George Lewith
This piece is almost identical with today’s Spectator Health article.
This week there has been enormously wide coverage in the press for one of the worst papers on acupuncture that I’ve come across. As so often, the paper showed the opposite of what its title and press release, claimed. For another stunning example of this sleight of hand, try Acupuncturists show that acupuncture doesn’t work, but conclude the opposite: journal fails, published in the British Journal of General Practice).
Presumably the wide coverage was a result of the hyped-up press release issued by the journal, BMJ Acupuncture in Medicine. That is not the British Medical Journal of course, but it is, bafflingly, published by the BMJ Press group, and if you subscribe to press releases from the real BMJ. you also get them from Acupuncture in Medicine. The BMJ group should not be mixing up press releases about real medicine with press releases about quackery. There seems to be something about quackery that’s clickbait for the mainstream media.
As so often, the press release was shockingly misleading: It said
Acupuncture may alleviate babies’ excessive crying Needling twice weekly for 2 weeks reduced crying time significantly
This is totally untrue. Here’s why.
|
Luckily the Science Media Centre was on the case quickly: read their assessment. The paper made the most elementary of all statistical mistakes. It failed to make allowance for the jelly bean problem. The paper lists 24 different tests of statistical significance and focusses attention on three that happen to give a P value (just) less than 0.05, and so were declared to be "statistically significant". If you do enough tests, some are bound to come out “statistically significant” by chance. They are false postives, and the conclusions are as meaningless as “green jelly beans cause acne” in the cartoon. This is called P-hacking and it’s a well known cause of problems. It was evidently beyond the wit of the referees to notice this naive mistake. It’s very doubtful whether there is anything happening but random variability. And that’s before you even get to the problem of the weakness of the evidence provided by P values close to 0.05. There’s at least a 30% chance of such values being false positives, even if it were not for the jelly bean problem, and a lot more than 30% if the hypothesis being tested is implausible. I leave it to the reader to assess the plausibility of the hypothesis that a good way to stop a baby crying is to stick needles into the poor baby. If you want to know more about P values try Youtube or here, or here. |
One of the people asked for an opinion on the paper was George Lewith, the well-known apologist for all things quackish. He described the work as being a "good sized fastidious well conducted study ….. The outcome is clear". Thus showing an ignorance of statistics that would shame an undergraduate.
On the Today Programme, I was interviewed by the formidable John Humphrys, along with the mandatory member of the flat-earth society whom the BBC seems to feel obliged to invite along for "balance". In this case it was professional acupuncturist, Mike Cummings, who is an associate editor of the journal in which the paper appeared. Perhaps he’d read the Science media centre’s assessment before he came on, because he said, quite rightly, that
"in technical terms the study is negative" "the primary outcome did not turn out to be statistically significant"
to which Humphrys retorted, reasonably enough, “So it doesn’t work”. Cummings’ response to this was a lot of bluster about how unfair it was for NICE to expect a treatment to perform better than placebo. It was fascinating to hear Cummings admit that the press release by his own journal was simply wrong.
Listen to the interview here
Another obvious flaw of the study is that the nature of the control group. It is not stated very clearly but it seems that the baby was left alone with the acupuncturist for 10 minutes. A far better control would have been to have the baby cuddled by its mother, or by a nurse. That’s what was used by Olafsdottir et al (2001) in a study that showed cuddling worked just as well as another form of quackery, chiropractic, to stop babies crying.
Manufactured doubt is a potent weapon of the alternative medicine industry. It’s the same tactic as was used by the tobacco industry. You scrape together a few lousy papers like this one and use them to pretend that there’s a controversy. For years the tobacco industry used this tactic to try to persuade people that cigarettes didn’t give you cancer, and that nicotine wasn’t addictive. The main stream media obligingly invite the representatives of the industry who convey to the reader/listener that there is a controversy, when there isn’t.
Acupuncture is no longer controversial. It just doesn’t work -see Acupuncture is a theatrical placebo: the end of a myth. Try to imagine a pill that had been subjected to well over 3000 trials without anyone producing convincing evidence for a clinically useful effect. It would have been abandoned years ago. But by manufacturing doubt, the acupuncture industry has managed to keep its product in the news. Every paper on the subject ends with the words "more research is needed". No it isn’t.
Acupuncture is pre-scientific idea that was moribund everywhere, even in China, until it was revived by Mao Zedong as part of the appalling Great Proletarian Revolution. Now it is big business in China, and 100 percent of the clinical trials that come from China are positive.
if you believe them, you’ll truly believe anything.
Follow-up
29 January 2017
Soon after the Today programme in which we both appeared, the acupuncturist, Mike Cummings, posted his reaction to the programme. I thought it worth posting the original version in full. Its petulance and abusiveness are quite remarkable.
I thank Cummings for giving publicity to the video of our appearance, and for referring to my Wikipedia page. I leave it to the reader to judge my competence, and his, in the statistics of clinical trials. And it’s odd to be described as a "professional blogger" when the 400+ posts on dcscience.net don’t make a penny -in fact they cost me money. In contrast, he is the salaried medical director of the British Medical Acupuncture Society.
It’s very clear that he has no understanding of the error of the transposed conditional, nor even the mulltiple comparison problem (and neither, it seems, does he know the meaning of the word ‘protagonist’).
I ignored his piece, but several friends complained to the BMJ for allowing such abusive material on their blog site. As a result a few changes were made. The “baying mob” is still there, but the Wikipedia link has gone. I thought that readers might be interested to read the original unexpurgated version. It shows, better than I ever could, the weakness of the arguments of the alternative medicine community. To quote Upton Sinclair:
“It is difficult to get a man to understand something, when his salary depends upon his not understanding it.”
It also shows that the BBC still hasn’t learned the lessons in Steve Jones’ excellent “Review of impartiality and accuracy of the BBC’s coverage of science“. Every time I appear in such a programme, they feel obliged to invite a member of the flat earth society to propagate their make-believe.
Acupuncture for infantile colic – misdirection in the media or over-reaction from a sceptic blogger?26 Jan, 17 | by Dr Mike Cummings So there has been a big response to this paper press released by BMJ on behalf of the journal Acupuncture in Medicine. The response has been influenced by the usual characters – retired professors who are professional bloggers and vocal critics of anything in the realm of complementary medicine. They thrive on oiling up and flexing their EBM muscles for a baying mob of fellow sceptics (see my ‘stereotypical mental image’ here). Their target in this instant is a relatively small trial on acupuncture for infantile colic.[1] Deserving of being press released by virtue of being the largest to date in the field, but by no means because it gave a definitive answer to the question of the efficacy of acupuncture in the condition. We need to wait for an SR where the data from the 4 trials to date can be combined. So what about the research itself? I have already said that the trial was not definitive, but it was not a bad trial. It suffered from under-recruiting, which meant that it was underpowered in terms of the statistical analysis. But it was prospectively registered, had ethical approval and the protocol was published. Primary and secondary outcomes were clearly defined, and the only change from the published protocol was to combine the two acupuncture groups in an attempt to improve the statistical power because of under recruitment. The fact that this decision was made after the trial had begun means that the results would have to be considered speculative. For this reason the editors of Acupuncture in Medicine insisted on alteration of the language in which the conclusions were framed to reflect this level of uncertainty. DC has focussed on multiple statistical testing and p values. These are important considerations, and we could have insisted on more clarity in the paper. P values are a guide and the 0.05 level commonly adopted must be interpreted appropriately in the circumstances. In this paper there are no definitive conclusions, so the p values recorded are there to guide future hypothesis generation and trial design. There were over 50 p values reported in this paper, so by chance alone you must expect some to be below 0.05. If one is to claim statistical significance of an outcome at the 0.05 level, ie a 1:20 likelihood of the event happening by chance alone, you can only perform the test once. If you perform the test twice you must reduce the p value to 0.025 if you want to claim statistical significance of one or other of the tests. So now we must come to the predefined outcomes. They were clearly stated, and the results of these are the only ones relevant to the conclusions of the paper. The primary outcome was the relative reduction in total crying time (TC) at 2 weeks. There were two significance tests at this point for relative TC. For a statistically significant result, the p values would need to be less than or equal to 0.025 – neither was this low, hence my comment on the Radio 4 Today programme that this was technically a negative trial (more correctly ‘not a positive trial’ – it failed to disprove the null hypothesis ie that the samples were drawn from the same population and the acupuncture intervention did not change the population treated). Finally to the secondary outcome – this was the number of infants in each group who continued to fulfil the criteria for colic at the end of each intervention week. There were four tests of significance so we need to divide 0.05 by 4 to maintain the 1:20 chance of a random event ie only draw conclusions regarding statistical significance if any of the tests resulted in a p value at or below 0.0125. Two of the 4 tests were below this figure, so we say that the result is unlikely to have been chance alone in this case. With hindsight it might have been good to include this explanation in the paper itself, but as editors we must constantly balance how much we push authors to adjust their papers, and in this case the editor focussed on reducing the conclusions to being speculative rather than definitive. A significant result in a secondary outcome leads to a speculative conclusion that acupuncture ‘may’ be an effective treatment option… but further research will be needed etc… Now a final word on the 3000 plus acupuncture trials that DC loves to mention. His point is that there is no consistent evidence for acupuncture after over 3000 RCTs, so it clearly doesn’t work. He first quoted this figure in an editorial after discussing the largest, most statistically reliable meta-analysis to date – the Vickers et al IPDM.[2] DC admits that there is a small effect of acupuncture over sham, but follows the standard EBM mantra that it is too small to be clinically meaningful without ever considering the possibility that sham (gentle acupuncture plus context of acupuncture) can have clinically relevant effects when compared with conventional treatments. Perhaps now the best example of this is a network meta-analysis (NMA) using individual patient data (IPD), which clearly demonstrates benefits of sham acupuncture over usual care (a variety of best standard or usual care) in terms of health-related quality of life (HRQoL).[3] |
30 January 2017
I got an email from the BMJ asking me to take part in a BMJ Head-to-Head debate about acupuncture. I did one of these before, in 2007, but it generated more heat than light (the only good thing to come out of it was the joke about leprechauns). So here is my polite refusal.
|
Hello Thanks for the invitation, Perhaps you should read the piece that I wrote after the Today programme Why don’t you do these Head to Heads about genuine controversies? To do them about homeopathy or acupuncture is to fall for the “manufactured doubt” stratagem that was used so effectively by the tobacco industry to promote smoking. It’s the favourite tool of snake oil salesman too, and th BMJ should see that and not fall for their tricks. Such pieces night be good clickbait, but they are bad medicine and bad ethics. All the best David |
|
“In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established”. . . “. . . they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.” David Mattin, lately of NHS Choices |
NHS Choices is usually a good source of information for the public. But there is one exception: the information they provide about alternative medicine is poor. A Freedom of Information Act request has revealed that the attempt of NHS Choices to rewrite their pages more accurately was censored by the Department of Health in conjunction with the late Prince’s Foundation for Integrated Health. The Department of Health (DH) has misled the public.
The earliest version of the homeopathy information page recorded by the Wayback Machine was November 12 2007. It was still there on December 5 2010. The comments were mostly critical. One said, quite correctly,
|
I find it most regrettable that the way NHS has covered this subject is to give uncritical voice to the claims of homoeopathy without giving readers the information they need to evaluate those claims. To refer readers to the websites of the British Homeopathy Association is like settling the question of the shape of planet by a reference to the website of the Flat Earth Society |
There were a lot of complaints, and to the credit of NHS Choices, the page vanished. Throughout 2011, and up to October 2012 the information page on homeopathy read
|
Introduction Content on homeopathy has been removed from the website pending a review by the Department of Health policy team responsible for complementary and alternative medicines. Homeopathy is not part of mainstream medicine. Instead it is defined as a complementary or alternative medicine. If you are considering using homeopathy, talk to your GP first. For more information about homeopathy see the House of Commons Science and Technology Committee report on homeopathy published on 8 February 2010 and the Department of Health response to that report published in July 2010 (PDF, 69KB). |
Then, at the end of 2012, the page reappeared. It was a bit better than the original, but not much. Many of the comments criticise the misleading nature of the information (as well as the usual “it worked for me” comments). The “useful links” still has six links to flat-earth organisations like the Society of Homeopaths, and only one to a sensible source, the excellent pamphlet from Sense about Science. They do link at the end to the 2010 Science and Technology Committee Report: Evidence Check 2: Homeopathy (PDF, 1.61Mb), and to the Government Response to the Science and Technology Committee Report, Evidence Check 2: Homeopathy (PDF, 69kb) but no comment is made on the findings.
Policy-based evidence
I wondered why the NHS Choices page, after an absence of almost two years, had returned in such an unsatisfactory form. So I asked them. After a reminder, I was told that my queries were being dealt with not by NHS Choices, but had been referred to Dr Sunjai Gupta “the DH official with responsibility for this area”. Dr Sunjai Gupta OBE is Deputy Director of Public Health Strategy and Social Marketing, Department of Health.
Dr Gupta is not obviously sympathetic to woo. It’s hard to tell since he doesn’t seem to have published much. But one is not reassured by an article that he wrote for the Journal of Holistic Healthcare. It appears straight after an article by fantasy herbalist, Simon Mills.
Despite assurances that I’d hear from Dr Gupta shortly, nothing happened. So I sent a request for the correspondence under the Freedom of Information Act (2000). Although the request was addressed to NHS Choices, a public body, strenuous efforts were made to divert it to the Department of Health. These were resisted. Nevertheless when, after a long delay, the material arrived, it came not from NHS Choices, but from DH, who had evidently vetted it,. The emails were rather shocking [download all].
A mail dated 1 December 2009 said

This is the most direct statement I’ve seen that, in the Department of Health, policy dictates evidence. NHS Choices is meant to provide evidence, but what they say has to be checked by DH to make sure they “don’t clash with any policy messages”.
The re-written page
The original version of the re-written page was sent to me by David Mattin, who worked for NHS Choices until September 2012. You can download the whole draft here. It is an enormous improvement on the original page. For example, it says
|
“Does it work?
Many independent experts would respond to this question ‘no, homeopathy does not work’ There is no good quality clinical evidence to show that homeopathy is more successful than placebo in the treatment of any type of condition. Furthermore, if the principles of homeopath were true it would violate all the existing theories of science that we make use of today; not just our theory of medicine, but also chemistry, biology and physics. |
This original draft was sent to Mattin on 29 January 2010. After editing it for length Mattin sent it to DH for approval. Over the next two years, DH removed much of the accurate content. Mattin’s own comments on this evisceration are reproduced below.
The DH emails
All the names have been redacted. Needless to say, nobody is willing to take responsibility. But the number of people who support magic medicine is really quite small so the main players were easy to identify.
During the nearly 2 year absence of the homeopathy page, dozens of changes were made by DH. It seems that the policy message with which the NHS Choices draft failed to comply were those of the Prince’s Foundation for Integrated Health, and its successor (after April 2010), the College of Integrated Health, now known as the College of Medicine.
NHS Choices sought advice about their redrafted pages from the right person, Sir Iain Chalmers, one of the founders of the Cochrane Collaboration. On 3 Nov 2009, Chalmers advised
The most reliable source in the country - and one of the most reliable in the world - is Professor Edzard Ernst, professor of Complementary Medicine at the Peninsular Medical School, |
Ernst returned his suggestions in July 2010, but it seems that few of them survived the subsequent 18 months of revisions by DH.
On 2 December 2009, a mail from the NHS headquarters (Quarry House, Leeds) was sent to NHS Choices

This makes it perfectly clear that DH regards the Prince’s Foundation, and the equally flaky Complementary and Natural Healthcare Council (CNHC: known on the web as Ofquack) as appropriate guides for public health policy. The fact of the matter is that regulation of magic medicine by the government has been a total disaster, because, it seems, DH regards the Prince of Wales as a reliable source.
On 29 December 2009, the Prince’s Foundation went on the attack.

