA, and if their aims are to propagate magic as science, that’s fine.”
That was illustrated perfectly in the documentary when Dr Stephen Jackson of the QAA appeared to try to justify the fact that the QAA had, like the University of Wales, failed entirely to spot any of the obvious problems. He had a nice dark suit, tie and poppy, but couldn’t disguise the fact that the QAA had given high ratings to some very dubious courses.
The QAA sent nine people to the other side of the globe, at a cost of £91,000. They could have done a lot better if they’d spent 10 minutes with Google at home.
Universities UK (UUK)
Needless to say, the Committee of Vice-Chancellors and Principals has said nothing at all. As usual, Laurie Taylor had it all worked out in Times Higher Education (4th November).
Speaking to our reporter Keith Ponting (30), he commended UUK’s decision to say absolutely nothing whatsoever about the abolition of all public funding for the arts and humanities.
He also praised UUK’s total silence on Lord Browne’s view that student courses should primarily be evaluated by their employment returns.
When pressed by Ponting for his overall view of UUK’s failure to respond in any way at all to any aspect of the Browne Review, he described it as “welcome evidence, in a world of change, of UUK’s consistent commitment over the years to ineffectual passivity”.
Meanwhile, a University of Wales video on YouTube

Caveat emptor
Follow-up
A couple of days later, a search of Google news for the “University of Wales” shows plenty of fallout. The vice-chancellor claims that ““The Minister’s attack came as a complete and total surprise to me”. That can’t be true. It is over two years since I told him what was going on, and if he was unaware of it, that is dereliction of duty. It is not the TV programme that brought the University into disrepute, it was the vice-chancellor.
The last few weeks have produced yet another example of how selective reporting can give a very misleading impression.
As usual, the reluctance of the media to report important negative results is, in part, to blame..
The B vitamins are a favourite of the fraudulent supplements industry. One of theit pet propositions is that they will prevent dementia. The likes of Patrick Holford were, no doubt, delighted when a study from Oxford University, published on September 8th, seemed to confirm their ideas. The paper was Homocysteine-Lowering by B Vitamins Slows the Rate of Accelerated Brain Atrophy in Mild Cognitive Impairment: A Randomized Controlled Trial. (Smith AD, Smith SM, de Jager CA, Whitbread P, Johnston C, et al. (2010)).
The main problem with this paper was that it did not measure dementia at all, but a surrogate outcome, brain shrinkage. There are other problems too. They were quickly pointed out in blogs, particularly by the excellent Carl Heneghan of the Oxford Centre for Evidence Based Medicine, at Vitamin B and slowing the rate of Brain Atrophy: the numbers don’t add up. Some detailed comments on this post were posted at Evidence Matters, David Smith, B vitamins and Alzheimer’s Disease.
This paper was reported very widely indeed. A Google search for ‘Vitamin B Alzheimer’s Smith 2010’ gives over 90,000 hits at the time of posting. Most of those I’ve checked report this paper uncritically. The Daily Mail headline was 10p pill to beat Alzheimer’s disease: Vitamin B halts memory loss in breakthrough British trial, though in fairness to Fiona MacRae, she did include at the end
“The Alzheimer’s Society gave the research a cautious welcome. Professor Clive Ballard said: ‘This could change the lives of thousands of people at risk of dementia. However, previous studies looking at B vitamins have been very disappointing and we wouldn’t want to raise people’s expectations yet.’ “
That caution was justified because a mere two weeks later, on September 22nd, another paper appeared, in the journal Neurology.. The paper is Vitamins B12, B6, and folic acid for cognition in older men, by Ford et al. It appears to contradict directly Smith et al. but it didn’t measure the same thing. This one measured what actually matters.
“The primary outcome of interest was the change in the cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-cog). A secondary aim of the study was to determine if supplementation with vitamins decreased the risk of cognitive impairment and dementia over 8 years.”
The conclusion was negative.
“Conclusions: The daily supplementation of vitamins B12, B6, and folic acid does not benefit cognitive function in older men, nor does it reduce the risk of cognitive impairment or dementia.”
Disgracefully, this paper has hardly been reported at all.
It is an excellent example of how the public is misled because of the reluctance of the media to publish negative results. Sadly that reluctance is sometimes also shown by academic journals, but not in this case.
Two things went wrong, The first was near-universal failure to evaluate critically the Smith et al paper. The second was to ignore the paper that measured what actually matters.
It isn’t as though there wasn’t a bit of relevant history, Prof Smith was one of the scientific advisors for Patrick Holford’s Food for the Brain survey. This survey was, quie rightly, criticised for being uninterpretable. When asked about this, Smith admitted as much, as recounted in Food for the Brain: Child Survey. A proper job?.
Plenty has been written about Patrick Holford, here and elsewhere. There is even a web site that is largely devoted to dispelling his myths, Holford Watch. He merited an enture chapter in Ben Goldacre’s book, Bad Science. He is an archetypal pill salesman and the sciencey talk seems to be largely used as a sales tool.
It might have been relevant too, to notice that the Smith et al. paper stated
|
Competing interests: Dr. A. D. Smith is named as an inventor on two patents held by the University of Oxford on the use of folic acid to treat Alzheimer’s disease (US6008221; US6127370); under the University’s rules he could benefit financially if the patent is exploited. |
There is, of course, no reason to think that the interpretation of the data was influenced by he fact that the first author had a financial interest in the outcome. In fact university managers encourage that sort of thing strongly.
Personally, I’m more in sympathy with the view expressed by Strohman (1997)
“academic biologists and corporate researchers have become indistinguishable, and special awards are given for collaborations between these two sectors for behaviour that used to be cited as a conflict of interest”.
When it comes to vitamin pills, caveat emptor.
