On 10th January 2010, two more letters were sent to DH by the Prince’s Foundation. At 13.48 they wrote

And at 22.14 on the same day, it was followed up with

The references to Devon and to Thought Field Therapy, make it very obvious that these letters were written by Dr Michael Dixon OBE, who was medical director of the Prince’s Foundation, and who is now a director of the “College of Medicine”. And the object of Dixon’s bile is obviously Edzard Ernst (the quotation is from his book, Trick or Treatment).
I find it fascinating to see just how venomous quacks become when the evidence contradicts their views. The cuddly “holistic” veneer quickly vanishes.
It gets worse. On 21 January 2010, a mail from NHS Choices to DH said

The only person in the country who fits this description is the (in)famous George Lewith. It is simply mind-boggling that DH regards him as an appropriate person to advise on anything.
After that, NHS Choices kept asking DH to sign off the documents, and changes continued to be made. Almost two years later, DH were still stalling.

The admission that “We are a bit short of doctors within DH these days” is interesting.
A bit short of anyone capable of critical thinking would be more accurate.
The most interesting document that I got from DH was an intermediate draft of the rewritten page on homeopathy (undated). Download the document. Here are a couple of extracts.
It’s a story of two years of meddling and procrastination. The end result misinforms the public.
Right at the start, the NHS Choices draft says, reasonably enough
A House of Commons Science and Technology Committee report said that homeopathic remedies perform no better than placebos and that the principles on which homeopathv is based are “scientifically implausible”.
But a comment, added apparently by DH, says
Can we remove this statement? This report is really quite contentious and we may well be subject to quite a lot of challenge from the Homeopathic community if published.
What on earth? The DH seems to think that that its job is not to present the evidence, but to avoid challenges from the homeopathic community! And true enough, this piece is missing from the final version.
A bit later, the NHS Choices draft was censored again
“A 2010 Science and Technology Committee report said that scientific tests had shown that homeopathic treatments don’t work”
But again this doesn’t appear in the final version. The comment, apparently from DH, says
“The DH response to this report (point 24) doesn’t support this statement though”
That’s a gross distortion of point 24, which actually concludes
“The Government Chief Scientific Adviser cannot envisage scientifically credible proposals for funding for research into homeopathy in the future”
NHS Choices was not happy with the result
Shortly before the revised page was published, Paul Nuki, Editor in Chief of NHS Choicea, sent an email to DH.
|
Date: 7th September 2011 Time: 3:33:42 pm Hi I’ve been through the CAM articles and asked that we publish them asap as requested. For the record, we will be publishing these pieces outside of the normal editorial process. Although originally signed off by a suitably qualified clinician, the time lapse and policy changes have been so substantial as to render that null and void. We also don’t have a formal |
It doesn’t need much reading between the lines to see that he was unhappy with the result. It will be interesting to see whether the Information Standard people at the Royal Society for Public Health do anything about it.
The Department of Health has not just ignored evidence but actively opposed it.
That’s the only possible conclusion from the documents that I was sent. And it’s pretty shocking that the DH has preferred advice from the Prince’s Foundation and its handful of acolytes (in particular Michael Dixon and George Lewith) to the findings of the Science and Technology Select Committee and the views of the Chief Scientific Advisor.
In January this year, the Chief medical Officer, Dame Sally Davies, said, in a rare outburst of candour
|
‘I’m very concerned when homeopathic practitioners try to peddle this way of life to prevent malaria or other infectious disease,” she said. “I am perpetually surprised that homeopathy is available on the NHS.” Dame Sally, who is England’s most senior doctor, concluded by remarking that homeopathy “is rubbish”. |
 |
So one part of DH is working to contradict another part. the Chief Medical Officer. Perhaps Sally Davies should have a word with Dr Gupta.
This all predates the advent of Jeremy Hunt (and known defender of homeopathy) as health minister. But the sympathies of some DH people are made obvious by the presence on the DH web site of an article “Personal health budgets: A new way of accessing complementary therapies?”. This astonishing piece confirms the worst fears that quacks will see personal health budgets as a commercial opportunity to peddle their wares. The article is by Jim Rogers of Lincoln University. What his paper does not mention is Rogers’ conflict of interest. He’s a homeopath, and he has a paper in the International Journal of High Dilution Research (yes, there is a journal for every form of make-believe). You can download a reprint of this paper. It advocates more research into homeopathic provings, something that even George Lewith seems to have given up on.
It’s about time that the DH started to listen to the Chief Medical Officer. As it is, some people at DH seem to prefer the advice of the Prince’s Foundation, and to actively suppress employees who prefer evidence to anecdote.
One thing is clear. The DH is an unholy mess. Parts of it are intent on producing policy-based evidence.
Comment by David Mattin, who edited the first draft for NHS Choices
David Mattin left NHS Choices in September, 2012. He edited the new version and lived through the two years of wrangling with DH during which much of the best content was eviscerated. He sent me this statement about the affair.
|
As an editor at NHS Choices, I viewed it as my job to present evidence-based information to the public. The article we prepared on homeopathy stayed true to that central purpose: it made clear to readers that there is no good quality evidence that homeopathy is an effective treatment for any health condition, and also presented the broad scientific consensus that the supposed method of action of homeopathy is implausible.
What followed was a two year story of delay, and eventual suppression, of that article. My strong impression was of DH civil servants who lacked the courage, and, frankly, the energy to stand up to the criticism from special interest groups that they anticipated would arise because of the article; and that did indeed arise when a draft of the article and other draft content on complementary and alternative medicines fell into the hands of the Prince’s Foundation and other CAM groups.
The attitude of DH civil servants, broadly, was simply to tell us ‘we can’t say this about homeopathy, people will complain’. They seemed to have no interest in making an appraisal of the evidence on homeopathy themselves to see if what we were saying was actually true or not. We repeatedly pushed back with the message: ‘some people may very well complain, but if what we are saying about the evidence base is true – and it is – then we must simply weather those complaints, and stand by our content. Our duty is to supply our readers with the best information, not to please the homeopathy community.’ But these arguments were disregarded. The DH civil servants were almost entirely concerned with the politics of the situation – that is, the politics as they saw them – and the possibility that this article may create new work for them, and very little concerned with the evidence itself, or the presentation of this evidence to the public.
The whole episode is an insight into the way special interest groups can influence the workings of government and the public sector simply by making a lot of noise, and having a few powerful friends. In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established, and that they fund. They have sold out the NHS Choices editorial team, who work tirelessly to fulfil their remit. And, most seriously, they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.
|
Follow-up
13 February 2013 The Guardian version of this story, written by Sarah Boseley, is Prince’s charity lobbied government to water down homeopathy criticism. It’s fine as far as it goes but it doesn’t name any names. There are some good comments though.
14 February 2013. The printed Guardian gave the story full 5 column-width coverage. [download print version]
And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
On 14 February, the Guardian version was Editor’s Choice by lunchtime, and the Guardian web version already had 414 comments, mostly sensible (though this blog got far more referrals from twitter than from the Guardian)

And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
15 February 2013. The Daily Mail had very fair coverage of the story.

The Guardian closed the comments on the story when it had got 642 comments, most of them very sensible. And this page got almost 6000 hits in 24 hours. The majority of the referrals came from Twitter rather than from the Guardian, despite the direct link to the page from the Guardian.
18 February 2013. The affair featured in BMJ News [download the reprint]. The item featured prominently on the BMJ news page.


19 February 2013 Only six days of this post, the NHS Choices page has been re-written again, in a much improved form. That looks like bloggers 1, DH 0. It is baffling that it’s left to bloggers, working for nothing, to extract a bit of sense from the highly-paid civil servants at the Department of Health. But at least they listened this time, which is a lot more than happens often. Paul Nuki, who runs NHS Choices, deserves congratulations. Of course the revised page still doesn’t call a spade a spade, but it gets close at times. I like the way it starts "Homeopathy is a ‘treatment’ based". Notice the quotation marks.
Reputation management?
Incidentally, NHS Choices is outsourced to the (in)famous company, Capita. And the moderation of the comments on their site is outsourced again to Tempero, which describes itself as a "reputation management" company. Each of them creams off money meant of patient care. This discovery might explain why I and others have had comments rejected by NHS Choices several times. "Reputation management" is the antithesis of evidence. It is public relations, i.e. paid lying. That is quite wrong for a site that is meant to provide dispassionate information.
21 February 2013. Sadly a step backwards. Part of the improved page was removed. This bit.
The Chief Medical Officer, Professor Dame Sally Davies, has said there is no scientifically plausible way that homeopathy can prevent or cure diseases. She has made it clear she is particularly concerned about the use of homeopathy in developing countries as a so-called cure for malaria.
We can only speculate why this was removed, because it was true. In fact she accurately described homeopathy as "rubbish". Why she should not be quoted beats me.
The College of Medicine is well known to be the reincarnation of the late unlamented Prince of Wales Foundation for Integrated Health. I labelled it as a Fraud and Delusion, but that was perhaps over-generous. It seems to be morphing into a major operator in the destruction of the National Health Service through its close associations with the private health industry.
Their 2012 Conference was held on 3rd May. It has a mixture of speakers, some quite sound, some outright quacks. It’s a typical bait and switch event. You can judge its quality by the fact that the picture at the top of the page that advertises the conference shows Christine Glover, a homeopathic pharmacist who makes a living by selling sugar pills to sick people (and a Trustee of the College of Medicine).
Her own company’s web site says
The approaches are, of course, based on sugar pills. The claim is untrue and dangerous. My name for that is fraud. |
 |
When the "College of Medicine" started it was a company, but on January 30th 2012, it was converted to being a charity. But the Trustees of the charity are the same people as the directors of the company. They are all advocates of ineffective quack medicine. The contact is named as Linda Leung, who was Operations Director of the Prince’s Foundation until it closed, and then became Company Secretary for the “College of Medicine”.
The trustees of the charity are the same people who were directors of the company
- Dr Michael Dixon, general practitioner. Michael Dixon was Medical Director of the Prince’s Foundation until it closed down.
- Professor George Lewith, is Professor of Health Research in the Complementary Medicine Research Unit, University of Southampton. He was a Foundation Fellow of the Prince’s Foundation until it closed down. Much has been written about him here.
- Professor David Peters. is Professor of Integrated Healthcare and Clinical Director at the University of Westminster’s School of Integrated Health; He’s famous for allowing dowsing with a pendulum as a method of diagnosis for treatment with unproven herbal medicines,
He was a Foundation Fellow of the Prince’s Foundation until it closed down. - Mrs Christine Glover is a pharmacist who sells homeopathic pills. She was a Foundation Fellow of the Prince’s Foundation until it closed down.
The involvement of Capita
According to their web site
"A Founder of the College of Medicine is Capita."
Still more amazingly, the CEO of the College of Medicine is actually an employee of Capita too.
"Mark Ratnarajah is interim CEO of the College of Medicine as well as Business Director at Capita Health and Wellbeing."

|
That isn’t the end of it. The vice-president of the College of Medicine is Dr Harry Brunjes. There is an article about him in the May 2012 issue of Director Magazine. It has to be said that he doesn’t sound like a man with much interest in the National Health Service.. |
Within 9 years of graduating he set up in private practice in Harley Street. Five years later he set up Premier Medical, which, after swallowing a couple of rivals, he sold to Capita for £60 million. He is now recorded in a Companies House document as Dr Henry Otto Brunjes, a director of Capita Health Holdings Limited. This company owns all the shares in Capita Health and Wellbeing Limited, and it is, in turn, owned by Capita Business Services Limited. And they are owned by Capita Holdings Limited. I do hope that this baroquely complicated array of companies with no employees has nothing to do with tax avoidance.
Capita is, of course, a company with a huge interest in the privatisation of health care. It also has a pretty appalling record for ripping off the taxpayer.
It has long been known in Private Eye, as “Crapita” and “the world’s worst outsourcing firm”.
Capita were responsible for of the multimillion pound failed/delayed IT project for the NHS and HMRC. They messed up on staff administration services at Leicester Hospitals NHS Trust and the BBC where staff details were lost. They failed to provide sufficient computing systems for the Criminal Records Bureau, which caused lengthy delays. Capita were also involved in the failure of the Individual Learning Accounts following a £60M over-spend. And most recently, they have caused the near collapse of court translation services after their acquisition of Applied Language Services.
With allies like that, perhaps the College of Medicine hardly needs enemies. No doubt Capita will be happy to provide the public with quackery for an enormous fee from the taxpayer.
 |
One shouldn’t be surprised that the College is involved in Andrew Lansley’s attempts to privatise healthcare. Michael Dixon, Chair of the College of Medicine, also runs the "NHS Alliance", almost the only organisation that supported the NHS Bill. The quackery at his own practice defies belief (some it is described here). |
One would have thought that such a close association with a company with huge vested interests would not be compatible with charitable status. I’ve asked the Charity Commission about that. The Charity commission, sadly, makes no judgements about the worthiness of the objects of the charities it endorses. All sorts of dangerous quack organisations are registered charities, like, for example, Yes to Life.
Secrecy at the College of Medicine
One of the big problems about the privatisation of medicine and education is that you can’t use the Freedom of Information Act to discover what they are up to. A few private companies try to abide by that act, despite not being obliged to do so. But the College of Medicine is not one of them.
Capita They refuse to disclose anything about their relationship with Capita. I asked I asked Graeme Catto, who is a friend (despite the fact that I think he’s wrong). I got nothing.
"Critical appraisal" I also asked Catto for the teaching materials used on a course that they ran about "critical appraisal". Any university is obliged, by the decision of the Information Tribunal, to produce such material on request. The College of Medicine refused, point blank. What, one wonders, have they got to hide? Their refusal strikes me as deeply unethical.
The course (costing £100) on Critical Appraisal, ran on February 2nd 2012. The aims are "To develop introductory skills in the critical appraisal of randomised controlled trials (RCTs) and systematic reviews (SRs)". That sounds good. Have they had a change of heart about testing treatments?
But, as always, you have to look at who is running the course. Is it perhaps a statistician with expertise in clinical trials? Or is it a clinician with experience in running trials? There are plenty of people with this sort of expertise. But no, It is being run by a pharmacist, Karen Pilkington, from that hotbed of unscientific medicine, the University of Westminster.
Pilkington originally joined the University of Westminster as manager for a 4-year project to review the evidence on complementary therapies (funded by the Department of Health). All of her current activities centre round alternative medicine and most of her publications are in journals that are dedicated to alternative medicine. She teaches "Critical Appraisal" at Westminster too, so I should soon have the teaching materials, despite the College’s attempts to conceal them.
Three people who ought to know better
Ore has to admire, however grudgingly, the way that the quacks who run the College of Medicine have managed to enlist the support of several people who really should know better. I suppose they have been duped by that most irritating characteristic of quacks, the tendency to pretend they have the monopoly on empathetic treatment of patients. We all agree that empathy is good, but every good doctor has it. One problem seems to be that senior medical people are not very good at using Google. They don’t do their homework.

|
Professor Sir Graeme Catto MD DSc FRCP FMedSci FRSE is president of the College of Medicine. He’s Emeritus Professor of Medicine at the University of Aberdeen. He was President of the General Medical Council from 2002 to 2009, Pro Vice-Chancellor, University of London and Dean of Guy’s, King’s and St Thomas’ medical school between 2000 and 2005. He’s nice and well-meaning chap, but he doesn’t seem to know much about what’s going on in the College. |

|
Professor Sir Ian Kennedy LLD, FBA, FKC, FUCL, Hon.DSc(Glasgow), Hon.FRCP is vice-president of the College. Among many other things he is Emeritus Professor of Health Law, Ethics and Policy at University College London. He was Chair of the Healthcare Commission until 2003, when it merged with other regulators to form the Care Quality Commission. No doubt he can’t be blamed for the recent parlous performence of the CQC. |

|
Professor Aidan Halligan MA, MD, FRCOG, FFPHM, MRCPI Since March 200y he has been Director of Education at University College London Hospitals. From 2003 until 2005, he was Deputy Chief Medical Officer for England, with responsibility for issues of clinical governance, patient safety and quality of care. He’s undoubtedly a well-meaning man, but so focussed on his (excellent) homelessness project that he seems immune to the company he keeps. Perhaps the clue lies in the fact that when I asked him what he thought of Lansely’s health bill, he seemed to quite like it. |
It seems to me to be incomprehensible that these three people should be willing to sign a letter in the British Medical Journal in defence of the College, with co-signatories George Lewith (about whom much has been written here) and the homeopath Christine Glover. In so doing, they betray medicine, they betray reason, and most important of all, they betray patients. Perhaps they have spent too much time sitting on very important committees and not enough time with patients.
The stated aims of the College sound good.
"A force that combines scientific knowledge, clinical expertise and the patient’s own perspective. A force that will re-define what good medicine means − renewing the traditional values of service, commitment and compassion and creating a more holistic, patient-centred, preventative approach to healthcare."
But what they propose to do about it is, with a few exceptions, bad. They try to whip up panic by exaggerating the crisis in the NHS. There are problems of course, but they result largely from under-funding (we still spend less on healthcare than most developed countries), and from the progressive involvement of for-profit commercial companies, like Capita. The College has the wrong diagnosis and the wrong solution. How do they propose to take care of an aging population? Self-care and herbal medicines seem to be their solution.
|
The programme for the College’s workshop shows it was run by herbalist Simon Mills and by Dick Middleton an employee of the giant herbal company, Schwabe. You can see Middleton attempting to defend misleading labelling of herbal products on YouTube, opposed by me. |
|
It seems that the College of Medicine are aiding and abetting the destruction of the National Health Service. That makes me angry.(here’s why)
I can end only with the most poignant tweet in the run up to the passing of the Health and Social Care Act. It was from someone known as @HeardInLondon, on March 15th
"For a brief period during 20th century, people gave a fuck & looked after each other. Unfortunately this proved unprofitable." #SaveOurNHS
— HeardinLondon (@HeardinLondon) March 13, 2012
"For a brief period during 20th century, people gave a fuck and looked after each other. Unfortunately this proved unprofitable."
Unprofitable for Crapita, that is.
Follow-up
5 May 2012. Well well, if there were any doubt about the endarkenment values of the College, I see that the Prince of Wales, the Quacktitioner Royal himself, gave a speech at the College’s conference.
"”I have been saying for what seems a very long time that until we develop truly integrated systems – not simply treating the symptoms of disease, but actively creating health, putting the patient at the heart of the process by incorporating our core human elements of mind, body and spirit – we shall always struggle, in my view, with an over-emphasis on mechanistic, technological approaches.”
Of course we all want empathy. The speech, as usual, contributes precisely nothing.
12 June 2012. Oh my, how did I manage to miss the fact the the College’s president, Professor Sir Graeme Catto, is also a Crapita eployee. It’s over a year since he was apponted to Capita’s clinical governance board he says "  In a rapidly growing health and wellbeing marketplace, delivering best practice in clinical governance is of utmost importance. I look forward to working with the team at Capita to assist them with continuing to adopt a best in class approach.". The operative word is "marketplace".
In a rapidly growing health and wellbeing marketplace, delivering best practice in clinical governance is of utmost importance. I look forward to working with the team at Capita to assist them with continuing to adopt a best in class approach.". The operative word is "marketplace".
There’s been no official announcement, but four more of Westminster’s courses in junk medicine have quietly closed.
For entry in 2011 they offer
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Complementary Medicine (B255) | 3FT Hon BSc |
| Complementary Medicine (B301) | 4FT Hon MHSci |
| Complementary Medicine: Naturopathy (B391) | 3FT Hon BSc |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSci |
| Nutritional Therapy (B400) | 3FT Hon BSc |
But for entry in 2012
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSc |
At the end of 2006, Westminster was offering 14 different BSc degrees in seven flavours of junk medicine. In October 2008, it was eleven. This year it’s eight, and next year only four degrees in two subjects. Since "Integrated Health" was ‘merged’ with Biological Sciences in May 2010, two of the original courses have been dropped each year. This September there will be a final intake for Nutrition Therapy and Naturopathy. That leaves only two, Chinese Medicine (acupuncture and (Western) Herbal Medicine.
The official reason given for the closures is always that the number of applications has fallen. I’m told that the number of applications has halved over the last five or six years. If that’s right, it counts as a big success for the attempts of skeptics to show the public the nonsense that’s taught on these degrees. Perhaps it is a sign that we are emerging from the endarkenment.
Rumour has it that the remaining degrees will eventually close too. Let’s hope so. Meanwhile, here is another helping hand.
There is already quite a bit here about the dangers of Chinese medicine, e.g. here and, especially, here. A submission to the Department of Health gives more detail. There has been a lot on acupuncture here too. There is now little doubt that it’s no more than a theatrical, and not very effective, placebo. So this time I’ll concentrate on Western herbal medicine.
Western Herbal Medicine
Herbal medicine is just a branch of pharmacology and it could be taught as such. But it isn’t. It comes overlaid with much superstitious nonsense. Some of it can be seen in slides from Edinburgh Napier University (the difference being that Napier closed that course, and Westminster hasn’t)
Even if it were taught properly, it wouldn’t be appropriate for a BSc for several reasons.
First, there isn’t a single herbal that has full marketing authorisation from the MHRA. In other words, there isn’t a single herb for which there is good evidence that it works to a useful extent.
Second, the fact that the active principals in plants are virtually always given in an unknown dose makes them potentially dangerous. This isn’t 1950s pharmacology. It’s 1920s pharmacology, dating from a time before methods were worked out for standardising the potency of natural products (see Plants as Medicines).
Third, if you are going to treat illness with chemicals, why restrict yourself to chemicals that occur in plants?
It was the herbal medicine course that gave rise to the most virulent internal complaints at the University of Westminster. These complaints revealed the use of pendulum dowsing by some teachers on the course and the near-illegal, and certainly dangerous, teaching about herbs in cancer.
Here are a few slides from Principles of Herbal Medicine(3CT0 502). The vocabulary seems to be stuck in a time warp. When I first started in the late 1950s, words like tonic, carminative, demulcent and expectorant were common Over the last 40 years all these words have died out in pharmacology, for the simple reason that it became apparent that there were no such actions. But these imaginary categories are still alive and well in the herbal world.
There was a lecture on a categories of drugs so old-fashioned that I’ve never even heard the words: "nervines". and "adaptogens".
 |
  |
 |
The "tonics" listed here seem quite bizarre. In the 1950s, “tonics” containing nux vomica (a small dose of strychnine) and gentian (tastes nasty) were common, but they vanished years ago, because they don’t work. None of those named here even get a mention in NCCAM’s Herbs-at-a-glance. Oats? Come on! |
|
The only ‘relaxant’ here for which there is the slightest evidence is Valerian. I recall tincture of Valerian in a late 1950s pharmacy. It smells terrible, According to NCCAM
Not much, for something that’s been around for centuries. And for chamomile
None of this near-total lack of evidence is mentioned on the slides. |
 |
What about the ‘stimulants‘? Rosemary? No evidence at all. Tea and coffee aren’t medicine (and not very good stimulants for me either).
|
Ginseng, on the other hand, is big business. That doesn’t mean it works of course. NCCAM says of Asian ginseng (Panax Ginseng).
|
 |
Thymoleptics – antidepressants are defined as "herbs that engender a feeling of wellbeing. They uplift the spirit, improve the mood and counteract depression".
Oats, Lemon balm, Damiana, Vervain. Lavender and Rosemary are just old bits of folklore
|
 |
The only serious contender here is St John’s Wort. At one time this was the prize exhibit for herbalists. It has been shown to be as good as the conventional SSRIs for treatment of mild to moderate depression. Sadly it has turned out that the SSRIs are themselves barely better than placebos. NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
"Adaptogens" are another figment of the herbalists’ imaginations. They are defined in the lecture thus.
|

|
Well, it would be quite nice if such drugs existed. Sadly they don’t.
- The evidence for using astragalus for any health condition is limited. High-quality clinical trials (studies in people) are generally lacking.
Another lecture dealt with "stimulating herbs". No shortage of them, it seems.

Well at least one of these has quite well-understood effects in pharmacology, ephedrine, a sympathomimetic amine. It isn’t used much because it can be quite dangerous, even with the controlled dose that’s used in real medicine. In the uncontrolled dose in herbal medicines it is downright dangerous.

|

|

|
|
This is what NCCAM says about Ephedra
- An NCCAM-funded study that analyzed phone calls to poison control centers found a higher rate of side effects from ephedra, compared with other herbal products.
- Other studies and systematic reviews have found an increased risk of heart, psychiatric, and gastrointestinal problems, as well as high blood pressure and stroke, with ephedra use.
- According to the U.S. Food and Drug Administration (FDA), there is little evidence of ephedra’s effectiveness, except for short-term weight loss. However, the increased risk of heart problems and stroke outweighs any benefits.
It seems that what is taught in the BSc Herbal Medicine degree consists largely of folk-lore and old wives’ tales. Some of it could be quite dangerous for patients.
A problem for pharmacognosists
While talking about herbal medicine, it’s appropriate to mention a related problem, though it has nothing to do with the University of Westminster.
My guess is that not many people have even heard of pharmacognosy. If it were not for my humble origins as an apprentice pharmacist in Grange Road, Birkenhead (you can’t get much more humble than that) I might not know either.
Pharmacognosy is a branch of botany, the study of plant drugs. I recall inspecting powered digitalis leaves under a microscope. In Edinburgh, in the time of the great pharmacologist John Henry Gaddum, medical students might be presented in the oral exam with a jar of calabar beans and required to talk about their anticholinesterase effects of the physostigmine that they contain.
The need for pharmacognosy has now all but vanished, but it hangs on in the curriculum for pharmacy students. This has engendered a certain unease about the role of pharmacognists. They often try to justify their existence by rebranding themselves as "phytotherapists". There are even journals of phytotherapy. It sounds a lot more respectable that herbalism. At its best, it is more respectable, but the fact remains that there no herbs whatsoever that have well-documented medical uses.
The London School of Pharmacy is a case in point. Simon Gibbons (Professor of Phytochemistry, Department of Pharmaceutical and Biological Chemistry). The School of Pharmacy) has chosen, for reasons that baffle me, to throw in his lot with the reincarnated Prince of Wales Foundation known as the “College of Medicine“. That organisation exists largely (not entirely) to promote various forms of quackery under the euphemism “integrated medicine”. On their web site he says "Western science is now recognising the extremely high value of herbal medicinal products . . .", despite the fact that there isn’t a single herbal preparation with efficacy sufficient for it to get marketing authorisation in the UK. This is grasping at straws, not science.
The true nature of the "College of Medicine" is illustrated, yet again, by their "innovations network". Their idea of "innovation" includes the Bristol Homeopathic Hospital and the Royal London Hospital for Integrated medicine, both devoted to promoting the utterly discredited late-18th century practice of giving people pills that contain no medicine. Some "innovation".
It baffles me that Simon Gibbons is willing to appear on the same programme as Simon Mills and David Peters, and George Lewith. Mills’ ideas can be judged by watching a video of a talk he gave in which he ‘explains’ “hot and cold herbs”. It strikes me as pure gobbledygook. Make up your own mind. He too has rebranded himself as "phytotherapist" though in fact he’s an old-fashioned herbalist with no concern for good evidence. David Peters is the chap who, as Clinical Director of the University of Westminster’s ever-shrinking School of Quackery, tolerates dowsing as a way to select ‘remedies’.
The present chair of Pharmacognosy at the School of Pharmacy is Michael Heinrich. He, with Simon Gibbons, has written a book Fundamentals of pharmacognosy and phytotherapy. As well as much good chemistry, it contains this extraordinary statement
“TCM [traditional Chinese medicine] still contains very many remedies which were selected by their symbolic significance rather than their proven effects; however this does not mean that they are all ‘quack’remedies! There may even be some value in medicines such as tiger bone, bear gall, turtle shell, dried centipedes, bat dung and so on. The herbs, however, are well researched and are becoming increasingly popular as people become disillusioned with Western Medicine.”
It is irresponsible to give any solace at all to the wicked industries that kill tigers and torture bears to extract their bile. And it is simple untrue that “herbs are well-researched”. Try the test,
A simple test for herbalists. Next time you encounter a herbalist, ask them to name the herb for which there is the best evidence of benefit when given for any condition. Mostly they refuse to answer, as was the case with Michael McIntyre (but he is really an industry spokesman with few scientific pretensions). I asked Michael Heinrich, Professor of Pharmacognosy at the School of Pharmacy. Again I couldn’t get a straight answer. Usually, when pressed, the two things that come up are St John’s Wort and Echinacea. Let’s see what The National Center for Complementary and Alternative Medicine (NCCAM) has to say about them. NCCAM is the branch of the US National Institutes of Health which has spent around a billion dollars of US taxpayers’ money on research into alternative medicine, For all that effort they have failed to come up with a single useful treatment. Clearly they should be shut down. Nevertheless, as an organisation that is enthusiastic about alternative medicine, their view can only be overoptimistic.
For St John’s Wort . NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
For Echinacea NCCAM says
- Study results are mixed on whether echinacea can prevent or effectively treat upper respiratory tract infections such as the common cold. For example, two NCCAM-funded studies did not find a benefit from echinacea, either as Echinacea purpurea fresh-pressed juice for treating colds in children, or as an unrefined mixture of Echinacea angustifolia root and Echinacea purpurea root and herb in adults. However, other studies have shown that echinacea may be beneficial in treating upper respiratory infections.
If these are the best ones, heaven help the rest.
Follow-up
Almost all the revelations about what’s taught on university courses in alternative medicine have come from post-1992 universities. (For readers not in the UK, post-1992 universities are the many new univerities created in 1992, from former polytechnics etc, and Russell group universities are the "top 20" research-intensive universities)
It is true that all the undergraduate courses are in post-1992 universities, but the advance of quackademia is by no means limited to them. The teaching at St Bartholomew’s Hospital Medical School, one of the oldest, was pretty disgraceful for example, though after protests from their own students, and from me, it is now better, I believe.

Quackery creeps into all universities to varying extents. The good ones (like Southampton) don’t run "BSc" degrees, but it still infiltrates through two main sources,
The first is via their HR departments, which are run by people who tend to be (I quote) "credulous and moronic" when it comes to science.
The other main source is in teaching to medical students. The General Medical Council says that medical students must know something about alterantive medicine and that’s quite right, A lot of their patients will use it. The problem is that the guidance is shockingly vague .
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
In many medical schools, the information that medical students get is quite accurate. At UCL and at King’s (London) I have done some of the familiarisation myself. In other good medical schools, the students get some shocking stuff. St Bartholomew’s Hospital medical School was one example. Edinburgh University was another.
But there is one Russell group university where alternative myths are propagated more than any other that I know about. That is the University of Southampton.
In general, Southampton is a good place, I worked there for three years myself (1972 – 1975). The very first noise spectra I measured were calculated on a PDP computer in their excellent Institute of Sound and Vibration Research, before I wrote my own programs to do it.
But Southanpton also has a The Complementary and Integrated Medicine Research Unit . Oddly the unit’s web site, http://www.cam-research-group.co.uk, is not a university address, and a search of the university’s web site for “Complementary and Integrated Medicine Research Unit” produces no result. Nevertheless the unit is “within the School of Medicine at the University of Southampton”
Notice the usual euphemisms ‘complementary’ and ‘integrated’ in the title: the word ‘alternative’ is never used. This sort of word play is part of the bait and switch approach of alternative medicine.
The unit is quite big: ten research staff, four PhD students and two support staff It is headed by George Lewith.
Teaching about alternative medicine to Southampton medical students.
The whole medical class seems to get quite a lot compared with other places I know about. That’s 250 students (210 on the 5-year course plus another 40 from the 4-year graduate-entry route).
Year 1: Lecture by David Owen on ‘holism’ within the Foundation Course given to all 210 medical students doing the standard (5-year) course.
Year 2: Lecture by Lewith (on complementary medicine, focusing on acupuncture for pain) given within the nervous systems course to the whole medical student year-group (210 students).
Year 3 SBOM (scientific basis of medicine) symposium: The 3-hour session (“Complementary or Alternative Medicine: You Decide”). I’m told that attendance at this symposium is often pretty low, but many do turn up and all of them are officially ‘expected’ to attend.
There is also an optional CAM special study module chosen by 20 students in year 3, but also a small number of medical students (perhaps 2 – 3 each year?) choose to do a BMedSci research project supervised by the CAM research group and involving 16-18 weeks of study from October to May in Year 4. The CAM research group also supervise postgraduate students doing PhD research.
As always, a list of lectures doesn’t tell you much. What we need to know is what’s taught to the students and something about the people who teach it. The other interesting question is how it comes about that alternative medicine has been allowed to become so prominent in a Russell group university. It must have support from on high. In this case it isn’t hard to find out where it comes from. Here are some details.
Year 1 Dr David Owen
David Owen is not part of Lewith’s group, but a member of the Division of Medical Education headed by Dr Faith Hill (of whom, more below). He’s one of the many part-time academics in this area, being also a founder of The Natural Practice .
Owen is an advocate of homeopathy (a past president of the Faculty of Homeopathy). Homeopathy is, of course, the most barmy and discredited of all the popular sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes it).
And he’s also a member of the British Society of Environmental Medicine (BSEM). That sounds like a very respectable title, but don’t be deceived. It is an organisation that promotes all sorts of seriously fringe ideas. All you have to do is notice that the star speaker at their 2011 conference was none other than used-to-be a doctor, Andrew Wakefield, a man who has been responsible for the death of children from measles by causing an unfounded scare about vaccination on the basis of data that turned out to have been falsified. There is still a letter of support for Wakefield on the BSEM web site.
The BSEM specialises in exaggerated claims about ‘environmental toxins’ and uses phony allergy tests like kinesiology and the Vega test that misdiagnose allergies, but provide en excuse to prescribe expensive but unproven nutritional supplements, or expensive psychobabble like "neuro-linguistic programming".
Other registered "ecological physicians" include the infamous Dr Sarah Myhill, who, in 2010, was the subject of a damning verdict by the GMC, and Southampton’s George Lewith.
If it is wrong to expose medical students to someone who believes that dose-response curves have a negative slope (the smaller the dose the bigger the effect -I know, it’s crazy), then it is downright wicked to expose students to a supporter of Andrew Wakefield.
David Owen’s appearance on Radio Oxford, with the indomitable Andy Lewis appears on his Quackometer blog.
Year 2 Dr George Lewith
Lewith is a mystery wrapped in an enigma. He’s participated in some research that is quite good by the (generally pathetic) standards of the world of alternative medicine.
In 2001 he showed that the Vega test did not work as a method of allergy diagnosis. "Conclusion Electrodermal testing cannot be used to diagnose environmental allergies", published in the BMJ .[download reprint].
In 2003 he published "A randomized, double-blind, placebo-controlled proving trial of Belladonna 30C” [download reprint] that showed homeopathic pills with no active ingredients had no effects: The conclusion was "”Ultramolecular homeopathy has no observable clinical effects" (the word ultramolecular, in this context, means that the belladonna pills contained no belladonna).
In 2010 he again concluded that homeopathic pills were no more than placebos, as described in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). [download reprint]
What i cannot understand is that, despite his own findings, his private practice continues to prescribe the Vega machine and continues to prescribe homeopathic pills. And he continues to preach this subject to unfortunate medical students.
Lewith is also one of the practitioners recommended by BSEM. He’s a director of the "College of Medicine". And he’s also an advisor to a charity called Yes To Life. (see A thoroughly dangerous charity: YesToLife promotes nonsense cancer treatments).
3rd year Student Selected Unit
The teaching team includes:
- David Owen – Principal Clinical Teaching Fellow SoM, Holistic Physician
- George Lewith – Professor of Health Research and Consultant Physician
- Caroline Eyles – Homeopathic Physician
- Susan Woodhead – Acupuncturist
- Elaine Cooke – Chiropractic Practitioner
- Phine Dahle – Psychotherapist
- Keith Carr – Reiki Master
- Christine Rose – Homeopath and GP
- David Nicolson – Nutritionalist
- Shelley Baker – Aromatherapist
- Cheryl Dunford – Hypnotherapist
- Dedj Leibbrandt – Herbalist
More details of the teaching team here. There is not a single sceptic among them, so the students don’t get a debate, just propaganda.
In this case. there’s no need for the Freedom of Information Act. The handouts. and the powerpoints are on their web site. They seem to be proud of them
Let’s look at some examples
Chiropractic makes an interesting case, because, in the wake of the Singh-BCA libel case, the claims of chiropractors have been scrutinised as never before and most of their claims have turned out to be bogus. There is a close relationship between Lewith’s unit and the Anglo-European Chiropractic College (the 3rd year module includes a visit there). In fact the handout provided for students, Evidence for Chiropractic Care , was written by the College. It’s interesting because it provides no real evidence whatsoever for the effectiveness of chiropractic care. It’s fairly honest in stating that the view at present is that, for low back pain, it isn’t possible to detect any difference between the usefulness of manipulation by a physiotherapist, by an osteopath or by a chiropractor. Of course it does not draw the obvious conclusion that this makes chiropractic and osteopathy entirely redundant -you can get the same result without all the absurd mumbo jumbo that chiropractors and osteopaths love, or their high-pressure salesmanship and superfluous X-rays. Neither does it mention the sad, but entirely possible, outcome that none of the manipulations are effective for low back pain. There is, for example, no mention of the fascinating paper by Artus et al [download reprint]. This paper concludes
"symptoms seem to improve in a similar pattern in clinical trials following a wide
variety of active as well as inactive treatments."
This paper was brought to my attention through the blog run by the exellent physiotherapist, Neil O’Connell. He comments
“If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery.”
This sort of critical thinking is conspicuously absent from this (and all the other) Southampton handouts. The handout is a superb example of bait and switch: No nonsense about infant colic, innate energy or imaginary subluxations appears in it.
Acupuncture is another interesting case because there is quite a lot of research evidence, in stark contrast to the rest of traditional Chinese medicine, for which there is very little research.
|
There is a powerpoint show by Susan Woodhead (though it is labelled British Acupuncture Council). The message is simple and totally uncritical. It works. |

|
In fact there is now a broad consensus about acupuncture.
(1) Real acupuncture and sham acupuncture have been found to be indistinguishable in many trials. This is the case regardless of whether the sham is a retractable needle (or even a toothpick) in the "right" places, or whether it is real needles inserted in the "wrong" places. The latter finding shows clearly that all that stuff about meridians and flow of Qi is sheer hocus pocus. It dates from a pre-scientific age and it was wrong.
(2) A non-blind comparison of acupuncture versus no acupuncture shows an advantage for acupuncture. But the advantage is usually too small to be of any clinical significance. In all probability it is a placebo effect -it’s hard to imagine a more theatrical event than having someone in a white coat stick long needles into you, like a voodoo doll. Sadly, the placebo effect isn’t big enough to be of much use.
Needless to say, none of this is conveyed to the medical students of Southampton. Instead they are shown crude ancient ideas that date from long before anything was known about physiology as though they were actually true. These folks truly live in some alternative universe. Here are some samples from the acupuncture powerpoint show by Susan Woodhead.



Well this is certainly a "different diagnostic language", but no attempt is made to say which one is right. In the mind of the acupuncurist it seems both are true. It is a characteristic of alternative medicine advocates that they have no difficulty in believing simultaneously several mutually contradictory propositions.
As a final exmple of barminess, just look at the acupuncture points (allegedly) on the ear The fact that it is a favoured by some people in the Pentagon as battlefield acupuncture, is more reminiscent of the mad general, Jack D. Ripper, in Dr Strangelove than it is of science.

There is an equally uncritical handout on acupuncture by Val Hopwood. It’s dated March 2003, a time before some of the most valuable experiments were done.
The handout says "sham acupuncture
is generally less effective than true acupuncture", precisely the opposite of what’s known now. And there are some bits that give you a good laugh, always helpful in teaching. I like
“There is little doubt that an intact functioning nervous system is required for acupuncture to produce
analgesia or, for that matter, any physiological changes”
and
Modern techniques: These include hybrid techniques such as electro-acupuncture . . . and Ryadoraku [sic] therapy and Vega testing.
Vega testing!! That’s been disproved dozens of times (not least by George Lewith). And actually the other made-up nonsense is spelled Ryodoraku.
It’s true that there is a short paragraph at the end of the handout headed "Scientific evaluation of acupuncture" but it doesn’t cite a single reference and reads more like excuses for why acupuncture so often fails when it’s tested properly.
Homeopathy. Finally a bit about that most boring of topics, the laughable medicine that contains no medicine, homeopathy. Caroline Eyles is a member for the Society of Homeopaths, the organisation that did nothing when its members were caught out in the murderous practice of recommending homeopathy for prevention of malaria. The Society of Homeopaths also endorses Jeremy Sherr, a man so crazy that he believes he can cure AIDS and malaria with sugar pills.
The homeopathy handout given to the students has 367 references, but somehow manages to omit the references to their own boss’s work showing that the pills are placebos. The handout has all the sciencey-sounding words, abused by people who don’t understand them.
"The remedy will be particularly effective if matched to the specific/particular characteristics of the individual (the ‘totality’ of the patient) on all levels, including the emotional and mental levels, as well as just the physical symptoms. ‘Resonance’ with the remedy’s curative power will then be at it’s [sic] best."
The handout is totally misleading about the current state of research. It says
"increasing clinical research confirms it’s [sic] clinical effectiveness in treating patients, including babies and animals (where a placebo effect would be hard to justify)."
|
The powerpont show by Caroline Eyles shows all the insight of a mediaeval vitalist |
|
Anyone who has to rely on the utterly discredited Jacques Benveniste as evidence is clearly clutching at straws. What’s more interesting about this slide the admission that "reproducibility is a problem -oops, an issue" and that RCTs (done largely by homeopaths of course) have "various methodological flaws and poor external validity". You’d think that if that was the best that could be produced after 200 yours, they’d shut up shop and get another job. But, like aging vicars who long since stopped believing in god, but are damned if they’ll give up the nice country rectory, they struggle on, sounding increasingly desperate.
How have topics like this become so embedded in a medical course at a Russell group university?
The details above are a bit tedious and repetitive. It’s already established that hardly any alternative medicine works. Don’t take my word for it. Check the web site of the US National Center for Complementary and Alternative Medicine (NCCAM) who, at a cost of over $2 billion have produced nothing useful.
A rather more interesting question is how a good university like Southampton comes to be exposing its medical students to teaching like this. There must be some powerful allies higher up in the university. In this case it’s pretty obvious who thay are.
Professor Stephen Holgate MD DSc CSc FRCP FRCPath FIBiol FBMS FMed Sci CBE has to be the primary suspect, He’s listed as one of Southampton’s Outstanding Academics. His work is nothing to do with alternative medicine but he’s been a long term supporter of the late unlamented Prince of Wales’ Foundation, and he’s now on the advisory board of it’s successor, the so called "College of Medicine" (for more information about that place see the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health, and also Don’t be deceived. The new “College of Medicine” is a fraud and delusion ). His description on that site reads thus.
"Stephen Holgate is MRC Clinical Professor of Immunopharmacology at the University of Southampton School of Medicine and Honorary Consultant Physician at Southampton University Hospital Trust. He is also chair of the MRC’s Populations and Systems Medicine Board. Specialising in respiratory medicine, he is the author of over 800 peer-reviewed papers and contributions to scientific journals and editor of major textbooks on asthma and rhinitis. He is Co-Editor of Clinical and Experimental Allergy, Associate Editor of Clinical Science and on the editorial board of 25 other scientific journals."
Clearly a busy man. Personally I’m deeply suspicious of anyone who claims to be the author of over 800 papers. He graduated in medicine in 1971, so that is an average of over 20 papers a year since then, one every two or three weeks. I’d have trouble reading that many, never mind writing them.
Holgate’s long-standing interest in alternative medicine is baffling. He’s published on the topic with George Lewith, who, incidentally, is one of the directors of the "College of Medicine"..
It may be unkind to mention that, for many years now, I’ve been hearing rumours that Holgate is suffering from an unusually bad case of Knight starvation.
The Division of Medical Education appears to be the other big source of support for. anti-scientific medicine. That is very odd, I know, but it was also the medical education people who were responsible for mis-educating medical students at. St. Bartholomew’s and at Edinburgh university. Southampton’s Division of Medical Education has a mind-boggling 60 academic and support staff. Two of them are of particular interest here.
Faith Hill is director of the division. Her profile doesn’t say anything about alternative medicine, but her interest is clear from a 2003 paper, Complementary and alternative medicine: the next generation of health promotion?. The research consisted of reporting anecdotes from interviews of 52 unnamed people (this sort of thing seems to pass for research in the social sciences). It starts badly by misrepresenting the conclusions of the House of Lords report (2000) on CAM. Although it comes to no useful conclusions, it certainly shows a high tolerance of nonsensical treatments.
Chris Stephens is Associate Dean of Medical Education & Student Experience. His sympathy is shown by a paper he wrote In 2001, with David Owen (the homeopath, above) and George Lewith: Can doctors respond to patients’ increasing interest in complementary and alternative medicine?. Two of the conclusions of this paper were as follows.
"Doctors are training in complementary and alternative medicine and report benefits both for their patients and themselves"
Well, no actually. It wasn’t true then, and it’s probably even less true now. There’s now a lot more evidence and most of it shows alternative medicine doesn’t work.
"Doctors need to address training in and practice of complementary and alternative medicine within their own organisations"
Yes they certainly need to do that.
And the first thing that Drs Hill and Stephens should do is look a bit more closely about what’s taught in their own university, I hope that this post helps them,
Follow-up
4 July 2011. A correspondent has just pointed out that Chris Stephens is a member of the General Chiropractic Council. The GCC is a truly pathetic pseudo-regulator. In the wake of the Simon Singh affair it has been kept busy fending off well-justified complaints against untrue claims made by chiropractors. The GCC is a sad joke, but it’s even sadder to see a Dean of Medical Education at the University of Southampton being involved with an organisation that has treated little matters of truth with such disdain.
A rather unkind tweet from (ex)-chiropractor @RichardLanigan.
“Chris is just another light weight academic who likes being on committees. Regulatory bodies are full of them”
An email yesterday alerted me to YesToLife. This outfit seemed to me to be so dangerous that a word of warning is in the public interest.
Their own description says “YES TO LIFE is a new charitable initiative to open up a positive future for people with cancer in the UK by supporting an integrative* approach to cancer care”. That sounds sort of cuddly but lets look below the surface.
As so often, the funding seems to have been raised as the result of the death of an unfortunate 23 year old woman. Instead of putting the money into real research, yet another small charity was formed. My correspondent pointed out that “I came across them at St Pancras Station on Friday afternoon — they had a live DJ to draw in the crowd and were raising funds through bucket collections”. No doubt many people just see the word ‘cancer’ and put money in the bucket, without realising that their money will be spent on promoting nonsensical and ineffective treatments.
The supporters list.
The list of supporters tells you all you need to know, if you are familiar with the magic medicine business, though it might look quite convincing if you don’t know about the people. Sadly the list starts with some celebrities (I didn’t know before that Maureen Lipman was an enthusiast foir quackery -how very sad). But never mind the air-head celebrities. The more interesting supporters come later.
- Dr Rosy Daniel of Health Creation is an old friend. After I complained about her promotion of some herbal concoction called Carctol to “heal cancer”, she was reprimanded by Trading Standards for breaching the Cancer Act 1939, and forced to change the claims (in my view she should have neen prosecuted but, luckily of her, Trading Standards people are notoriously ineffective). There is, of course not the slightest reason to to think that Carctol works (download Carctol: Profits before Patients?). Read also what Cancer Research UK say about carctol.
Dr Daniel is also well known because ran a course that was, for one year, accredited by the University of Buckingham. But once the university became aware of the nonsense that was being taught on the course, they first removed her as the course director, and then removed accreditation from the course altogether. She then tried to run the course under the aegis of the Prince’s Foundation for Integrated Health, but even they turned her down. Now it is running as a private venture, and is being advertised by YesToLife. - Boo Armstrong, “Chief Executive of The Prince’s Foundation for Integrated Health and Founder and Executive Director GetWellUK”. The web site is out of date since the Prince’s Foundation shut its doors a year ago. She runs a private company, GetWellUK, that was responsible for a very poor study of alternative medicine in Northern Ireland. So she has a vested interest in promoting it. See Peter Hain and GetwellUK: pseudoscience and privatisation in Northern Ireland
- Professor George Lewith. This is beginning to look like the usual list of suspects. I’ve had cause to write twice about the curious activities of Dr Lewith. See Lewith’s private clinic has curious standards, in 2006, and this year George Lewith’s private practice. Another case study. The make up your own mind about whether you’d trust him.
- Dr Michael Dixon OBE, Chairman NHS Alliance and Medical Director The Prince’s Foundation for Integrated Health. Again the job description is a year out of date. You can read about Dr Dixon at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’. He seems to be a well meaning man for whom no new-age idea is too barmy.
In fact both Dixon and Lewith have moved to a reincarnation of the Prince’s Foundation known as the “College of Medicine” (actually it’s a couple of offices in Buckingham Street). See Don’t be deceived. The new “College of Medicine” is a fraud and delusion.
It seems to me incomprehensible that people such as Sir Graeme Catto, Sir Cyril Chantler and Sir Muir Grey are willing to be associated with people who behave like this. - Charlotte Grobien, Managing Director, Give it Away. This seems to be a fund-raising organisation that has supported YesToLife. The lesson seems to be, never give money to fundraisers unless you know exactly where your money is going.
The Help Centre
YesToLife has a help centre. But beware, There is no medical person there. Just Traditional Chinese medicine (rather dangerous), acupuncture, osteopath and naturopathy (which means, roughly, do nothing and hope for the best).
Patrick Holford,
There can be no better indication of the standard of advice to be expected from YesToLife than the fact they are advertising a lecture by Holford, with the enticing title "Say no to cancer"."Through learning about the effects of diet and nutrition, people with cancer or at risk of developing cancer can be empowered to say Yes to Life and No to Cancer". Would that it were so easy. It will cost you £15.00.
Just in case there is still nobody who has heard of Holford, he is the media nutritionist who has an entire chapter devoted to him in Ben Goldacre’s Bad Science book, He has a whole website that has exposed his dubious advice, the excellent HolfordWatch. And you can find quite a lot about him on this blog. Try, for example, Patrick Holford’s CV: the strange case of Dr John Marks, and Response to a threatening letter from Mr Holford, or Holford’s untruthful and unsubstantiated advertisement
The treatments directory
Now we get to the truly scary bit of YesToLife, their treatment directory. Try searching for ‘cancer type’ and then "breast (metastatic)".. We find no mention of the advances in understanding of the genetics of breast cancer, nor ot real therapies like tamoxifen. What we find are four "alternative treatments".
- Neuroimmunomodulation Therapy It sounds impressive until you learn that its only proponent is a an 82 year old Venezuelan doctor with a clinic in Caracas. Even YesToLife doesn’t pretend that there is any evidence that it works
- Vitamin C Therapy The old chestnut cure-all Vitamin C Again even YesToLife don’t pretend there is any good evidence but it is still offered; treatment cost £3140.00 (what? Vitamin C is very cheap indeed)
- Dendritic Cell Therapy Said by YesToLife to be "well-researched", though that isn’t so for breast cancer (metastatic). Although possibly not as barmy as the other things that are recommended, it is nevertheless not shown to be effective for any sort of cancer,
- Gerson Therapy It is a sign of the extreme unreliability of advice given by YesToLife that they should still recommend anything as totally discredited as Gerson Therapy.Although YesToLife describes it as "well-researched" that is simply not true: there are no proper clinical trials. Cancer Research UK say
"Overall, there is no evidence to show that Gerson therapy works as a cure for cancer. "
"Available scientific evidence does not support claims that Gerson therapy can treat cancer. It is not approved for use in the United States. Gerson therapy can be very harmful to your health. Coffee enemas have been linked to serious infections, dehydration, constipation, colitis (inflammation of the colon), and electrolyte imbalances. In some people, particular aspects of the diet such as coffee enemas have been thought to be responsible for their death."Recommended reading: The (Not-So-)Beautiful (Un)Truth about the Gerson protocol and cancer quackery, by David Gorski (breast cancer surgeon, writing in Science-based Medicine.
Conclusion
The information supplied by YesToLife is more likely to kill you than to cure you.
The next time you see somebody collecting for a "cancer charity" be very careful before you give them money.
Follow-up
November 2012. It gets worse.
I had an email from someone who was distressed because a friend was trying to raise £15,000 to cover the cost of treatments recommended by YesToLife. The treatment is high-dose intravenous Vitamin C infusion. This is pure quackery. There isn’t the slightest reason to think it will affect the course of cancer, or the wellbeing of the patient. It is exploitation of the desperate. My heart sinks at the thought that a “charity” can be quite so wicked.
|
Professor George Lewith is perhaps the most prominent advocate of alternative medicine within quackademia, at least in Russell Group University. He claims to be a member of “The Complementary and Integrated Medicine Research Unit is within the School of Medicine at the University of Southampton.”. |
The URL for this unit is actually http://www.cam-research-group.co.uk/. Strangely, though, a search of Southampton University’s own web site for “Complementary and Integrated Medicine Research Unit” yields very little information about this unit.
But Lewith does not spend all of his time on his academic duties. He also spends time in London at his private practice, at the Centre for Complementary and Integrated Medicine. This practice, I discovered in 2006, was selling to patients that well known method for misdiagnosing food intolerance, the Vega test. It was doing so despite the fact that Lewith himself had written a paper that concluded that the Vega machine does not work, The paper was in the British Medical Journal, 2001;322:131-4. It concludes “Electrodermal testing cannot be used to diagnose environmental allergies”. This history is recorded in Lewith’s private clinic has curious standards.
Dr Lewith was in the news again recently when he published a paper that showed (yet again) that homeopathic pills work no better than placebo. No surprise there of course. The paper has been described here, in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again).
So we can congratulate Lewith for being one of the few members of the magic-medicine community to have published papers of reasonable quality that show that neither homeopathy nor the Vega test work. In fact there was nothing novel in the conclusions about the Vega machine. It has been debunked again and again.
The BBC’s Inside Out programme in 2003 found that when the Vega test was taken in three different branches of Holland and Barrett, the results were quite different every time. The reporter was advised to by a total of 20 different supplements, but got different advice from every store.
In 2006, the test was destroyed again in, of all places, the Daily Mail which published ‘The great allergy con‘.
In 2011, BBC’s Watchdog programme looked again at food intolerance tests, with results as crazy as before. Holland & Barrett said “In light of this report, however, we have instructed The UK Health Partnership to investigate the findings and review their current training practices”. That’s odd, because in 2001 they had said “”In light of the issues raised, we are already carrying out a full review of the services that HSL provide.” So not much progress there.
What is rather more surprising is to find that Dr Lewith, having himself shown that neither the Vega test nor homeopathy work, continues to sell both to patients in his private practice.
I recently heard from a young student about her experiences when she went to Prof Lewith’s private practice. If you want to read her letter in full, download the pdf. Some quotations from it suffice to tell the tale.
“I had suffered from CFS/ME for nearly 8 years when on March 18th 2009 I had my first appointment with doctor Lewith”
“We talked for 7 to 10 minutes about my history and gave a very brief outline of my medical past. I did feel that this was a bit rushed”
“He said that he would treat me with a mixture of homeopathic medicine and conventional treatments and then hooked me up to a machine to determine any food intolerances.”
“He put me off all dairy products and said that he would send me some homeopathic remedies and food supplements”
“Having suffered with the illness for so long and having been involved with the conventional practices for treating ME with no relief I went to Dr Lewith desperate. I left this first consultation a little shocked at the rushed pace and a little wary of homeopathy but determined to carry on. ”
“I waited for my remedies in the post but only the food supplements and the blood test results arrived.”
“On April 8th 2009, I went back for my 30 minute follow up consultation. We talked briefly about how I was doing. Dr Lewith exclaimed that I looked so much better than last time and that the treatments that he had sent me had obviously worked. I assumed he meant the food supplements. It quickly transpired that he meant the homeopathic drops that I had never received. I suggested that I was probably better than last time because I was not recently recovering from tonsillitis. My confidence was immediately lost as I felt I was being coerced into thinking that the drugs he had provided were the reason for my recovery. Someone with knowledge of ME should be aware that a sufferer is not in a permanent state of ill health but generally that they follow what is known as ‘Boom and Bust’. I was going through a good patch, which after 8 years of being ill was the normal pattern. This was a maximum 5 minute conversation.”
“He hooked me up to the machine again still without any real explanation. ”
“I cancelled my next appointment with Dr Lewith having completely lost faith in his methods. I subsequently received two packages of drugs by post which I have returned. Neither at the consultation nor with the packages of drugs was there any explanation of what each drug was prescribed to achieve.”
“It was soon after that Lewith was chasing me for payment of the cancelled appointment and the homeopathic drugs that I had sent back. This was a total of £230. I had already spent nearly £300. I refused to pay as I did not feel that I had received the proper medical care that is expected of a GP.”
“He threatened to lay a claim against me at the small claims court.”
“I submitted both a Defence and Counterclaim to his action against me.”
“We went to court yesterday [January 17 2011] where Dr Lewith did not attend. ”
“He failed to submit witness statements and a Defence to my Counterclaim. The judge struck the case off and my costs awarded against Dr Lewith.”
“Conventional medicine had not been successful in helping me with ME and at 20 years old and at university I was desperate for a cure. I feel that complementary medicine takes advantage of people in my situation – I witnessed extortionate fees, blatant coercion to believe that it was working and blasé professionalism”
In response to a subsequent enquiry, the student told me
“He never told me what the homeopathic drugs were or what they were meant to do. When I received them I sent them straight back.”
“I am pretty sure that I was given general vitamins and minerals and some magnesium (if that makes sense?)”
|
 A Vega machine |
The student also paid £85 for an ATP metabolism test, done by Acumen, a private company run by Dr John McLaren-Howard. This test allegedly found defects in ATP metabolism on the basis of which the student was charged £91.91 for CoQ10 tablets. Neither the test, nor CoQ10, have any verified usefulness for her condition.
Here’s the bill for the homeopathic pills prescribed by Lewith.
These are the facts. Make of them what you will. At a cost of over £500, no good was done.
It isn’t surprising that Lewith’s claim was dismissed by the court.

The College of Medicine
We notice that Professor Lewith plays is vice-chair of the “College of Medicine” that has arisen from the ashes of the Prince’s Foundation for Integrated Health (for more details see Don’t be deceived. The new “College of Medicine” is a fraud and delusion). That organisation is supposed to be devoted to “patient-centered medicine”. The reader can judge whether the case related here is a good example.
It is often said that one reason that people go to alternative practitioners is because real medicine can do nothing for them. That, only too often, is the case. People get desperate and clutch at straws. That is bad enough even in cases where the alternative practitioner believes sincerely, if wrongly, that their treatments work.
For the alternative practitioner to prescribe things which he knows full well don’t work, is, perhaps, rather worse.
Follow-up
Just as this post was about to go up, George Lewith popped up again in a BCC piece about how expectations affect the perception of pain (something that has been known for years). Lewith is quoted as saying “It completely blows cold randomised clinical trials, which don’t take into account expectation.” This comment shows a total misunderstand of how a randomised trial works. It is all explained properly by Majikthyse, in The wrong end of the stick
Just for fun, here is a discussion that I had with Lewith on Channel 4 News, as edited (not by me) for YouTube.
I’m bored stiff with that barmiest of all the widespread forms of alternative medicine, homeopathy. It is clearly heading back to where it was in 1960, a small lunatic fringe of medicine. Nevertheless it’s worth looking at a recent development.
A paper has appeared by that arch defender of all things alternative, George Lewith.
The paper in question is “Homeopathy has clinical benefits in rheumatoid arthritis patients that are attributable to the
consultation process but not the homeopathic remedy: a randomized controlled clinical trial”, Sarah Brien, Laurie Lachance, Phil Prescott, Clare McDermott and George Lewith. [read it here]. It was published in Rheumatology.
Conclusion. Homeopathic consultations but not homeopathic remedies are associated with clinically relevant benefits for patients with active but relatively stable RA.
So yet another case where the homeopathic pills turn out the same as placebos, Hardly surprising since the pills are the same as the placebos, but it’s always good to hear it from someone whose private practice sells homeopathy for money.
The conclusion isn’t actually very novel, because Fisher & Scott (2001) had already found nine years ago that homeopathy was ineffective in reducing the symptoms if joint inflammation in RA. That is Peter Fisher, the Queens’ homeopathic physician, and Clinical Director of the Royal Hospital for Integrated Medicine (recently renamed to remove ‘homeopathy’ from its title). That paper ends with the remarkable statement [download the paper]
- "Over these years we have come to believe that conventional RCTs [randomised controlled trials] are unlikely to capture the possible benefits of homeopathy . . . . It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response."
That seemed to me at the time to amount to an admission that it was all ‘placebo effect’, though Fisher continues to deny that this is the case.
"Homeopathy has clinical benefits in rheumatoid arthritis patients" -the title says. But does it?
In fact this is mere spin. What the paper actually shows is that an empathetic consultation has some benefit (and even this is inconsistent). This is hardly surprising, but there is really not the slightest reason to suppose that the benefit, such as it is, has anything whatsoever to do with homeopathy.
Homeopathy, non-specific effects and good medicine is the title of an excellent editorial, in the same issue of Rheumatology, by Edzard Ernst. He points out that "The recognition of the therapeutic value of an empathetic consultation is by no means a new insight". Any therapy that provides only non-specific effects is unacceptable. Any good doctor provides that and, when it exists, real effective treatments too.
Lewith’s private clinic

The Centre for Complementary and Integrated Medicine is run by Drs Nick Avery and George Lewith. It is always a bit galling to real scientists, who often work 60 hours a week or more to get results, that people like Lewith get a professorial salary (in his case from the University of Southampton) but still have time to make more money by doing another job at the same time.
Avery is a homeopath. I wonder whether we can now look forward to the web site being changed in the near future so that there is a clear statement that the pills have no effect?
There is, at least, now no longer any mention of the Vega test on Lewith’s site. That is a test for food allergy that has been shown again and again to be fraudulent. The Environmental medicine page is brief, and avoids making any claims at all. It now contains the somewhat coy statement
“Specific food avoidance regimes are a controversial area and one in which there may be conflict between conventionally trained allergists and CAM practitioners.”
However the page about fibromyalgia still mentions homeopathy favourably. And it still fails to refer to my reanalysis of one of the positive trials which revealed a simple statistical mistake.
The front page of their web site boasts that "Dr George Lewith is now one of The Lifestyle 50!". " The Times, in an article on September 6th 2008, included George Lewith in The Lifestyle 50, this newspaper’s listing of the “top 50 people who influence the way we eat, exercise and think about ourselves”. Dr Lewith is included in the Alternatives category". It doesn’t mention that this is an honour he shares with such medical luminaries as Gillian ("I’m not a doctor") McKeith, Jennifer Ariston and the Pope,
But let’s end this on a happier note. There is one thing that I agree with wholeheartedly. Lewith says
"The use of bottled water seems to me to be a multi-billion pound industry, based on some of the cleverest marketing that I have ever encountered. There is absolutely no evidence that bottled water is any safer, better, or more “energising” than the water you get from the tap."
No connection of course with the multi-million pound industry of selling homeopathic water by clever marketing.
Some limitations of the paper by Brien et al.
Like any good trial, this one defined in advance a primary and secondary outcome.
The primary outcome was ACR20. which means the propertion of patients that showed an improvement of at least 20% of the number of tender and swollen joint counts and 20% improvement in 3 of the 5 remaining ACR core set measures (see Felsen 1995). Although it isn’t stressed in the paper, there was no detectable difference between consultation vs no consultation for this primary outcome.
The secondary outcome was 28-joint DAS (DAS-28), tender and swollen joint count, disease severity, pain, weekly patient
and physician GA and pain, and inflammatory markers (see, for example, Stucki. 1996). It was only on this outcome that an effect was seen between consultation and no consultation. The "effect size" (standardized mean score differences, adjusted for baseline differences) was an improvement of 0.7 in DAS-28 score, which runs on a scale from 0 – 10. Although this improvement is probably real (statistically significant), it is barely bigger than improvement of 0.6 which is said to be the smallest change that is clinically significant (Stucki. 1996).
Not only is the improvement by the consultation small in clinical terms. It is also rather inconsistent. for example Table 6 shows that the consultation seemded to result in a detectable effect on swollen joint count, but not on tender joint count. Neither was there any significant effect of the consultation on the response to “considering all the ways your arthritis affects you, please make a vertical line to show how well you are now”. There appeared to be an improvement on “negative mood score”, but not on “positive mood score”. Effects of the consultation on pain scores was marginal at best.
It seems to me that the conclusion that the consultation process helps patients, though not entirely implausible, gets marginal support from this study. It may be real, but if so it isn’t a large effect.
Like most alternative medicine advocates, the authors of this paper make the mistake of confusing caring and curing. Caring is good if there is nothing else that can be done (as is only too often the case). But what patients really want is cures and they’ll never get that from an empathetic consultation.
The problem of Human Resources
What does all this mean for alternative medicine on the NHS? Nobody denies the desirability of empathy. In fact it is now talked about so much that there is a danger that scientific medical education will be marginalised. My own experience of the NHS is that most doctors are quite good at empathy, without any need to resort to hocus pocus like homeopathy and all the myriad forms of mythical medicine.
It must be said that Drs Avery and Lewith have had proper medical training. Their views on alternative medicine seem bizarre to me, but at least they should do no great harm. Sadly, the same can’t be said for the majority of homeopaths who have no medical training and who continue to andanger the public by recommending sugar pills for anything from malaria to Dengue fever. People like that have no place in the NHS. Indeed some are in jail.
Not long ago, I was invited to tour the oncology wards at UCL hospital with their chief spiritual healer, Angie Buxton-King. Although in her private practice she offers some pretty bizarre services like healing humans and animals at a distance, I had the impression that on the wards she did a pretty good job holding hands with people who were nervous about injections and chatting to people in for their third lot of chemotherapy. I asked if she would object to being called a "supportive health care worker" rather than a spiritual healer. Somewhat reluctantly she said that she wouldn’t mind that. But it can’t be done because of the absurd box-ticking mentality of HR departments. There is no job-description for someone who holds hands with patients, and no formal qualifications. On the other hand, if you are sufficiently brainless, you can tick a box for a healer. Once again I wish that HR departments would not hinder academic integrity.
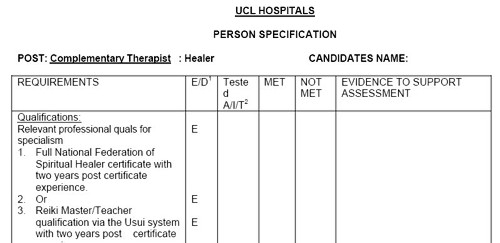
Follow-up
Steven Novella, at Science-Based medicine, has also written about this paper.
The Prince of Wales’ Foundation for Integrated Health shut down amidst scandal in April 2010. In July, we heard that a new “College of Medicine” was to arise from its ashes. It seemed clear from the people involved that the name “College of Medicine” would be deceptive.
Now the College of Medicine has materialised, and it is clear that one’s worst fears were well justified.

At first sight, it looks entirely plausible and well-meaning. Below the logo one reads
“There is a new force in medicine. A force that brings patients, doctors, nurses and other health professionals together, instead of separating them into tribes.”
"That force is the new College of Medicine. Uniquely, it brings doctors and other health professionals together with patients and scientists.”
It is apparent from the outset that the well-meaning words fall into the trap described so clearly by James May (see What ‘holistic’ really means). It fails to distinguish between curing and caring.
As always, the clue lies not in the words, but in the people who are running it.
Who is involved?
After a bit of digging on the web site, you find the names of the people on the Science Council of the “College of Medicine”, The preamble says
“Good medicine must be grounded in good science as well as compassion. The College’s Science Council brings a depth of knowledge from many senior figures.”
But then come the names. With the odd exception the “science council” is like a roll-call of quacks, the dregs left over from the Prince’s Foundation. The link (attached to each name) gives the College’s bio, My links tell a rather different story.
-
Professor George Lewith You’ll find plenty about George Lewith on this blog.
-
Professor Mustafa Djamgoz Superficially respectable but seduced by ‘ancient wisdom’ He once wrote to me "There are many ‘eastern’ remedies (such as acupuncture that we witnessed dismissed 25 year ago) that work. ". Well it isn’t as simple as that.
-
Professor Simon Gibbons A phytochemist with exaggerated ideas of what you can get from plants.
-
Professor Jane Plant A respectable geochemist who became obsessed with alternative medicine, Read about her here,
-
Dr Peter Fisher The Queen’s Homeopathic Physician. Advocate of the most discreded of all forms of quackery. Lots about him here.
-
Dr Michael Loughlin A post-modernist-influenced theorist who hates Ben Goldacre. Read about him here.
-
Dr Hugh MacPherson An acupuncturist and fellow traveller of the Prince of Wales. Read here.
-
Professor Andrew Miles I’m sorry to see him in this company after the good job he did in ejecting quacks at the University of Buckingham.
-
Simon Mills A man who thinks herbs can be classified as "hot"and "cold", See here and here
-
Professor Nicola Robinson Head of the Centre for Complementary Healthcare & Integrated Medicine,Thames Valley University A well known advocate of unevidenced treatments. Try Googling her
-
Dr Catherine Zollman Another hangover from the Princes’ Foundation, and believer in magic medicine
It seems that the "Scientific Council" of the College of Medicine could more properly be called an "Antiscientific Council".
There are a few gaps in this table, to be filled in soon. One can guarantee that a great deal more will appear about the College on the web, very soon.
The Governing Council of the College is equally replete with quacks (plus a few surprising names). It has on it, for example, a spiritual healer (Angie-Buxton King), a homeopath (Christine Glover), a herbalist (Michael McIntyre). Westminster University’s king of woo (David Peters), not to mention the infamous Karol Sikora. Buxton-King offers a remarkable service to heal people or animals at a distance.
Meanwhile, it seemed worthwhile to provide a warning that the title of the College is very deceptive. It hides an agenda that could do much harm.
It is, quite simply, the Prince of Wales by stealth.
Follow-up
28 October 2010
Professor Sir Graeme Catto, who has, disgracefully, allowed his name to be used as president of this “College” has said to me “There are real problems in knowing how to care for folk with chronic conditions and the extent of the evidence base for medicine is pretty limited”.
Yes of course that is quite true. There are many conditions for which medicine can still do little. There is a fascinating discussion to be had about how best to care for them. The answer to that is NOT to bring in spiritual healers and peddlers of sugar pills to deceive patients with their fairy stories. The “College of Medicine” will delay and pervert the sort of discussion that Catto says, rightly, is needed.
29 October 2010
I need a press card. I see that the BMJ also had a piece about the “College of Medicine” yesterday: Prince’s foundation metamorphoses into new College of Medicine, by Nigel Hawkes. He got the main point right there in the title.
As was clear since July, the driving force was Michael Dixon, Devon GP and ex medical director of the Prince’s Foundation. Hawkes goes easy on the homeopaths and spiritual healers, but did spot something that I can’t find on their web site. The “Faculties” will include
“in 2011, neuromusculoskeletal care. Two of the six strong faculty members for this specialty are from the British Chiropractic Association, which sued the author Simon Singh for libel for his disobliging remarks about the evidence base for their interventions.”
The College certainly picks its moment to endorse chiropractic, a subject that is in chaos and disgrace after they lost the Singh affair.
One bit of good news emerges from Hawkes’ piece, There is at least one high profile doubter in the medical establishment, Lord (John) Walton (his 2000 report on CAM was less than blunt, and has been widely misquoted by quacks) is reported as saying, at the opening ceremony
“I’m here as a sceptic, and I’ve just told my former houseman that,” he said. The target of the remark was Donald Irvine, another former GMC president and a member of the new college’s advisory council.”
31 October 2010. I got an email that pointed out a remarkable service offered by a member of College’s Governing Council. Angie Buxton-King, a “spiritual healer” employed by UCLH seems to have another web site, The Beacon of Healing Light that is not mentioned in her biography on the College’s site. Perhaps it should have been because it makes some remarkable claims. The page about distant healing is the most bizarre.
Absent Healing/Distant Healing
"Absent healing is available when it is not possible to visit the patient or it is not possible for the patient to be brought to our healing room. This form of healing has proved to be very successful for humans and animals alike."
"We keep a healing book within our healing room and every night spend time sending healing to all those who have asked for it. We have found that if a picture of the patient is sent to us the healing is more beneficial, we also require a weekly update to monitor any progress or change in the patients situation. Donations are welcome for this service."
I wonder what the Advertising Standards people make of the claim that it is “very successful”? I wonder what the president of the College makes of it? I’ve asked him.
Other blogs about the “College of Medicine”
30 October 2010. Margaret McCartney is always worth reading. As a GP she is at the forefront of medicine. She’s written about the College in The Crisis in Caring and dangerous inference. She’s also provided some information about a "professional member" of the College of Medicine, in ..and on Dr Sam Everington, at the Bromley by Bow Centre….
It is one of the more insulting things about alternative medicine addicts that they claim to be the guardians of caring (as opposed to curing), They are not, and people like McCartney and Michael Baum are excellent examples.
Prince of Wales to become honorary president of the “College of Medicine?”
Last night I heard a rumour that the Prince of Wales is, despite all the earlier denials, to become Honorary President of the “College”. If this is true, it completes the wholesale transformation of the late, unlamented, Prince’s Foundation for Integrated Medicine into this new “College”. Can anybody take it seriously now?
Text messages to Graeme Catto and Michael Dixon, inviting them to deny the rumour, have met with silence.
Herbal nonsense at the College
29 July 2011. I got an email from the College if Medicine [download it]. It contains a lot of fantasy about herbal medicines, sponsered by a company that manufactures them. It is dangeroous and corrupt.
In July 2008 I wrote an editorial in the New Zealand Medical Journal (NZMJ), at the request of its editor.
The title was Dr Who? deception by chiropractors. It was not very flattering and it resulted in a letter from lawyers representing the New Zealand Chiropractic Association. Luckily the editor of the NZMJ, Frank Frizelle, is a man of principle, and the legal action was averted. It also resulted in some interesting discussions with disillusioned chiropractors that confirmed one’s worst fears. Not to mention revealing the internecine warfare between one chiropractor and another.
This all occurred before the British Chiropractic Association sued Simon Singh for defamation. The strength of the reaction to that foolhardy action now has chiropractors wondering if they can survive at all. The baselessness of most of their claims has been exposed as never before. No wonder they are running scared. The whole basis of their business is imploding.
Needless to say chiropractors were very cross indeed. Then in February 2009 I had a polite email from a New Zealand chiropractor, David Owen, asking for help to find one of the references in the editorial. I’d quoted Preston Long as saying
"Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
And I’d given the reference as
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10
I’d found the quotation, and the reference, in Ernst’s 2005 article, The value of Chiropractic, but at the time I couldn’t find the Journal of Quality Healthcare. I did find the same article on the web. At least the article had the same title, the same author and the same quotation. But after finding, and reading, the article, I neglected to change the reference from J Quality Health Care to http://skepticreport.com/sr/?p=88. I should have done so and for that I apologise.
When I asked Ernst about the Journal of Quality Healthcare, he couldn’t find his copy of the Journal either, but he and his secretary embarked on a hunt for it, and eventually it was found.

![]()
|
It turns out that Journal of Quality Healthcare shut down in 2004, without leaving a trace on the web, or even in the British Library. It was replaced by a different journal, Patient Safety and Quality Healthcare (PSQH) A reprint was obtained from them. It is indeed the same as the web version that I’d read, and it highlighted the quotation in question. The reprint of the original article, which proved so hard to find, can be downloaded here. |

|
The full quotation is this
"Sixty-two clinical neurologists from across Canada, all certified members of the Royal College of Physicians and Surgeons, issued a warning to the Canadian public, which was reported by Brad Stewart, MD. The warning was entitled Canadian Neurologists Warn Against Neck Manipulation. The final conclusion was that endless non-scientific claims are being made as to the uses of neck manipulation(Stewart, 2003). They need to be stopped. The public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45."
I have often condemned the practice of citing papers without reading them (it is, of course, distressingly common), so I feel bad about this, though I had in fact read the paper in question in its web version. I’m writing about it because I feel one should be open about mistakes, even small ones.
I’m also writing about it because one small section of the magic medicine community seems to think they have nailed me because of it. David Owen, the New Zealand chiropractor, wrote to the editor of the NZMJ, thus.
|
The quote [in question] is the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45. Long PH. Stroke and Manipulation. J Quality Health Care. 2004:3:8-10 This quote actually comes from the following blog article http://www.skepticreport.com/medicalquackery/strokespinal.htm [DC the URL is now http://skepticreport.com/sr/?p=88] I have attached all my personal communications with Colquhoun. They demonstrate this is not a citation error. Prof Colquhoun believes the origin of the quote doesn’t matter because Long was quoting from a Canadian Neurologists’ report (this is also incorrect). As you can see he fails to provide any evidence at all to support the existance [sic] of the “J Quality Health Care.” Colquhoun ‘s belief that my forwarding this complaint is me “resorting to threats” is the final nail in the coffin. If he had any leg to stand on where is the threat? This may seem pedantic but it surely reflects a serious ethical breach. Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility? Incidentally, at the end of the article, conflicts of interest are listed as none. As Colquhoun is a Professor of Pharmacology and much of his research funding no doubt comes from the pharmaceutical industry how can he have no conflict of interest with therapies that do not advocate the use of drugs and compete directly against the billions spent on pain medications each year? If I may quote Colquhoun himself in his defence of his article (Journal of the New Zealand Medical Association, 05-September-2008, Vol 121 No 1281) I’ll admit, though, that perhaps ‘intellect’ is not what’s deficient in this case, but rather honesty. David Owen |
Financial interests
Well, here is a threat: I’m exposed as a shill of Big Pharma. ". . . much of his funding no doubt comes from the pharmaceutical industry". I can’t count how many times this accusation has been thrown at me by advocates of magic medicine. Oddly enough none of them has actually taken the trouble to find out where my research funding has come from. None of them even knows enough about the business to realise the extreme improbability that the Pharmaceutical Industry would be interested in funding basic work on the stochastic properties of single molecules. They fund only clinicians who can help to improve their profits,
The matter of funding is already on record, but I’ll repeat it now. The media ‘nutritional therapist’, Patrick Holford, said, in the British Medical Journal
“I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry “
To which my reply was
” Oh dear, Patrick Holford really should check before saying things like “I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry”. Unlike Holford, when I said “no competing interests”, I meant it. My research has never been funded by the drug industry, but always by the Medical Research Council or by the Wellcome Trust. Neither have I accepted hospitality or travel to conferences from them. That is because I would never want to run the risk of judgements being clouded by money. The only time I have ever taken money from industry is in the form of modest fees that I got for giving a series of lectures on the basic mathematical principles of drug-receptor interaction, a few years ago.”
I spend a lot of my spare time, and a bit of my own money, in an attempt to bring some sense into the arguments. The alternative medicine gurus make their livings (in some cases large fortunes) out of their wares.
So who has the vested interest?
Does chiropractic actually cause stroke?
As in the case of drugs and diet, it is remarkably difficult to be sure about causality. A patient suffers a vertebral artery dissection shortly after visiting a chiropractor, but did the neck manipulation cause the stroke? Or did it precipitate the stroke in somebody predisposed to one? Or is the timing just coincidence and the stroke would have happened anyway? There has been a lot of discussion about this and a forthcoming analysis will tackle the problem of causality head-on,
My assessment at the moment, for what it’s worth, is that there are some pretty good reasons to suspect that neck manipulation can be dangerous, but it seems that serious damage is rare.
In a sense, it really doesn’t matter much anyway, because it is now apparent that chiropractic is pretty well discredited without having to resort to arguments about rare (though serious) effects. There is real doubt about whether it is even any good for back pain (see Cochrane review), and good reason to think that the very common claims of chiropractors to be able to cure infant colic, asthma and so on are entirely, ahem, bogus. (See also Steven Novella, ebm-first, and innumerable other recent analyses.)
Chiropractic is entirely discredited, whether or not it may occasionally kill people.
Complaint sent to UCL
I had an enquiry about this problem also from my old friend George Lewith. I told him what had happened. Soon after this, a complaint was sent to Tim Perry and Jason Clarke, UCL’s Director and Deputy Director of Academic Services. The letter came not from Lewith or Owen, but from Lionel Milgom. Milgrom is well known in the magic medicine community for writing papers about how homeopathy can be “explained” by quantum entanglement. Unfortunately for him, his papers have been read by some real physicists and they are no more than rather pretentious metaphors. See, for example, Danny Chrastina’s analysis, and shpalman, here. Not to mention Lewis, AP Gaylard and Orac.
|
Dear Mr Perry and Mr Clark, I would like to bring to your attention an editorial (below) that appeared in the most recent issue of the New Zealand Medical Journal. In it, one of your Emeritus Professors, David Colquhoun, is accused of a serious ethical breach, and I quote – “Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility?” Professor Colquhoun is well-known for writing extensively and publicly excoriating many forms of complementary and alternative medicine, particularly with regard to the alleged unscientific nature and unethical behaviour of its practitioners. Professor Colquhoun is also a voluble champion for keeping the libel laws out of science. While such activities are doubtlessly in accord with the venerable Benthamite liberal traditions of UCL, I am quite certain hypocrisy is not. And though Professor Colquhoun has owned up to his error, as the NZMJ’s editor implies, it leaves a question mark over his credibility. As custodians of the college’s academic quality therefore, you might care to consider the possible damage to UCL’s reputation of perceived professorial cant; emeritus or otherwise. Yours Sincerely Dr Lionel R Milgrom |
So, as we have seen, the quotation was correct, the reference was correct, and I’d read the article from which it came I made a mistake in citing the original paper rather than the web version of the same paper..
I leave it to the reader to judge whether this constitutes a "serious ethical breach", whether I’d slipped in an "unsupported statement", and whether it constitutes "hypocrisy"
Follow-up
It so happens that no sooner was this posted than there appeared Part 2 of the devastating refutation of Lionel Milgrom’s attempt to defend homeopathy, written by AP Gaylard. Thanks to Mojo (comment #2) for pointing this out.
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
On 23rd May 2009, the Financial Times magazine published a six-page cover story about pseudo-scientific degrees by Richard Tomkins. The online version has the text but doesn’t do justice to the prominence that it was given. The print version had a much better title too, The Retreat from Reason. This article, which was some time in gestation, appeared shortly afte the last degree in homeopathy in the UK closed its doors. So perhaps it should have been called The Return of Reason. What’s interesting is that it has become commonplace for the mainstream newspapers to print articles like this and to dump some of their whackier lifestyle articles.

The print version had a much better title too, The Retreat from Reason, with a two-page spread..

They published the entire ‘Patients’ Guide to Magic Medicine‘ as a sidebar on page 4.

To these has now been added, inspired by Jack of Kent,
Libel: A very expensive remedy, to be used only when you have no evidence. Appeals to alternative practitioners because truth is irrelevant
One part of the article that I particularly enjoyed is this.
George Lewith, professor of health research at the University of Southampton’s medical school, is also director of the Centre for Complementary and Integrated Medicine, a private practice with clinics in Southampton and London’s West End, so it is no surprise that he is ready to speak out in support of complementary therapies. In fact, Southampton University – a member of the elite Russell Group – does not offer degree courses in complementary medicine, but Lewith defends the idea of offering them in principle, on the basis that, done properly, they produce better-trained practitioners. “Without the new universities’ involvement we might be faced with the quackery we saw in the 1940s and 1950s, when these people were outside medicine and were practising in an alternative fringe culture,” he says.
Sorry George, you are still an “alternative fringe culture”. And universities are realising that, and shutting down courses all over the place.
A response in the Finacial Times
The FT published one response in its letter column, A bilious attack on complementary medicine.
“Sir, Like many journalists, Richard Tomkins has been over-impressed by the scientific credentials of Professors David Colquhoun and Edzard Ernst as they carry on their absurdly over-stated, arrogant and irresponsible campaign against complementary medicine (“The retreat of reason”, May 23)”
and then the trump card
“Absence of evidence is not evidence of absence”
That’s the line used by quacks again and again and again (see, for example, integrative baloney @ Yale). I guess they have never heard of type 1 and type 2 errors. But that is a bit technical for homeopaths, so put it more simply. There is a quite remarkable absence of evidence for tooth fairies. So they must exist. Get it?
The letter is from Allen Parrott of Yeovil. Could that be the Allen Parrott of the British Acupuncture Accreditation Board? If so he is “is an adult educationist who was Dean of Adult and Community Education at Yeovil College and a lecturer in the School of Education at Exeter University. As well as his work for the Board, he is currently working as an educational adviser for the Kent, Surrey and Sussex Deanery in the NHS.”. So no reason to worry about the standards of education in Yeovil, then.
Two days ago I wrote NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself
Now the official ‘guidance’ is out, and it is indeed quite as bad as the draft.
The relevant bits now read thus.
- Offer one of the following treatment options, taking into account patient preference: an exercise programme, a course of manual therapy or a course of acupuncture. Consider offering another of these options if the chosen treatment does not result in satisfactory improvement.
- Consider offering a structured exercise programme tailored to the person:
- This should comprise of up to a maximum of 8 sessions over a period of up to 12 weeks.
- Offer a group supervised exercise programme, in a group of up to 10 people.
- A one-to-one supervised exercise programme may be offered if a group programme is not suitable for a particular person.
- Consider offering a course of manual therapy, including spinal manipulation, comprising up to a maximum of nine sessions over a period of up to 12 weeks
- Consider offering a course of acupuncture needling comprising up to a maximum of 10 sessions over a period of up to 12 weeks.
The summary guidance still doesn’t mention chiropractic explicitly, just a coy reference to “spinal manipulation”. At a time when the British Chiropractic Association is busy trying to suppress free speech via the law courts, I guess it isn’t surprising that they don’t like to use the word.
The bias in the recommendations is perhaps not surprising because the guidance development group had a heavy representation from alternative medicine advocates, and of people with a record of what, is, in my view, excessive tolerance of mumbo-jumbo.
Royal College of General Practitioners (RCGP) played a large part in writing the guidance. That is an organisation thar has steadfastly refused to make any sort of sensible statement of policy about magic medicine. It isn’t long since I was told by a senior person at the RCGP that there was nothing odd about neuro-linguistic programming. That does not bode well.
Professor Martin Underwood, Professor of Primary Care Research Warwick Medical School, University of Warwick. Underwood chaired the guidance development group. Martin Underwood is also a GP in Coventry See also the British Osteopathic Association. Underwood was lead author of the BEAM trial (download reprint). It is well worth reading the comments on this trial too. It was a randomised trial (though not, of course, blind).
|
Our main aim was to estimate, for patients consulting their general practitioner with back pain, the effectiveness of adding the following to best care in general practice: a class based exercise programme (“back to fitness”), a package of treatment by a spinal manipulator (chiropractor, osteopath, or physiotherapist), or manipulation followed by exercise Conclusions |
In other words, none of them worked very well. The paper failed to distinguish between manipulation by physiotherapists, chiropractors and osteopaths and so missed a valuable chance to find out whether there is an advantage to employing people from alternative medicine (the very problem that this NICE guidance should have dealt with)
Steve Vogel, another member of the guidance development group, is an osteopath. Osteopathy has cast off its shady origins better than chiropractic, but it remains a largely evidence-free zone, and is still usually classified as alternative medicine.
Peter Dixon DC FCC FBCA is chairman of the General Chiropractic Council and founder of Peter Dixon Associates. They run six chiropractic clinics. The claims made by these clinics on their web site are mostly related to musculo-skeletal conditions (not, all spine-related however). But they also include
“Chiropractic is also suitable for relieving the symptoms of stress, and optimizing the way the body works is one of the best ways of enhancing health and wellbeing.”
I wonder how they could justify that claim? Then we get
A chiropractor is always willing to discuss individual conditions or answer questions in order to assess whether chiropractic may be of benefit.
Thanks for the invitation. I accepted it. After the first two phone calls, I had learned all I needed.
The first of Peter Dixon’s clinics that I called, was asked about my son who was suffeiing from perpetual colic. I asked for advice. I was put through to the chiropractor. Here are some extracts from the conversation.
“I think now it’s termed irritable baby syndrome. . . . . We’ve found chiropractic is very effective for colic . . . . £50 up to 3/4 hour which would involve taking a case history, examining the baby, with regard to seeing how the joints in the spine work because often colic is down to, er um, faulty movement patterns in the spine. We deal with an awful lot of things to do with the frame -how the spine moves -and it’s often problems with the way that the bones of the spine move in infants and babies that is the underlying cause in colicky symptoms. . . usually on the whole, I’ve shot myself in the foot by saying this in the past, if there are -um when I say back problems they’re usually temporary issues -when they are there the response for most babies is quite quick . . . it depends on how it’s related to what’s gone on in the birth process -there is usually some traumatic cause and it usually sets up a problem in the upper neck or the mid-back and that will drive those colic symptoms. . . . Yes it’s quite a straightforward thing we just check the baby’s spine and see if it’s problem we can deal with or not.”
Yes, I think you just shot yourself in the foot again. I have no idea in what fraction of cases a chiropractor would fail to claim that it was a case that they could deal with. At least that possibility was envisaged. But when I asked where he’d refer me to in such case I was told it might be a result of bottle feeding -“what they consume”. So I expect it would have been sent to some sort of “nutritional therapist” who would have used one of their usual battery of unreliable tests for food allergies.
I tried a second clinic in Peter Dixon’s empire and asked if chiropractic could help with asthma.”It can do, depending on what type of asthma you have". After some questions I was asked
“Do you have any general aches and pains otherwise, any tension .problems round the rib cage or thoracic spine . . . There are two things we’d look as chiropractors as to whether we could help or not and that would include the tension round the rib cage -in any type of asthma you’ll become tight round the rib cage and merely by keeping that area loose you’d help to stop the asthma from becoming quite as bad. And the second part is we’d look at the neck area with you to see if there is any restriction there -which houses the nerve supply to the lungs which can be indicated in some asthma cases also.”
I was invited to come for a free screen, so I asked if it usually worked quickly, “It depends what the problem is but you’d need a course I suspect”. £45 for the first appointment then £28 per session. “In most cases you’d need to look at a six to eight session course”.
Would anyone with experience of crying babies or of asthma like to comment on these proposed treatments? They are not my idea of evidence-based treatments and I find it quite surprising that someone who sponsors them is thought appropriate to write guidance for NICE.
This sort of ‘sting’ always makes me feel a bit uneasy, but it seems to be the only way to find out what actually goes on. And what goes on has all the appearance of classic bait and switch. You go in for your backache, and before you know where you are you are being sold a course of treatment to stop your baby crying.
Media follow-up after the NICE announcement
Sadly, I heard that the Today programme (my favourite news programme) was pretty wet. if only their science reporting was as good as their politics reporting.
The 27th May was certainly pretty busy for me, Apart from a couple of local paper interviews, this is what happened,
Sky News TV. Richard Suchet and two cameraman came to UCL and filmed a lot of stuff out of which a 20 second clip was used. And then they grumble that they don’t make money.
BBC TV 6 o’clock News. Similar, but at least only two people this time. Both TV stations spent ages showing pictures of people having needles pushed into them and very little time discussing the problems. A pathetically bad attempt at science reporting. Radio, on the whole, did much better
BBC Three Counties Radio (09.20) Host Ronnie Barbour, The daytime talk shows may be appalling to some of us, but the hosts did a far better job of airing the problems than TV [download the mp3].
Radio 5 Live Victoria Derbyshire [download the mp3]
BBC Radio Sheffield (12.05) was the best talk show by far. First speaker was Steve Vogel, the osteopath from the guidance development group. Although invited by the rather sensible host, Rony, to respond to the idea that a secondary consequence of the guidance would be to introduce hocus-pocus, he steadfastly refused to answer the question. At the end a rather sensible GP summed up the view from the coalface. [play the mp3]
Radio 4 PM programme This excellent early evening news programme is run by Eddie Mair. It was the best interview yet. The other side was put by Martin Underwood, chair of the guidance development group [play the mp3]
Underwood said “the evidence shows that it [acupuncture] works”. I disagree. The evidence shows that acupuncture, in a non-blind comparison with no acupuncture shows a small, variable additional effect that doesn’t last and is of marginal clinical significance, That is not what I call “works”. Underwood then indulges in the subgroup analysis fallacy by asserting that a few people get a large benefit from acupuncture. Or perhaps a few people just happen to get better that day. I was not convinced.
More 4 News TV 20.20 was an interview, with the other side being put by my old friend, George Lewith.
During the introduction, an acupuncturist. Lisa Sherman, ‘explained’ acupuncture in the usual sort of utterly meaningless words that illustrate perfectly the problem.
George Lewith said that “we don’t have a good pretend form of acupuncture”. “We don’t have a good placebo and we can demonstrate that acupuncture is literally twice as effective as conventional care”. The first is simply nonsense: huge efforts have gone into developing good controls in acupuncture studies (see, for example, Barker Bausell’s book, Snake Oil Science). And I hope that George will send the references for his “twice as effective” claim. It seems to me to be nothing short of preposterous.
My conclusions
So what went wrong?
One problem could be regarded as medical arrogance. The fact is that the problem of low back pain has not been solved, either by drugs or anything else. It is a failure of medicine (and of pharmacology). That should be the premise of all discussions, and it smacks of arrogance not to tell people straight out. Of course there are some cases when causes can be identified, and perhaps remedied, usually by surgery, but these are the exceptions not the rule.
One consequence of the inability of medicine to help much is that patients get desperate, and willing to try anything. And of course if they happen to have a remission, that is attributed to the treatment, however preposterous that treatment may have been. Conditions like back pain that come and go unpredictable are a gift for quacks.
Another consequence, for researchers rather than patients, is to clutch at straws. Even small and inconsistent effects are seized on as ‘successes’. This phenomenon seems to be part of the reason for the NICE guidance. Another reason is, almost certainly, the grinding of axes by some of the people who wrote it.
What should be done now?
Professor Sir Michael Rawlins is a sensible chap. He cares about evidence, But it does seem that in this case, he might have taken his eye off the ball, for once. In my opinion, he should restore the reputation of NICE by withdrawing this guidance and starting again.
Follow-up
An interesting document has come my way. It shows the responses of the guidance group to the consultation on the draft guidance. Many people made comments not unlike mone, but they were all brushed aside in a way that looks to me rather partisan. The document appears to have vanished from NICE’s web site, but you can download it here.
Friday 29th May. The Times prints a letter from two consultants in pain medicine, Joan Hestor and Stephen Ward. It says, inter alia
“As experienced pain specialists we feel that NICE has lost its way in publishing these guidelines.”
“We are saddened that NICE has chosen to ignore our important role and promote seemingly unworkable and for the most part clinically ineffective treatments”
Friday 29th May. NICE has had a good reputation in the USA for its important, and usually high-quality, attempts to assess what works and what doesn’t. That makes it all the sadder to see it condemned already from the USA for its latest effort. The excellent Yale neurologist, Steven Novella, has written about it on his Neurologica blog.
Friday 29th May. A correspondent points out that the costings of the guidance can be found on the NICE web site. Table 1 has a strong air of make-believe.

The Daily Mail (29 May 2009). Their article quotes serious criticisms of NICE.
Dr Ron Cooper, past chairman of the group and a consultant pain specialist in Northern Ireland, said: ‘I have never known so many pain medicine specialists to be so furious. More patients will end up having more expensive surgery, which is unnecessary, risky and has worse results.
‘NICE made it difficult for us to submit evidence to a committee on which there was not one experienced pain physician.
‘The guidelines will make us the laughing stock of Europe, Australia and the U.S. where pain specialists will continue to have full access to a wide range of treatments.’
Chirowatch suspended. 30 May 2009. The invaluable chiro-watch site, http://www.chirowatch.com, run by Dr Canadian physician, Dr Tom Polevoy, has been “suspended”. In fact the whole of his domain, healthwatcher.net, has been disabled. It seems that this was the result of a legal threat to his ISP, not by chiropractors this time, but by William O’Neill of the Canadian Cancer Research Group, which is far from being what the respectable-sounding title suggests, according to Dr Stephen Barrett. The site will be back soon, I’m told. Meanwhile you can read the suspended page here, and the only result of their hamfisted bullying will be to vastly increase the number of people who read it. You can read lots more at Quackwatch’s chirobase and at ebm-first.
A new blog, Not as NICE as you think appeared on May 30th. It is written by a pain physician, Stephen Ward. and is devoted to pointing out the serious problems raised by NICE’s guidance. It starts with the (very critical) World Institute of Pain Press Release.
British Medical Journal has more flak for the NICE guidelines
And the BMJ has published a letter signed by 50 consultants in pain medicine, NICE guidelines on low back pain are flawed.(this will probably appear as a letter in the print edition of the BMJ).









